FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
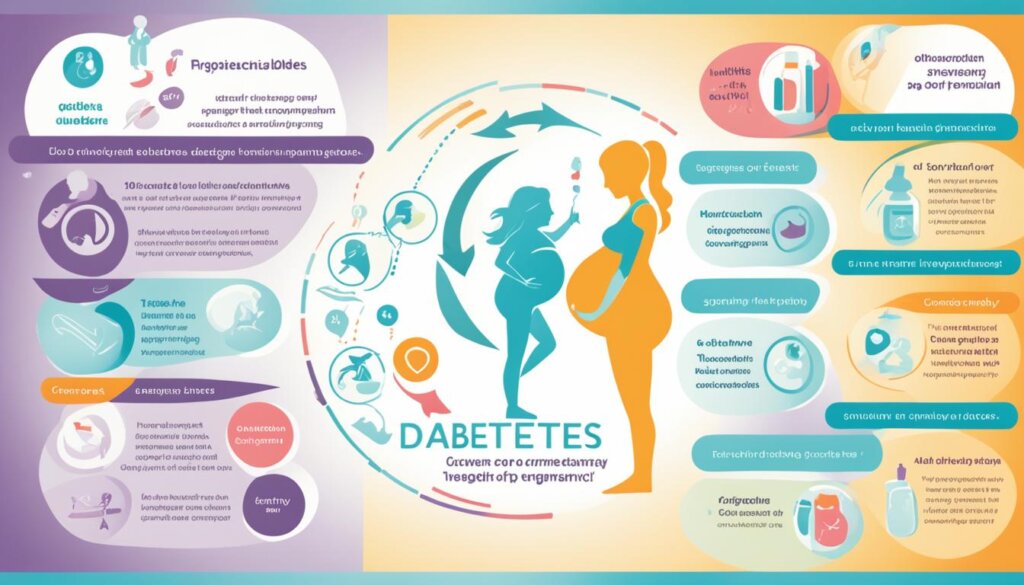
Women with diabetes during pregnancy face many challenges. High blood sugar can harm the baby early on. It can also lead to premature birth, big babies, breathing issues, and low blood sugar in newborns. High blood sugar can even cause miscarriage or stillbirth.
Diabetes also raises the risk of preeclampsia in pregnant women. It’s vital to keep blood sugar in check. Regular prenatal care and a healthy lifestyle are key for a safe pregnancy.
Key Takeaways
- Diabetes during pregnancy can pose significant risks to both the mother and baby if not properly managed.
- High blood glucose levels can increase the chances of birth defects, premature birth, and other complications.
- Regular monitoring of blood sugar levels and adjustments to insulin therapy are crucial throughout the pregnancy.
- Adopting a healthy lifestyle, including a balanced diet and regular exercise, can help prevent gestational diabetes and manage blood sugar levels.
- Comprehensive prenatal care and planning are essential for women with diabetes who are pregnant or planning a pregnancy.
Understanding Diabetes and Pregnancy
Pregnancy can be tough for women with diabetes, whether it’s type 1 or type 2 diabetes or gestational diabetes. It’s important to know about the risks and complications. This knowledge helps ensure a healthy pregnancy and delivery.
Types of Diabetes in Pregnancy
There are two main types of diabetes that can happen during pregnancy:
- Preexisting diabetes – This is type 1 or type 2 diabetes a woman has before pregnancy. Keeping blood sugar levels in check is key to avoiding complications.
- Gestational diabetes – This type of diabetes starts during pregnancy and usually goes away after the baby is born. But, women with gestational diabetes are more likely to get type 2 diabetes later.
Potential Risks and Complications
Both preexisting and gestational diabetes can lead to pregnancy problems if not managed well. These include:
- Birth defects and stillbirth – High blood sugar before conception can harm the baby’s health.
- Excessive fetal growth and high birth weight – High blood sugar during pregnancy can make the baby too big. This can make delivery harder and increase the risk of obesity and type 2 diabetes later.
- Preterm birth – Women with diabetes are more likely to have a baby too early.
- Cesarean delivery – Diabetes raises the chance of needing a C-section.
Managing blood sugar levels is key. This can be done through diet, exercise, and medicine if needed. Doing this helps lower risks and ensures the best outcomes for mom and baby.
Managing Blood Sugar During Pregnancy
Keeping your blood sugar levels healthy is key during pregnancy. Your healthcare team will watch your target blood glucose levels closely. They might be different from before you were pregnant. You’ll need to test your blood sugar levels often, sometimes more than once a day.
Target Blood Glucose Levels
If you have diabetes before getting pregnant, your blood sugar targets are specific. They are: 60-99 mg/dl before meals and at bedtime, 100-129 mg/dl after meals and less than 6% for A1C. Keeping your blood glucose levels in this range is important for a healthy pregnancy and to lower the risk of problems.
Blood Glucose Testing and Monitoring
Women with diabetes during pregnancy might need to test their blood glucose up to eight times a day. Insulin therapy, changing your diet, and staying active are ways to manage your blood sugar during pregnancy.
A good serving size for starchy foods is 1 cup of cooked rice or pasta or 2 slices of bread. Drinking only one 8-ounce cup of milk at a time can help keep your blood sugar levels stable. For fruit, have one small piece or half a big one, or 1 cup of mixed fruit, to avoid high blood sugar.
Whole grain foods like whole grain bread and brown rice help keep your blood sugar levels low. Choosing whole grains for breakfast is good for blood sugar control. It’s best to pair them with a protein source for a stable blood sugar level in the morning.
Avoid fruit juices and sugary drinks because they raise blood sugar levels quickly. Sweets and desserts are also bad for your blood sugar because they have a lot of sugar and aren’t very nutritious.
Artificial sweeteners like aspartame are safe during pregnancy as sugar substitutes. But be careful with sugar-alcohols in sugar-free foods because they can affect your blood sugar levels like sugar does. Some sugar alcohols can cause stomach issues like gas and bloating.
Staying active is good for pregnant women with diabetes. You can do walking, low-impact aerobics, swimming, or water aerobics. Avoid hard exercises if you have certain health issues like high blood pressure.
Preparing for Pregnancy with Diabetes
If you have diabetes before getting pregnant, it’s very important to prepare. Work closely with your healthcare team to control your blood sugar before trying for a baby. This means regular check-ups, changing your meds if needed, and taking supplements like high-dose folic acid (5mg) before and during the first 12 weeks of pregnancy.
Preconception Care and Checkups
Getting your blood sugar under control before pregnancy lowers the risk of problems. The American Diabetes Association says to keep HbA1c levels below 48mmol/mol for a safe pregnancy. You’ll also need eye and kidney tests before trying for a baby. These tests are important because pregnancy can make eye and kidney problems worse.
Diabetes Management Plan
Creating a good diabetes management plan is key. This means checking your blood sugar, changing your meds if needed, and eating well and exercising regularly. Women with diabetes should avoid some sports and heavy lifting during pregnancy to stay safe.
By doing these things, people with diabetes before pregnancy can have a healthier pregnancy. This lowers the risk of problems for both mom and baby.
Diabetes and Pregnancy: What You Need to Know
Pregnancy with diabetes can be tough, but you can have a healthy pregnancy and baby with the right steps and help from doctors. If you have diabetes before pregnancy or get it during, knowing what to do is key.
Keeping your blood sugar in check is very important. Women with diabetes might have bigger babies, harder births, and need more help during labor. They also might get eye and kidney problems or a serious condition called diabetic ketoacidosis.
Getting ready for pregnancy with diabetes is a must. This means a health check before pregnancy, changing your insulin or medicine, and watching your blood sugar closely. Working with a team of doctors, including an obstetrician, endocrinologist, and dietitian, helps keep you and your baby healthy.
During pregnancy, you might face issues like miscarriage, pre-eclampsia, or needing help during labor. But, with careful management and watching the baby, these risks can be lowered.
After the baby comes, taking care of yourself and breastfeeding is important. You might need less insulin, and it’s still key to watch your blood sugar closely after giving birth. A check-up at 6 weeks after birth is a good idea to make sure you’re doing well and plan for the future.
Dealing with diabetes and pregnancy means understanding the risks, how to manage them, and getting special care. By working with your healthcare team and making smart choices, you can have a healthy pregnancy and a happy baby.

“With proper management and close collaboration with the healthcare team, individuals with diabetes can have a healthy pregnancy and baby.”
Healthy Lifestyle for Gestational Diabetes
For those with gestational diabetes, a healthy lifestyle is key. It helps manage the condition and keeps mom and baby healthy. Eating a balanced diet and staying active are important steps. They help control blood sugar and support the baby’s growth.
Dietary Recommendations
Managing gestational diabetes means eating foods that keep blood sugar stable. You should eat less sugar and more complex carbs, lean proteins, and healthy fats. Try to get less than half of your calories from carbs, and balance the rest with protein, fiber, and healthy fats.
- Aim for 6 or more servings of grains, beans, and starchy vegetables per day.
- Consume 3 to 5 servings of vegetables daily.
- Enjoy 2 to 4 servings of fruits per day.
- Incorporate 4 servings of low-fat or non-fat dairy products into your diet.
- Aim for 2 to 3 servings of protein sources per day.
- Limit your intake of fatty and saturated foods.
Exercise During Pregnancy
Exercise is great for those with gestational diabetes. It keeps blood sugar in check, makes insulin work better, and boosts health for mom and baby. Always talk to your doctor to find the right exercise plan for you during pregnancy.
“The management of diabetes in pregnancy adheres to standards of care, with a focus on optimizing maternal and fetal health.”
By changing your lifestyle, you can better manage gestational diabetes and lower the risk of problems. These changes help both mom and baby stay healthy during pregnancy.
Potential Complications for Mother and Baby
Diabetes during pregnancy can lead to serious issues for both mom and baby. For moms, it might cause high blood pressure, preeclampsia, and the need for a C-section. Babies could face problems like being too heavy, having trouble breathing, low blood sugar, obesity, and a higher chance of getting type 2 diabetes later. It’s key to watch closely and act fast to stop these problems.
High blood sugar can make labor start early and might mean a C-section is needed. Babies of moms with gestational diabetes might be more likely to be overweight or obese and could get type 2 diabetes later. If diabetes is not managed well, there’s a small chance the baby could have jaundice or face serious risks at birth.
Studies show kids of moms with gestational diabetes might face a higher risk of getting type 2 diabetes or obesity as adults. Women with gestational diabetes might give birth earlier than others, affecting the timing. Even with good diabetes control, some moms might need to deliver early to protect their babies.
For gestational diabetes, keeping blood sugar in check is crucial. Goals include levels of 95 mg/dL before eating, 140 mg/dL an hour after eating, and 120 mg/dL two hours after eating. Not controlling glucose can raise the risk of miscarriage and stillbirth. Every pregnancy has a small chance of birth defects, but gestational diabetes doesn’t usually increase this risk.
High blood sugar during pregnancy can lead to serious issues like pre-eclampsia, too much amniotic fluid, early delivery, big babies, and health problems for newborns. Babies of parents with gestational diabetes might be more likely to get diabetes later.
But, gestational diabetes doesn’t seem to affect a child’s behavior or learning. For most, gestational diabetes goes away after giving birth, but some might turn into type 2 diabetes.
We need more research on how gestational diabetes affects the brain later in life. Doctors check for gestational diabetes around 24 to 28 weeks with a glucose test, and more tests if needed.
If you had gestational diabetes before, you’re more likely to have it again in future pregnancies. Breastfeeding is good, but moms with diabetes must keep their sugar levels under control to protect their babies.
Labor and Delivery Considerations
People with diabetes, including gestational diabetes, need special care during labor and delivery. They must watch their blood sugar closely and adjust insulin therapy as needed. This ensures the safety of both the mom and the baby. The healthcare team will help create a plan for managing diabetes during this time.
Labor might start early for some to prevent problems. Keeping an eye on blood sugar levels is key during labor and delivery. Adjusting insulin therapy is important to keep blood sugar right and avoid too high or too low levels.
The choice between vaginal or cesarean delivery matters for those with diabetes and pregnancy. The baby’s size, blood sugar control, and any complications affect the decision. The healthcare team will help pick the safest delivery option.
Good planning and teamwork between the patient and healthcare team are key to a safe birth for those with diabetes and pregnancy. By managing blood sugar, watching the baby, and making smart decisions, risks can be lowered. This keeps the focus on the health of the mom and baby.
Recommendation | Description |
|---|---|
Inducing Labor | Individuals with diabetes may need to have their labor induced earlier than the due date to help prevent complications. |
Continuous Glucose Monitoring | Frequent blood sugar checks and continuous glucose monitoring are essential to maintain optimal blood sugar levels during labor and delivery. |
Insulin Therapy Adjustments | Insulin therapy may need to be adjusted to keep blood sugar within the target range and avoid both hyperglycemia and hypoglycemia. |
Mode of Delivery | The decision for vaginal or cesarean delivery is based on factors such as the size of the baby, the mother’s blood sugar control, and the presence of any complications. |
Working with the healthcare team and following a detailed plan helps people with diabetes have a safe and positive birth. This ensures the best outcomes for both the mom and the baby.
Postpartum Care and Follow-up
After your baby comes, taking care of yourself is key. Keeping an eye on your blood sugar is very important. This is because your body’s insulin needs change after having a baby. If you had gestational diabetes during pregnancy, you’re more likely to get type 2 diabetes later. So, it’s important to check in regularly and get screened to stop or slow down this condition.
Blood Glucose Monitoring After Birth
Checking your blood sugar after having a baby is crucial. Your doctor will help you make a plan to keep an eye on your blood sugar and manage your diabetes. This might mean checking your blood sugar often, changing your meds or insulin, and living a healthy life to help you recover and stay healthy.
The American College of Obstetricians and Gynecologists (ACOG) makes sure we have the latest info on caring for new moms. They say all women should see their healthcare providers within three weeks after giving birth. They also suggest a full check-up by 12 weeks after the baby is born.
Women with ongoing health issues, like diabetes, need to see their doctors regularly for care. This shows how important it is to keep up with your diabetes care and go to your postpartum appointments. It helps you stay healthy and adjust well after having a baby.

Some women might not go to their postpartum check-ups, and some groups might not go as often. To help, doctors talk about postpartum care during pregnancy visits. They use peer counselors and tech to remind you to come in. They also push for paid sick days and family leave to make it easier to take care of yourself after having a baby.
Being active in your postpartum care helps you keep your blood sugar in check. It supports your health and lowers your risk of getting type 2 diabetes later.
Breastfeeding with Diabetes
Breastfeeding is key for moms with diabetes during postpartum care. It’s important to watch blood sugar levels closely. The healthcare team can help manage insulin, diet, and breastfeeding for everyone’s health.
Studies say breastfeeding lowers diabetes risk for moms with gestational diabetes. Babies who get formula are more likely to get diabetes than those breastfed. Moms with diabetes might take longer to start making milk.
To help with breastfeeding and keep the baby’s blood sugar stable, moms should nurse every hour in the first few hours. Skin-to-skin contact, or kangaroo care, helps the baby’s heart and breathing. It also helps with breastfeeding.
Most diabetes medicines, like insulin and metformin, are safe for breastfeeding. Breastfeeding for over two months cuts the risk of type 2 diabetes almost in half. Breastfeeding for more than five months lowers the risk even more.
An Infant Feeding Advisor at the hospital can offer great support and info for diabetic moms. With help from their healthcare team, moms with diabetes can overcome breastfeeding challenges. This ensures the best outcomes for moms and babies.
Long-term Risks and Prevention
Women who have gestational diabetes are more likely to get type 2 diabetes later. It’s key to watch your health closely and live a healthy life to stop or slow type 2 diabetes. Those with gestational diabetes are three times more likely to have metabolic syndrome than others. This shows the need to take steps to keep their health in check.
Gestational diabetes can lead to more heart problems and cancer later on. Babies born to mothers with gestational diabetes might face a higher chance of having trouble with sugar levels and being overweight as kids. Being exposed to diabetes in the womb can also make kids more likely to get type 2 diabetes and be overweight later.
To lower these risks, people with gestational diabetes should act early. Eating right, staying active, and keeping a healthy weight are key steps. Checking your health often and acting quickly can stop or slow type 2 diabetes and other health issues.
Long-term Risks | Prevalence |
|---|---|
Type 2 Diabetes | Increased risk compared to the general population |
Metabolic Syndrome | 3-fold higher prevalence |
Cardiovascular Morbidity | Increased risk |
Female Malignancies | Increased risk |
Childhood Obesity and Impaired Glucose Tolerance | Increased risk in offspring |
By being proactive, people with gestational diabetes can lessen their health risks and aim for a healthier life.

“Early detection and management of gestational diabetes are crucial for maternal and fetal health.”
Resources and Support for Diabetes in Pregnancy
Managing diabetes during pregnancy is tough. But, there are many resources and support options to help.
Working with a healthcare team that knows about diabetes and pregnancy is key. Doctors, obstetricians, nurse educators, and dietitians offer great advice and help. They help manage gestational diabetes for a healthy pregnancy and birth.
Educational materials and support groups are also great. They give info on controlling blood sugar, what to eat, and how to handle diabetes during pregnancy’s challenges.
Using these resources and support makes people with diabetes feel strong and ready for a healthy pregnancy and birth.
The Woman’s Hospital of Texas has special classes and support for those with diabetes. They offer Perinatal Diabetes Management Classes, Preconception Counseling, Diabetes in Pregnancy classes, and Postpartum and Breastfeeding support. These programs give full education and help for managing diabetes before, during, and after pregnancy.
The hospital’s Education Department has free support groups and talks on diabetes support and health education. They have Registered Dietitians for nutrition advice before pregnancy, during pregnancy, and for diabetes management.
With these wide-ranging resources and support, people with diabetes in pregnancy can feel empowered, informed, and ready to face this journey. They can aim for the best health outcomes for themselves and their babies.,
Conclusion
Managing diabetes and pregnancy needs a full plan, working with doctors, and caring for your health. If you have preexisting diabetes or get gestational diabetes, it’s key to know the types, check blood sugar levels, and follow prenatal care tips.
Start by getting ready for pregnancy, living a healthy lifestyle, and dealing with possible complications. This helps people with diabetes have a good pregnancy and birth. Also, postpartum care and watching for long-term health risks, like type 2 diabetes, are key to staying healthy.
With the right info, support, and help from your healthcare team, you can feel sure and happy during this time. This article gives you the tools and advice to manage your health. It helps you have a happy and rewarding pregnancy.
FAQ
What are the different types of diabetes that can occur during pregnancy?
There are two main types of diabetes that can happen during pregnancy. These are preexisting diabetes (type 1 or type 2) and gestational diabetes. Gestational diabetes starts during pregnancy.
How can diabetes affect the mother and the baby during pregnancy?
Diabetes can affect both the mother and the baby during pregnancy. It can lead to birth defects, preterm birth, and other issues for the baby. For the mother, it may cause high blood pressure, preeclampsia, and the need for a C-section.
What are the key strategies for managing blood sugar during pregnancy?
Keeping blood sugar levels healthy is key during pregnancy. This means testing blood glucose often, using insulin if needed, eating right, and staying active. These steps help keep blood sugar in a safe range.
What should individuals with preexisting diabetes do to prepare for pregnancy?
If you have preexisting diabetes, talk to your healthcare team to get your blood sugar under control before pregnancy. You’ll need regular check-ups, might need to adjust your meds, and take folic acid. Creating a good diabetes plan is also important.
What lifestyle changes are important for individuals with gestational diabetes?
If you have gestational diabetes, eating right and staying active are key. You should eat foods that help control your blood sugar and support your baby’s growth. Your healthcare team will tell you how much exercise is good for you.
What are the potential complications during labor and delivery for individuals with diabetes?
Women with diabetes might need special care during labor and delivery. This includes inducing labor early, watching blood sugar levels closely, and adjusting insulin therapy as needed. This ensures the safety of both the mother and the baby.
What should individuals with diabetes consider in terms of postpartum care and follow-up?
After the baby is born, it’s important to keep an eye on your blood glucose levels. Your insulin needs might change after giving birth. Breastfeeding with diabetes needs extra care. Women who have gestational diabetes are at higher risk of type 2 diabetes later. Regular check-ups and screenings are key.
How can individuals with a history of gestational diabetes prevent or delay the onset of type 2 diabetes?
If you’ve had gestational diabetes, you’re at higher risk of getting type 2 diabetes later. Regular check-ups and a healthy lifestyle can help prevent or delay type 2 diabetes. This includes eating right, exercising regularly, and keeping a healthy weight.
What resources and support are available for individuals with diabetes during pregnancy?
There are many resources and support options for managing diabetes during pregnancy. You can work with a healthcare team that knows about diabetes and pregnancy. There are educational materials and support groups for guidance and emotional support.