FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Did you know that out of every 1,000 pregnancies in the United States, one is a molar pregnancy? This is a rare complication where abnormal cells grow instead of a normal placenta. It’s crucial to know about molar pregnancies, their causes, symptoms, and treatments. In this guide, we’ll dive into the details of this unique pregnancy condition. We aim to give you the knowledge to handle this tough situation.
Key Takeaways
- Molar pregnancy is a rare complication where abnormal cells grow instead of a normal placenta.
- There are two main types of molar pregnancy: complete and partial.
- Molar pregnancies can lead to serious complications, including a rare form of cancer called choriocarcinoma.
- Symptoms can include vaginal bleeding, nausea, vomiting, and high levels of the hormone hCG.
- Treatment often involves a procedure called dilation and curettage (D&C) or medication to remove the abnormal tissue.
What is a Molar Pregnancy?
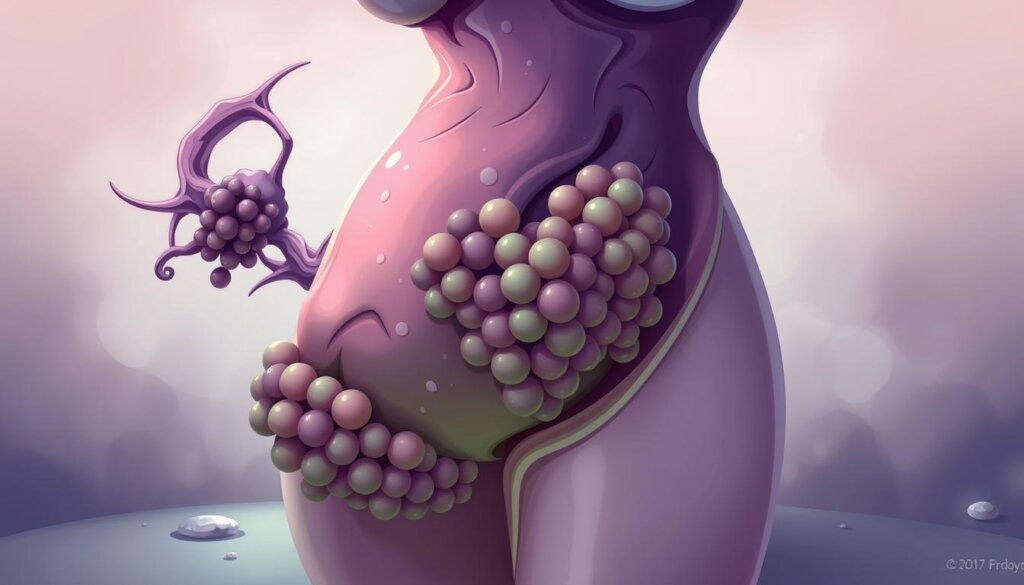
A molar pregnancy is when the placenta grows wrong without a healthy baby. It’s a rare issue that can be either complete or partial. Both types are unusual and need special care.
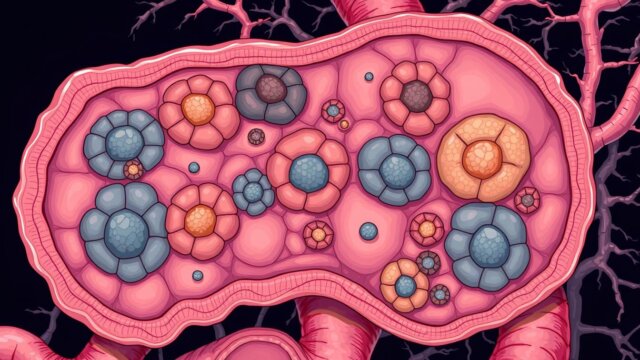
Types of Molar Pregnancy
In a complete molar pregnancy, the placenta gets very big and looks like fluid-filled cysts. There’s no baby in this case. On the other hand, a partial molar pregnancy has a placenta with both normal and abnormal tissue. There might be a baby, but it can’t live.
Abnormal Placental Growth
The growth problem in molar pregnancies comes from genetic mistakes during fertilization. These mistakes cause the placenta to grow wrong instead of a healthy baby. Molar pregnancies are rare, happening in about 1 in 1,200 pregnancies. They are more common in Asian women than in others.
Molar Pregnancy Type | Characteristics |
|---|---|
Complete Molar Pregnancy | – No fetus present – Placental tissue swells, appearing as fluid-filled cysts |
Partial Molar Pregnancy | – Presence of a fetus, but it cannot survive – Placenta has both regular and irregular tissue |
Molar pregnancies are often found early through ultrasounds or when tissue is checked after a miscarriage. Even though they’re rare, doctors need to know the signs to diagnose and treat them quickly.
Symptoms of Molar Pregnancy
Molar pregnancy can seem like a normal pregnancy at first. But, it has specific symptoms. Early signs may include dark brown to bright red vaginal bleeding, severe nausea and vomiting, and passing of grape-like cysts. If not caught early, symptoms can worsen, including a fast-growing uterus, preeclampsia before 20 weeks, ovarian cysts, and an overactive thyroid. It’s important to see a doctor quickly for any unusual pregnancy symptoms.
Early Signs and Symptoms
One common early sign is vaginal bleeding, starting between weeks 6 and 12. This bleeding can be dark brown to bright red. Molar pregnancies also cause severe nausea and vomiting, more intense than usual. Some women may also pass grape-like cysts from the vagina, a sign of molar pregnancy.
Later Signs and Symptoms
If a molar pregnancy is not caught early, symptoms can get worse. The uterus may grow larger than expected for the pregnancy stage. Pre-eclampsia, a condition with high blood pressure and organ damage, can happen much earlier than usual. Also, ovarian cysts and hyperthyroidism, or an overactive thyroid, can develop. These signs show why it’s crucial to get medical help quickly for any unusual pregnancy symptoms.

Molar pregnancies are rare, happening by chance. They can be detected during the 1st pregnancy ultrasound scan at around 8 to 14 weeks. The pregnancy hormone hCG levels are usually higher than normal. Molar pregnancies are more common in young teenagers or women over 45, those with an Asian background, and those who have had a molar pregnancy before.
“Recovering from a molar pregnancy can take time both physically and emotionally, and support services are available through specialists and organizations like Molar Pregnancy Support & Information, Miscarriage Association, and Tommy’s.”
It’s vital to seek medical help quickly for any unusual pregnancy symptoms. Early detection and proper management are key for the mother’s health and resolving the molar pregnancy.
Causes and Risk Factors
Molar pregnancies often come from genetic problems during fertilization. In a complete molar pregnancy, the egg lacks chromosomes, and the placental tissue is formed solely from the father’s genetic material. In a partial molar pregnancy, there is an extra set of paternal chromosomes.
Several risk factors increase the chance of molar pregnancy. These include a history of molar pregnancy, being over 43 or under 15, and fertility issues. Women who’ve had a molar pregnancy before are 6 times more likely to have another. Those with more than two molar pregnancies are 120 times more likely.
Genetics also play a big role. Certain genes like NLRP7 and KHDC3L are linked to molar pregnancy risk. Women of Asian descent are more likely to have molar pregnancies.
Workplace conditions and environmental factors can also affect molar pregnancy risk. A study in Iran found a link between physical jobs and molar pregnancy risk.
In summary, molar pregnancy is caused by genetic issues, past molar pregnancies, age, fertility problems, and work or environmental exposures. Knowing these factors helps doctors spot risks and take steps to prevent them.
Molar Pregnancy Diagnosis
Healthcare providers use ultrasound imaging and blood tests to find molar pregnancies. They check human chorionic gonadotropin (hCG) levels, a hormone seen in pregnancy.
Ultrasound scans show a mass of cysts instead of a normal placenta. They also find no or an abnormal fetus. A partial molar pregnancy might show a small fetus, low amniotic fluid, and a strange placenta.
Tests like CT scans or MRI might be needed. They check if the abnormal tissue has spread. These tests help doctors plan the best treatment.
High hCG levels are a sign of a molar pregnancy. Doctors keep watching hCG levels after removing molar tissue. This is because high levels might need more treatment.

Doctors use ultrasound images and hCG blood tests to diagnose molar pregnancies. This helps them create a treatment plan for this special condition.
Management and Treatment Options
For molar pregnancy, the main goal is to remove the bad placental tissue. This is usually done with a D&C procedure. The cervix is opened, and the uterine contents are sucked out. Sometimes, removing the uterus (hysterectomy) is suggested. This is if the patient doesn’t want more kids or if there are risks for GTN.
Dilation and Curettage (D&C)
The D&C is the most common treatment for molar pregnancy. The cervix is slowly opened. Then, the bad placental tissue is removed with a suction device or a spoon-shaped tool. This is done under anesthesia and followed by close monitoring.
Medication for Pregnancy Termination
Medications can also be used to make the uterus contract and push out the molar tissue. This method is less common but can work well. The choice between D&C and medication depends on the patient’s situation and the doctor’s preference.
After treatment, it’s important to keep a close eye on the patient. This ensures all molar tissue is gone and catches any signs of disease. Patients are told to use birth control and wait a while before trying to get pregnant again. This helps lower the risk of GTN after molar pregnancy.
In short, treating molar pregnancy involves both surgery and medicine. It’s key to watch the patient closely after treatment. This helps make sure the molar pregnancy is fully treated and prevents any future problems.
Complications of Molar Pregnancy
Molar pregnancies are rare, happening in about one in 1,000 pregnancies. Even after removing the abnormal tissue, some complications can still occur. One major worry is persistent gestational trophoblastic neoplasia (GTN). This happens when some molar tissue stays and grows, needing more treatment, like chemotherapy.
In 15% to 20% of cases, the trophoblastic tissue turns invasive or cancerous, leading to GTN. Choriocarcinoma is a fast-growing cancer that can spread to other organs.
Persistent Gestational Trophoblastic Neoplasia (GTN)
Persistent GTN occurs when some abnormal molar tissue stays and grows after initial treatment. It needs close watching and might need more chemotherapy to get rid of it.
Choriocarcinoma
Choriocarcinoma is a rare but serious issue from molar pregnancy. It’s a cancerous tumor from abnormal trophoblastic cells. This cancer can spread to places like the lungs and needs quick treatment, usually with chemotherapy. Even though it’s serious, choriocarcinoma often responds well to chemotherapy. Early detection and treatment usually have a good outcome.
It’s key to quickly find and treat abnormal vaginal bleeding after pregnancy, especially with pelvic pressure and nausea. Molar pregnancies don’t lead to a baby.
New research is looking into treatments like immunotherapy for choriocarcinoma. Patients getting cancer treatment can also get help to preserve fertility. This support is for healthy pregnancy and childbirth after treatment.
Complication | Frequency | Treatment |
|---|---|---|
Persistent GTN | 15-20% of molar pregnancies | Chemotherapy |
Choriocarcinoma | Rare but serious | Chemotherapy, potentially immunotherapy |
“The outlook for most types of choriocarcinoma is positive with successful treatment.”
Molar Pregnancy and Fertility
If you’ve had a molar pregnancy, you might wonder about your future fertility. A molar pregnancy itself doesn’t cause infertility. Doctors suggest waiting 6 months to 1 year before trying again. This time, let’s ensure all bad tissue is gone and hormone levels are back to normal.
After a molar pregnancy, you might need more checks during future pregnancies. But, the risk of another molar pregnancy is low. Only about 1% of women (1 out of 100) have another one.
Women who get chemotherapy for GTD after a molar pregnancy face some challenges. They might start menopause 3 years early. Women over 45 who get chemotherapy might not get their periods back and could go through early menopause.
Even with these challenges, the chance of having a healthy baby after chemotherapy is the same as for any woman of the same age. The risk of a baby with problems is also the same as for women without GTD.
If you’re thinking about getting pregnant again after a molar pregnancy or GTD treatment, wait at least a year after finishing chemotherapy. This lets your body heal and ensures the best outcome for your future pregnancy.
Remember, your fertility and ability to have healthy children aren’t forever changed by a molar pregnancy or GTD. With the right medical care and support, you can still have a successful pregnancy in the future.
Prevention and Future Pregnancy Planning
There’s no known way to prevent a molar pregnancy. But talking to your healthcare provider about future pregnancies is key if you’ve had one before. They might suggest early ultrasounds and close monitoring for any future pregnancies. This helps catch problems early.
People who’ve had a molar pregnancy should wait 6 to 12 months before trying again. This time lets any leftover tissue go away, and hCG levels get back to normal.
The chance of having another molar pregnancy is low. About 99% of women who’ve had one don’t have another, and future pregnancies are usually safe.
But, some things can raise your risk, like being over 43 or under 15. Talking about these with your doctor can help you plan your future pregnancies better.
If a molar pregnancy happens again, or if GTN persists, places like Charing Cross Hospital in London can help.
Being proactive and working with your healthcare team can help you plan a healthy future pregnancy. Keeping up with monitoring and talking openly with your doctor is crucial for a good outcome.
Molar Pregnancy: Causes, Symptoms, and Treatment
A molar pregnancy is a rare but serious issue in early pregnancy. It happens when the placenta grows abnormally, leading to a gestational trophoblastic disease called a hydatidiform mole. If not treated, it can cause pregnancy loss or even rare cancers.
It’s important to know the signs of a molar pregnancy. Early signs include bleeding, grape-like cysts, nausea, vomiting, and pelvic pain. As it gets worse, the uterus may grow too big, and you might face other problems like high blood pressure.
The exact cause of molar pregnancy is still a mystery. But it’s thought to be linked to genetic issues causing abnormal placental growth. Older age, a history of molar pregnancies, and a diet lacking carotene might increase your risk.
To diagnose a molar pregnancy, doctors use ultrasound imaging and blood tests to measure hCG levels. The main treatment is a dilation and curettage (D&C) procedure to remove the bad tissue. Afterward, they watch hCG levels closely to make sure all tissue is gone and to prevent cancer.
If cancer does develop, chemotherapy treatment might be needed. Though it’s tough, most people can still have healthy pregnancies later. It’s wise to wait 6 to 12 months before trying again.
Knowing about molar pregnancy is key to staying healthy. With quick medical help and the right care, most people can have a healthy future.
Conclusion
Molar pregnancy is rare but very important for pregnant people and doctors. Knowing the causes, like genetic problems, helps. Also, being aware of symptoms, like abnormal growth, is key.
Early signs and later problems, like persistent growth, need quick action. This way, people can watch their health closely and get help fast.
Getting a quick diagnosis and right treatment, like surgery or medicine, is good. It shows that future pregnancies can be healthy. This is why keeping fertility in mind and planning carefully is so important.
Doctors can keep getting better at handling molar pregnancy by staying up-to-date. Knowing all about molar pregnancy helps ensure the best health for everyone.
FAQ
What is a molar pregnancy?
A molar pregnancy is a rare issue during pregnancy. It happens when cells called trophoblasts grow too much. This leads to a mass or tumor in the uterus instead of a normal placenta.
What are the types of molar pregnancy?
There are two main types. A complete molar pregnancy has no fetus and swollen placental tissue. A partial molar pregnancy has an abnormal placenta and a fetus that can’t survive.
What are the symptoms of a molar pregnancy?
Early signs include dark brown to bright red vaginal bleeding. You might also feel severe nausea and vomiting. Passing grape-like cysts is another symptom.
Later, you might notice a uterus growing fast. You could also get preeclampsia before 20 weeks. Ovarian cysts and an overactive thyroid are other signs.
What causes a molar pregnancy?
Genetic problems during fertilization cause molar pregnancies. In a complete molar, the egg lacks chromosomes. The placental tissue comes from the father’s genetic material.
In a partial molar, there’s an extra set of paternal chromosomes.
How is a molar pregnancy diagnosed?
Doctors often find molar pregnancies through ultrasound or blood tests. These tests show high levels of the pregnancy hormone hCG. Ultrasound can spot a mass of cysts instead of a normal placenta.
It can also show if a fetus is missing or growing abnormally.
How is a molar pregnancy treated?
The main treatment is removing the abnormal placental tissue. This is usually done through a procedure called dilation and curettage (D&C). Medication might be used to help the uterus contract and expel the contents.
In some cases, a hysterectomy might be recommended.
What are the potential complications of a molar pregnancy?
Even after treatment, complications can still happen. Persistent GTN can occur if some tissue remains. This requires more treatment, like chemotherapy.
Rarely a cancerous form called choriocarcinoma can develop. It can spread to other organs.
How does a molar pregnancy affect fertility?
A molar pregnancy itself doesn’t cause infertility. However, doctors might suggest waiting 6 months to 1 year before trying to conceive again. This ensures all abnormal tissue is removed and hormone levels are normal.
During future pregnancies, extra monitoring is done to catch any molar pregnancy issues early.
How can I prevent a molar pregnancy?
There’s no known way to prevent a molar pregnancy. But if you’ve had one before, talk to your healthcare provider about future pregnancies. They might suggest early ultrasounds and close monitoring to catch issues early.


![14 Effective Home Remedies for Cough [Ultimate Guide]](https://healthyious.com/wp-content/uploads/2020/01/14-Effective-Home-Remedies-for-Cough-Ultimate-Guide-640x360.jpg)