FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Did you know that nearly 40% of people over 50 have colon polyps? These small growths on the colon lining are common. About 20% of adults have them. Knowing about colon polyps is key to a healthy gut and stopping colorectal cancer.
Key Takeaways
- Colon polyps are small growths on the lining of the colon or large intestine, affecting around 20% of adults overall and 40% of individuals over age 50.
- While most colon polyps are not cancerous, some can turn into colon cancer over time, making early detection and removal important.
- Certain risk factors, such as age, family history, obesity, and lifestyle habits like smoking and heavy alcohol consumption, can increase the likelihood of developing colon polyps.
- Regular screening through colonoscopy is recommended to identify and remove any precancerous polyps, reducing the risk of colorectal cancer.
- Adopting a healthy diet, staying physically active, and maintaining a healthy weight can help prevent the development of colon polyps and reduce the risk of colorectal cancer.
What are Colonic Polyps?
Colon polyps grow on the lining of the colon or large intestine. They are a type of tumor, made of abnormal cells. About 25 percent of men and women over 45 have them. Polyps come in different shapes and types.
Types of Colonic Polyps
Colon polyps are divided by shape and growth. Pedunculated polyps have a “head” and “stalk.” Sessile polyps stick directly to the colon wall. They grow in two ways: flat and with a stalk.
Neoplastic vs. Non-Neoplastic Polyps
Polyps are also split into neoplastic and non-neoplastic types. Neoplastic polyps can turn into cancer. About 70 percent are adenomatous, the most common type. Fifteen percent are villous or tubulovillous adenomas.
Neoplastic polyps, like adenomas and serrated types, can become cancerous if not treated. Non-neoplastic polyps, like hyperplastic and inflammatory, rarely turn into cancer.
Some polyps are more likely to become cancerous than others. Most do not turn into cancer.
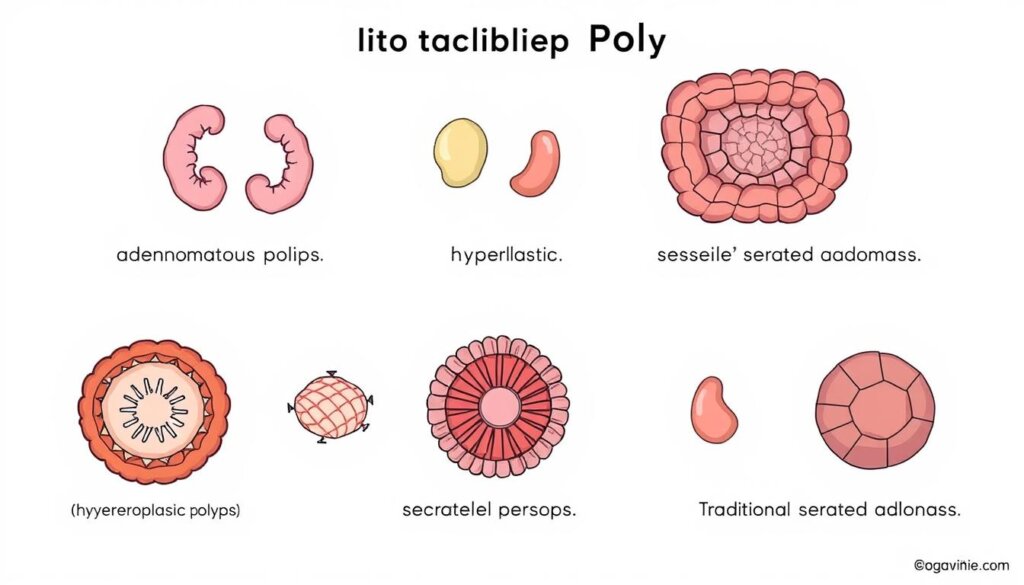
Knowing the type of colon polyp is key for managing them. It helps prevent colorectal cancer.
Prevalence of Colonic Polyps
Colonic polyps are quite common, affecting 15-40% of adults. They become more common with age, hitting about 40% of people over 50. Men are slightly more likely to have them than women.
These growths can happen in anyone, but they’re more common in Western countries. Some genetic conditions, like FAP and Lynch syndrome, raise the risk of getting many polyps early on.
Demographic Factor | Colon Polyp Prevalence |
|---|---|
Overall Adult Population | 15-40% |
People Over 50 Years Old | 40% |
Non-White Men | Most Prevalent |
Children with Lower Gastrointestinal Bleeding | 12% |
Familial Adenomatous Polyposis (FAP) Patients | Majority Develop Colorectal Cancer by Age 40 |
Juvenile Polyposis Syndrome (JPS) Patients | 20% Develop Colorectal Cancer by Age 35 |
In summary, colon polyps are common, especially with age and in men. They’re also more common in certain ethnic groups. People with FAP and Lynch syndrome face a higher risk of getting many polyps early.
Risk Factors for Colonic Polyps
Many things can make you more likely to get colon polyps. Age is a big one, with more polyps showing up after 50. Men are a bit more likely to get them than women.
Being overweight or obese, smoking, drinking a lot of alcohol, and eating too much fat and not enough fiber also up your risk. Some hereditary conditions like FAP, Lynch syndrome, and MUTYH-associated polyposis make you more likely to get polyps early.
If you or your family has had colon polyps or cancer, you’re at higher risk. Knowing these risks helps find who’s at higher risk. It also helps plan better screening to lower colorectal cancer rates.
Risk Factor | Increased Polyp Risk |
|---|---|
Age over 50 | Higher |
Male gender | Slightly higher |
Overweight or obesity | Increased |
Smoking | Increased |
Heavy alcohol use | Increased |
Diet high in fat, low in fiber | Increased |
Hereditary conditions (FAP, Lynch syndrome, MUTYH) | Significantly increased |
Personal or family history of polyps or colorectal cancer | Increased |
Symptoms and Signs of Colonic Polyps
Many people with colon polyps don’t feel any symptoms. But some might notice changes in their bowel habits. These can include constipation, diarrhea, or blood in the stool.
Larger polyps can cause abdominal pain and lead to iron deficiency anemia.
It’s key to remember that these symptoms can mean many things. They don’t always mean you have a polyp. Still, it’s vital to tell a doctor about any unusual digestive issues.
Symptom | Description |
|---|---|
Constipation | Difficulty passing stool or infrequent bowel movements |
Diarrhea | Loose, watery stools that occur more frequently than normal |
Rectal Bleeding | Bright red or dark blood in the stool, on toilet paper, or in the toilet bowl |
Abdominal Pain | Discomfort or pain in the abdominal region |
Iron Deficiency Anemia | A condition where the body lacks sufficient iron, leading to fatigue and other symptoms |
These symptoms don’t always mean you have a polyp. They can have many causes. Still, it’s important to tell a doctor about any unusual digestive issues.
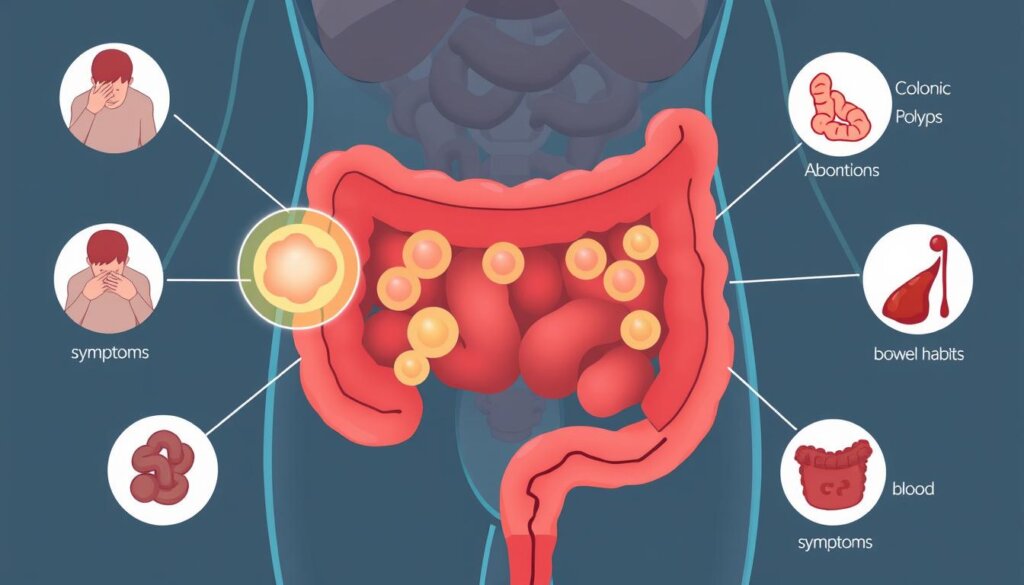
“Most people with colon polyps do not experience any symptoms, and the polyps are often discovered incidentally during routine screening tests like colonoscopy.”
Some people might notice changes in their bowel habits or other digestive issues. However, colon polyps can often go undetected without screening. Regular check-ups and testing are key for early detection and management.
Causes and Development of Colonic Polyps
Colonic polyps grow on the colon’s lining. They happen when genes change, making cells grow without stopping. This can lead to polyp formation. Conditions like Lynch syndrome and FAP increase polyp risk, especially at a young age.
Genetic Mutations
Big polyps can turn cancerous over time if not treated. It’s key to screen and remove polyps early to stop cancer. Studies show over 40% of people in their 50s have precancerous polyps.
A family history of early colon polyps or cancer also raises risk. People with such a history should start screening at 40 or 10 years before their family’s earliest diagnosis.
Lifestyle choices like eating too much fat and red meat increase polyp risk. But eating less fat and more fruits and veggies can lower cancer risk.
Risk Factors for Colonic Polyps | Protective Factors for Colonic Polyps |
|---|---|
|
|
Knowing what causes colonic polyps helps us take steps to stay healthy.
Colon Cancer Risk and Colonic Polyps
Most colon polyps are not harmful. But, if not treated, they can turn into colorectal cancer. About 75% of colorectal cancers start from adenomatous polyps, which are 80% of all polyps. Yet, only 5-10% of these polyps become cancerous.
Polyps over 10 mm (1 cm) in size have a higher risk of becoming cancerous. Most polyps don’t cause symptoms. The bigger a polyp gets, the faster it grows.
Screening for colorectal cancer, like colonoscopies starting at 45, is key. It helps find and remove polyps before they turn into cancer. Removing polyps early can stop colorectal cancer.
“Following colorectal cancer screening guidelines can help discover colorectal cancer at an earlier stage or prevent cancer from developing.”
Some genetic conditions, like Peutz-Jeghers Syndrome (PJS), increase polyp and cancer risk. People with a family history of these syndromes have a 50% chance of getting the gene. They should get genetic counseling and special checks to manage their risk.
Research keeps uncovering how polyps and cancer are linked. By removing polyps and following screening advice, people can lower their cancer risk.
Screening and Detection of Colonic Polyps
Regular screening is key to catch and remove colon polyps early. Colonoscopy is the top choice for finding and removing polyps. It lets doctors see the colon and take out any polyps found.
Other tests like CT colonography, flexible sigmoidoscopy, and stool tests are also used. These tests look for bleeding or genetic changes that might mean polyps or cancer are there.
Colonoscopy
A colonoscopy is very good at checking the whole colon and removing polyps. People at average risk should start screening at 45. Those at higher risk might need to start sooner.
Other Screening Tests
Though colonoscopy is the best, other tests can work for some. Flexible sigmoidoscopy looks at the last part of the colon. Stool tests find blood or DNA signs of polyps or cancer, but a positive test means you need a colonoscopy.
Talking to your doctor about screening options is important. They can help pick the best test for you. Regular screenings help stop polyps and cancer.
“Colonoscopies are vital in the early detection and removal of polyps to prevent cancer formation.”
Prevention and Management of Colonic Polyps
Some things like age and genetics can’t be changed. But, there are steps to help prevent polyps. Eating more fruits, veggies, and whole grains helps. Also, eating less red and processed meat is good.
Staying at a healthy weight and exercising often is key. Quitting smoking and drinking too much alcohol also helps.
For those at higher risk, regular screenings are vital. Removing any found polyps quickly stops cancer. Taking calcium and vitamin D supplements can also help.
Polyp Management Strategies | Lifestyle Changes to Reduce Polyp Risk |
|---|---|
|
|
Preventing colon polyps and managing them well is key to avoiding cancer. By making lifestyle changes, you can help your health.
“Screening with colonoscopy is the best method for preventing colon cancer.”
Genetic Factors and Polyp Risk
Genetic conditions like familial adenomatous polyposis and Lynch syndrome raise polyp and cancer risk. Early and more frequent screenings are needed for these cases.
Knowing how to prevent and manage polyps helps keep your colon healthy.
Conclusion
Colon polyps are often harmless but can prevent colorectal cancer. This cancer is the second leading cause of death in men and the third in women. Regular screenings and early detection are key, as these growths can take years to become cancerous.
By getting the right screening tests, like colonoscopies, you can protect your colon. This helps lower your risk of colorectal cancer.
Colon polyps are common, with up to 40% of people over 50 having them during screenings. Almost 39% of colons over 30 years old have polyps at autopsy. Most polyps are not cancerous, but some can turn into cancer if not treated.
Living a healthy lifestyle and managing risks are important. Regular screenings are also key to preventing dangerous polyps.
Knowing about colon polyps and how to prevent them is empowering. It helps you protect your colon and lower cancer risk. Stay alert and get screenings to catch and remove polyps early. This prevents cancer and keeps you healthy for years to come.
FAQ
What are colonic polyps?
Colonic polyps are small growths on the colon’s lining. They are a type of tumor made of abnormal cells.
What are the different types of colonic polyps?
There are two main types of colonic polyps. Pedunculated polyps have a “head” and “stalk”. Sessile polyps are flat and stick to the wall. They can be non-cancerous or have cancer potential.
How common are colonic polyps?
About 15-40% of adults have colonic polyps. This number goes up with age, especially after 50.
What factors increase the risk of developing colonic polyps?
Risk factors include age and being male. Being overweight, smoking, and heavy drinking also increase risk. A diet high in fat and low in fiber and certain genetic conditions like FAP and Lynch syndrome also play a role.
What are the symptoms of colonic polyps?
Most people with colonic polyps don’t show symptoms. But, some may notice changes in bowel habits, pain, bleeding, or iron deficiency anemia.
What causes the development of colonic polyps?
Polyps develop from gene changes that make cells divide too much. Certain genetic conditions can greatly increase the risk of many polyps.
How do colonic polyps relate to the risk of colon cancer?
Most polyps are not cancerous but can turn into cancer if not treated. Regular screening and removal of polyps are key to preventing cancer.
How are colonic polyps detected and screened for?
A colonoscopy is the best way to screen for polyps. It lets doctors see the colon and remove polyps. Other options include CT colonography, flexible sigmoidoscopy, and stool tests.
How can colonic polyps be prevented or managed?
Eating a healthy diet, staying active, and avoiding smoking and alcohol can help prevent polyps. Regular screening and removing polyps found are also important to stop cancer.