FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Inflammatory heart disease is a type of heart disease caused by heart inflammation. The most common form of inflammatory heart disease is coronary artery disease, caused by the buildup of plaque in the arteries that supply blood to the heart.
Other forms of inflammatory heart disease include myocarditis, endocarditis, and pericarditis.
Inflammatory heart disease is a leading cause of death in the United States. According to the Centers for Disease Control and Prevention (CDC), about 600,000 people die from heart disease yearly in the United States. This includes about 370,000 deaths from coronary artery disease, the most common form of heart disease.
The exact cause of inflammatory heart disease is unknown, but it is thought to be related to genetic and environmental factors.
Inflammatory heart disease is more common in people with certain risk factors, such as smoking, high blood pressure, high cholesterol, diabetes, or a family history of heart disease.
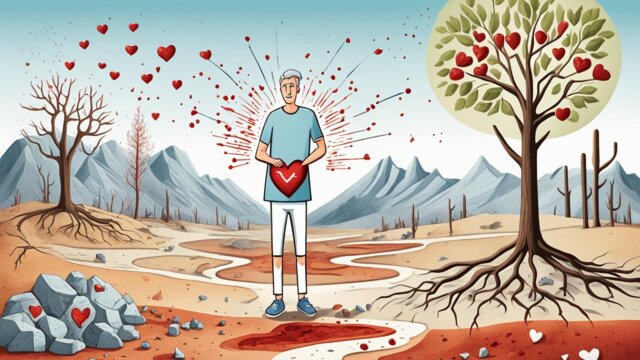
Treatment for inflammatory heart disease usually involves lifestyle changes and medical therapy.
Lifestyle changes that can help reduce the risk of developing heart disease include eating a healthy diet, maintaining a healthy weight, exercising regularly, and avoiding smoking.
Medical therapy for inflammatory heart disease may include aspirin, beta-blockers, statins, and other medications. In some cases, surgery may be necessary to treat heart disease.
What is Inflammatory Heart Disease?
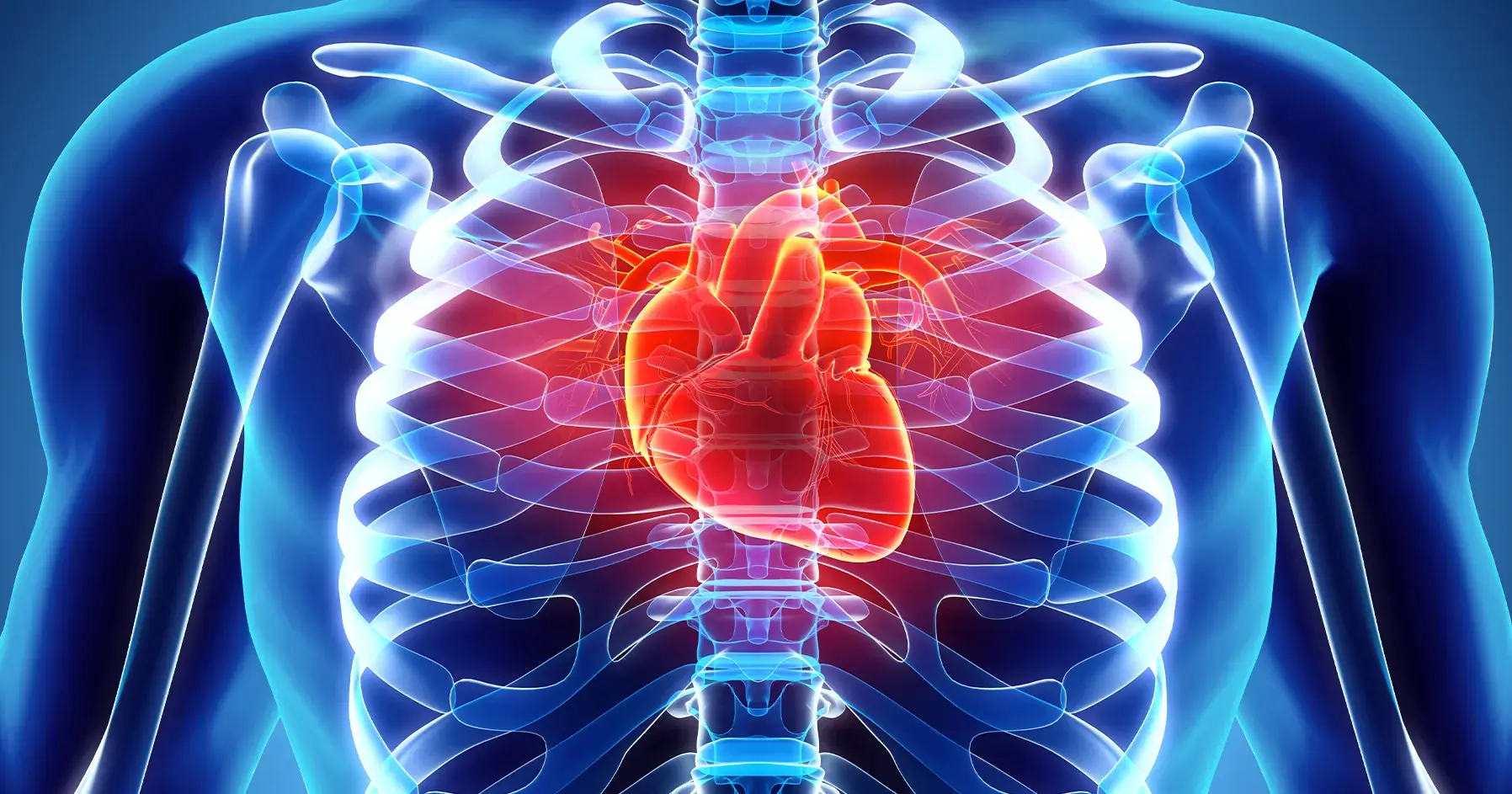
Inflammatory heart disease is a condition in which the heart becomes inflamed, often as a result of infection. The inflammation can cause the heart to beat faster and harder, leading to heart failure.
Inflammatory heart disease is most commonly caused by a virus, such as the flu or a respiratory virus. It can also be caused by bacteria, such as those that cause strep throat or tuberculosis. In some cases, inflammatory heart disease may be caused by a fungal infection.
Inflammatory heart disease can also be caused by autoimmune disorders, such as lupus or rheumatoid arthritis. In these disorders, the body’s immune system mistakenly attacks the heart tissue, causing inflammation.
Treatment for inflammatory heart disease often includes antibiotics to clear the infection and corticosteroids to reduce the inflammation. Surgery may sometimes be necessary to repair or remove damaged heart tissue.
If you think you may have inflammatory heart disease, it’s important to see your doctor immediately. Early diagnosis and treatment can help prevent the disease from progressing and causing serious complications.
Triggers of Inflammatory Heart Disease
Inflammatory heart disease develops when the surrounding heart tissue or muscle is subjected to inflammation from exposure to an infection like bacteria, virus, or internal irregularity.
This type of inflammation may occur in rheumatic fever and Kawasaki disease cases. The condition may be categorized as either endocarditis, myocarditis, or pericarditis.
Pericarditis
The heart is enclosed by a sac called the pericardium. The sac comprises two layers the fibrous pericardium and the serous pericardium.
The serous pericardium has two layers that lubricate the active heart to eliminate friction.
The fibrous pericardium is the outer layer of dense connective tissue that secures the heart to the bordering walls, prevents the excessive flooding of the heart with blood, and protects the heart.
There are many instances where pericarditis occurs without a known cause however there are some triggers that have been identified, including:
- Viral and bacterial infections
- Connective tissue diseases such as sarcoidosis and rheumatoid arthritis
- Previous injuries to the heart like heart attack, trauma, and heart surgery
- Metabolic disorders, most notably hypothyroidism and uremia (kidney failure)
- An adverse reaction to a specific type of medication
- Tumors and cancers
Symptoms
The primary symptom will be chest pain which is usually described as a sharp severe pain that may radiate from the chest area to the shoulder blades, neck, and back.
There may also be pain near the diaphragm that migrates to the back area. Upon deep inhalation, the chest pain will likely be exacerbated. It is also much worse when lying down and generally alleviated by slanting the body forward.
Pain may manifest upon swallowing if the inflammation is very close to the esophagus. It is also possible to experience a fever if an infection triggers pericarditis.
Diagnosing Pericarditis
To diagnose the disease, the doctor will assess the type of pain being experienced by the patient. The most obvious finding may be from a pericardial friction rub, a sound that will be heard when a stethoscope is applied to the chest area.
However, this is not always guaranteed to work because the rub is not constant.
An ECG electrocardiogram, chest x-ray, and heart ultrasound will be performed to ensure an accurate diagnosis.
A blood test may be performed to identify any other underlying conditions that may have prompted the pericarditis.
Treatments
The foremost treatment is the administering of anti-inflammatory medications.
Drugs like ibuprofen are used to decrease inflammation. A pain reliever in the form of narcotic pain medication may be prescribed.
Pericardiocentesis may be performed to remove excess fluid from the sac, or it may be used to identify the pathogen of origin that may have initiated the condition.
Endocarditis
Endocarditis is caused by an infection of the endocardium or inner lining of the heart resulting in subsequent inflammation.
It generally manifests when pathogens from other body areas enter the bloodstream and latch on to weakened areas of the heart.
If not treated, it may partially or completely ruin the heart valves and progress into a life-threatening condition.
The condition rarely affects individuals with healthy hearts. The greatest risk factor is having a damaged or artificial heart valve or other heart defects.
Symptoms
The development of endocarditis may be quite sudden or may be gradual in progression, dependent on the particular type of infection or an associated heart defect.
- Joint and muscle pain
- Fever and chills
- Heart murmurs (irregular sounds emanating from the heart)
- Persistent coughing
- Oedema (swelling) of the feet and abdomen
- Extreme tiredness or fatigue
- Night sweats
- Tenderness below the rib cage generated from the spleen
- A pale complexion
- Blood in the urine
- Visible purple or red spots in the mouth on the skin or the whites of the eyes
- Areas of red, tender spots beneath the skin of the fingers.
- Sudden weight loss
- Shortness of breath
Though these symptoms may resemble other non-critical conditions, it is still important to contact a doctor once a few are experienced, especially in another heart condition.
High-risk groups for developing the condition
- Individuals with artificial valves. Artificial valves are more likely to be attacked by pathogens, especially within the first year of valve implantation.
- Having a congenital birth defect means the heart is more prone to infection.
- Experiencing any prior damage to the heart valve will make developing the condition more likely.
- Intravenous drug users have a heightened chance of developing the condition because the shared needles are likely to be contaminated with bacteria that can trigger infection leading to this disease.
Diagnosis
- Blood tests will be performed to identify the source of bacterial infection.
- An echocardiogram will be used so the doctor can assess any damage to the valve.
- An ECG or electrocardiogram and x-ray will be used to assess the heart’s condition further.
- If the infection is thought to have affected other body areas, a CT computerized tomography or MRI magnetic resonance imaging scan will be performed.
Treatments
Treatment will often include antibiotics in less severe cases and surgery in instances where there is valve damage or persistent infection.
Myocarditis
Myocarditis refers to inflammation of the heart muscle. It is caused by several infections, including viruses like sarcoidosis, pregnancy, and immune diseases.
The most frequent infection is by a virus that attacks the heart muscle producing local inflammation. Once the infection is abated, the immune response will be perpetuated, lengthening the duration of the myocarditis.
Symptoms
It may sometimes be asymptomatic. The most typical system is a pain in the chest. In severe cases, the disease may result in the deterioration of the heart muscle.
Therefore, it is possible to cause heart failure with evident shortness of breath or difficulty breathing, Oedema, extreme tiredness, and so on.
Diagnosis
It will be identified by using conventional methods of diagnostics. ECG or electrocardiogram will be used to pinpoint irregularities within the heartbeat.
MRI or magnetic resonance imaging tests will detect heart muscle abnormalities.
Blood tests will be carried out to check for infection and possible elevation of heart muscle enzymes.
Prognosis
From the outset of the disease, it is unknown how well an individual will recover. Some persons recover completely, while others may develop chronic heart failure due to excessive damage to the heart muscles.
Rarely may an individual be afflicted with fulminant heart failure, which is lethal if a heart transplant is not performed. If the damage to the muscle is extreme, a defibrillator may be implanted to increase the heart’s overall efficiency.
The Bottom Line
If you have inflammatory heart disease, it is important to work with your healthcare team to create a treatment plan that is right for you.
With treatment, most people with inflammatory heart disease can live long and healthy lives.