FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
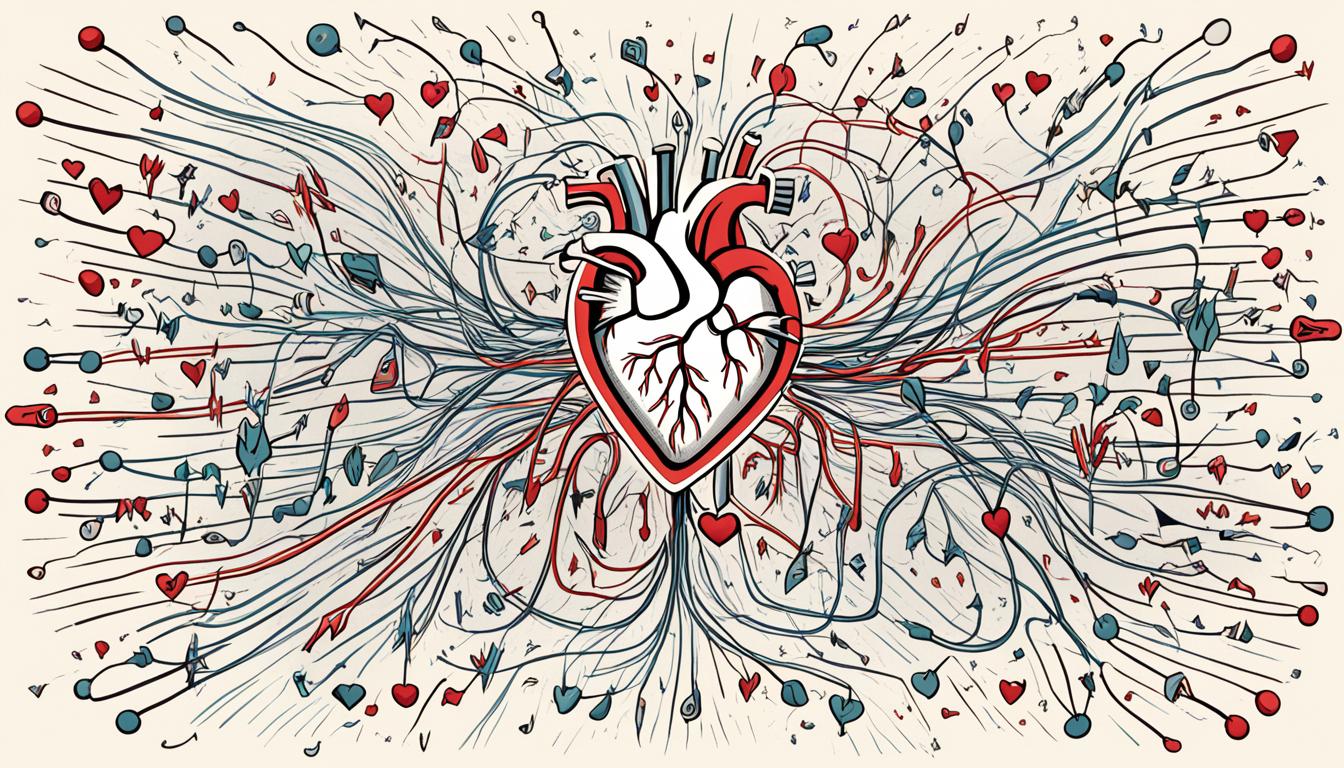
Did you know atrial fibrillation (AFib) can cause your heart to beat up to 175 times a minute? That’s way faster than the usual 60 to 100 beats per minute. This fast and irregular heart rhythm is a big deal. It raises your risk of stroke, heart failure, and other serious problems. It’s important to know about AFib’s causes, signs, and treatment to keep your heart healthy.
Key Takeaways
- Atrial fibrillation is an irregular and often rapid heart rhythm that can lead to serious health complications.
- Common symptoms of AFib include a fast, pounding heartbeat, shortness of breath, and dizziness.
- Underlying heart conditions, high blood pressure, and unhealthy lifestyle habits can all contribute to the development of AFib.
- Diagnostic tests for AFib include electrocardiograms, Holter monitors, and echocardiograms.
- Treatment options for AFib may include medications, cardioversion therapy, and surgical procedures.
What is Atrial Fibrillation?
Overview of Atrial Fibrillation
Atrial fibrillation, or Afib, is a common heart rhythm disorder. It affects the upper chambers of the heart, the atria. Normally, the heart’s rhythm starts with a tiny group of cells at the sinus node. These cells send out an electrical signal that travels to the atrioventricular (AV) node and then to the lower chambers.
However, in atrial fibrillation, electrical signals come from many places in the upper chambers, making the heart beat chaotically. The AV node can’t stop all these signals, so the heart beats fast and irregularly, often over 400 times a minute.
This condition can be classified into three types: paroxysmal Afib, persistent Afib, and long-standing persistent Afib. Symptoms include chest pain, dizziness, fainting, palpitations, weakness, and shortness of breath. It’s more common in people with a family history of it, especially if they started young.
Around 1.4 million people in the UK have atrial fibrillation, making it the most common type of cardiac arrhythmia. It’s more common in older people and affects more men than women. It’s also the leading cause of stroke.
Risk factors include being older, having high blood pressure, heart or lung disease, congenital heart disease, and drinking too much alcohol.
“Atrial fibrillation is a serious condition that can increase the risk of stroke, heart failure, and other complications if left untreated. Understanding the causes, symptoms, and available treatments is crucial for managing this heart rhythm disorder.”
Symptoms of Atrial Fibrillation
Atrial fibrillation (AFib) can cause a fast, fluttering heartbeat, known as palpitations. Some people with AFib may feel chest pain, dizziness, fatigue, and shortness of breath. But, not everyone with AFib notices these symptoms.
AFib’s type affects its symptoms. Paroxysmal fibrillation means the heart goes back to normal in seven days. Persistent AFib lasts over seven days and needs treatment. Long-standing persistent AFib lasts over a year, and permanent AFib is forever.
Older adults might not notice AFib symptoms as much. They might find out during checkups or EKG screenings. Women with AFib often have milder symptoms than men. At night, AFib symptoms can include heavy breathing and sweating.
If you have chest pain or other serious symptoms, get medical help fast. These could mean a heart attack or stroke.
Managing atrial fibrillation is key to avoiding serious problems like stroke. Knowing the symptoms and getting medical help quickly can help improve heart health and life quality.
Causes of Atrial Fibrillation
Heart Conditions Causing Atrial Fibrillation
Atrial fibrillation, or AFib, often starts with heart structure problems. The top reason for AFib is a heart structure issue. Heart diseases and health issues can raise your risk of getting this irregular heart rhythm. These include congenital heart defects, sick sinus syndrome, sleep apnea, heart attacks, and more.
Atrial fibrillation is the most common heart rhythm disorder and the main cause of stroke. Factors that increase your risk include being older, having high blood pressure, heart and lung diseases, and more. About 9% of people over 75 have atrial fibrillation. Experts think the number of people with atrial fibrillation will jump by 2050.
Some lifestyle choices can also trigger AFib, like drinking too much alcohol or caffeine, using drugs, smoking, and certain medicines.
Heart Condition | Link to Atrial Fibrillation |
|---|---|
Congenital Heart Defect | Structural heart problems can mess up normal electrical signals, leading to AFib. |
Sick Sinus Syndrome | Issues with the heart’s pacemaker can cause irregular heart rhythms like AFib. |
Sleep Apnea | Sleep apnea puts strain on the heart, raising the risk of AFib. |
Heart Attack | Heart muscle damage from a heart attack can lead to AFib. |
Heart Valve Disease | Bad heart valves can mess up electrical signals and cause AFib. |
High Blood Pressure | High blood pressure that’s not controlled can weaken and enlarge the heart, making AFib more likely. |
Coronary Artery Disease | Blocked or damaged arteries can make the heart work less efficiently and cause AFib. |
Thyroid Disease | Too much or too little thyroid hormone can lead to AFib. |
Infections | Certain infections can cause heart inflammation and damage, triggering AFib. |
About 9% of people over 75 have atrial fibrillation. By 80, the risk of getting atrial fibrillation at some point in life goes up to 22%.
“Atrial fibrillation is a serious condition that can lead to heart failure, stroke, and other complications if left untreated. It’s important to work closely with your healthcare provider to identify and address any underlying causes.”
Risk Factors for Atrial Fibrillation
Atrial fibrillation (AFib) is a complex condition with many risk factors. These factors can make you more likely to get it. Knowing about these risks is key for prevention and early action.
Age is a big risk factor for AFib. The risk goes up as you get older, especially after 65. By 2030, the CDC says 12.1 million U.S. adults will have AFib.
Your genes can also affect your risk. People of European descent face a higher risk than others. Within this group, women are more likely to have AFib than men.
Some heart conditions increase the risk of AFib. These include heart attacks, certain heart defects, and past heart surgery. High blood pressure is a top risk factor. It often comes with other health issues, like COPD, which also raises the risk.
What you do in your daily life can also be a risk. Things like caffeine, nicotine, alcohol, and drugs can cause AFib episodes. Electrolyte imbalances, like low potassium, also increase your risk.
Other factors include obesity, diabetes, metabolic syndrome, and sleep apnea. These can strain your heart and make you more likely to get AFib.
Knowing these risks is important. Talk about them with your doctor. This will help you manage your health better and lower your risk of AFib.

Risk Factor | Explanation |
|---|---|
Age | The risk of AFib increases significantly as you get older, with the condition being most common in adults over the age of 65. |
Genetic Background | Individuals of European ancestry are more likely to have AFib compared to those of Black, Hispanic, or Asian descent. Among people of European ancestry, those assigned female at birth are more likely to have AFib than those assigned male at birth. |
Heart Conditions | Certain heart conditions, such as heart attacks, structural heart defects, and previous heart surgery, can increase your risk of developing AFib. |
High Blood Pressure | High blood pressure is the most common condition linked to AFib, and conditions like chronic obstructive pulmonary disease (COPD), which often coexist with high blood pressure and heart disease, can further raise your risk. |
Lifestyle Factors | Caffeine, nicotine, alcohol, and illegal drug use can trigger AFib episodes. Electrolyte imbalances, such as low potassium levels, have also been linked to an increased risk of AFib. |
Other Conditions | Obesity, diabetes, metabolic syndrome, and sleep apnea can put additional strain on your heart and increase your susceptibility to AFib. |
Complications of Atrial Fibrillation
Blood Clots and Stroke Risk
Atrial fibrillation (AFib) greatly raises the chance of blood clots and stroke. Those with AFib face a much higher stroke risk than others. These clots can block blood flow to important organs like the brain, lungs, and kidneys. A stroke from a blocked blood vessel means the brain doesn’t get enough oxygen, leading to cell death. Strokes can cause long-term disability, brain decline, and even death.
High blood pressure, diabetes, heart failure, and certain heart valve diseases increase the stroke risk for AFib patients. Doctors often prescribe blood thinners to prevent clots and stroke in AFib patients. But these drugs can also raise the chance of bleeding in the brain, stomach, or kidneys.
AFib can also cause heart failure. Its fast, irregular heart rate can weaken the heart muscle, leading to lung fluid and less oxygen for the body. This can make people feel very tired and increase the risk of brain decline and even dementia.
Managing AFib and its risks, like high blood pressure and diabetes, is key to avoiding these serious issues. A mix of medicines, lifestyle changes, and sometimes surgery can help lower risks and improve health for those with AFib.
Preventing Atrial Fibrillation
Living a heart-healthy life can lower your risk of atrial fibrillation (AF). To prevent this heart rhythm issue, it’s important to manage high blood pressure, high cholesterol, and diabetes. Quitting smoking, eating a diet low in salt and saturated fat, and exercising regularly can also help.
Caffeine and alcohol can trigger AF episodes. Potassium-rich foods like fruits, vegetables, and legumes can help prevent AF. Yoga and the Valsalva maneuver may also improve heart health and lessen AF symptoms.
Keeping a healthy weight and drinking plenty of water are more ways to prevent AF. By following these heart-healthy habits, you can greatly reduce your risk of atrial fibrillation and its serious complications, like stroke and heart failure.
Lifestyle Factors | Impact on Atrial Fibrillation Risk |
|---|---|
High Blood Pressure | Increases risk |
High Cholesterol | Increases risk |
Diabetes | Increases risk |
Smoking | Increases risk |
Unhealthy Diet | Increases risk |
Physical Inactivity | Increases risk |
Excess Alcohol | Triggers AF episodes |
Dehydration | Increases risk of AF episodes |
Focusing on a heart-healthy lifestyle can prevent atrial fibrillation and lower your risk of serious problems.
Diagnosing Atrial Fibrillation
If you notice your heartbeat is not regular, your doctor will check you with tests to see if you have atrial fibrillation. They use tests like an electrocardiogram (ECG or EKG), Holter monitor, and more to find out what’s going on. These tests help figure out if you have atrial fibrillation and what might be causing it.
Tests for Atrial Fibrillation
An ECG is quick, takes about 5 minutes, and shows the heart’s electrical activity. It can spot heart rhythms that suggest atrial fibrillation. Sometimes, a Holter monitor or an event recorder is used to watch the heart over time, catching any odd beats.
An echocardiogram uses ultrasound to visualize the heart’s shape and function. Stress tests and chest X-rays might also be performed to examine the heart more closely and rule out other issues.
Your doctor, such as a cardiologist or electrophysiologist, will choose the right tests and plan your treatment.
“Atrial fibrillation can be asymptomatic in some cases, making it necessary for a doctor to confirm the diagnosis through tests.”
With a full check-up, your doctor can make sure you have atrial fibrillation and create a plan to help you. This plan aims to manage your condition and lower the risk of problems.
Test | Purpose |
|---|---|
Electrocardiogram (ECG) | Measures the heart’s electrical activity, detects irregular heart rhythms |
Holter Monitor | Continuously records the heart’s activity over 24-48 hours |
Event Recorder | Captures irregular heart rhythms over a period of time |
Implantable Loop Recorder | Monitors heart activity for up to 30 days, transmitting data for analysis |
Echocardiogram | Creates images of the heart to assess its structure and function |
Stress Test | Evaluates the heart’s response to physical activity and increased heart rate |
Chest X-Ray | Checks for underlying conditions that may contribute to atrial fibrillation |
Using these tests together, your doctor can find out if you have atrial fibrillation and what’s causing it. This helps them make a good plan to manage your condition and reduce risks.
Treatment Options for Atrial Fibrillation
Treating atrial fibrillation (AFib) focuses on controlling the heart rate and rhythm. It also aims to prevent blood clots that can cause stroke. There are many medications and procedures to help manage this condition.
Medications for Atrial Fibrillation
Medicines are key in treating atrial fibrillation. Beta-blockers, calcium channel blockers, and digoxin help control the heart rate. Antiarrhythmic drugs like flecainide, propafenone, and amiodarone work to fix the heart’s rhythm.
Direct-acting anticoagulants like rivaroxaban, dabigatran, apixaban, and edoxaban are recommended for those at high or moderate risk of stroke. If other anticoagulants aren’t suitable, warfarin might be given, but it carries a higher risk of bleeding. Warfarin requires regular blood tests and may need dose changes based on the results.
Cardioversion Therapy
Cardioversion, a process that uses a controlled electric shock, can help restore normal heart rhythm. However, if the atrial fibrillation lasts more than two days, it may increase clotting risk. Before and after cardioversion, anticoagulants are often given to lower stroke risk.
Other options like catheter ablation or pacemaker implantation might be considered if medications don’t work or aren’t tolerated. Catheter ablation targets the heart area, causing problems with stopping abnormal electrical signals. Pacemakers, small devices implanted under the collarbone, help regulate heartbeats, especially for those 80 or older.
The right treatment depends on the person’s situation, including symptom severity, the cause of atrial fibrillation, and overall health. A detailed check-up with a healthcare provider is crucial to find the best treatment plan.
Surgical and Catheter Procedures
If medications or cardioversion don’t work, more invasive procedures might be needed for atrial fibrillation (AFib). Cardiac ablation uses heat or cold to make scars in the heart, stopping irregular signals. Catheter ablation, like radiofrequency and cryoablation, is a common way to treat AFib. These procedures can take 3 to 6 hours, and recovery varies, with some going home the same day and others staying in the hospital for a few days.
Another surgical option is the maze procedure. It cuts into the chest to create scar tissue that helps the heart’s signals work better. This method works well for 60%–70% of patients, allowing many to stop blood thinners later. Closing the left atrial appendage during the maze also cuts stroke risk by over 30%. Recovery takes about 6 to 8 weeks.
Hybrid ablation combines surgery and catheter techniques, and pulsed-field ablation uses electric pulses to stop irregular heart rhythms. Left atrial appendage closure also helps prevent clots from forming.
Surgical ablation, including the maze procedure, is an option when other treatments fail or aren’t tolerated. But, it comes with risks like bleeding, blood clots, and the need for a pacemaker. Older patients, those who are overweight, or those with other health issues might face more complications. It’s important to talk about these risks with your surgeon.
After any procedure, making lifestyle changes is key to keeping your heart healthy. This includes eating right, quitting smoking, managing weight, staying active, and handling stress.
Procedure | Success Rate | Recovery Time | Risks |
|---|---|---|---|
Catheter Ablation | Common procedure for AFib | Same-day discharge to 1 week | Bleeding, blood clots, need for pacemaker |
Maze Procedure | 60%-70% success rate | 6-8 weeks | Bleeding, blood clots, need for a pacemaker, complications from anesthesia, kidney failure, infection. |
Hybrid Ablation | An effective procedure for AFib | Varies depending on the procedure | Risks associated with both surgical and catheter-based techniques |
Pulsed Field Ablation | An effective procedure for AFib | Varies depending on the procedure | Potential risks similar to other ablation procedures |
Left Atrial Appendage Closure | Decreases stroke risk by over 30% | Varies depending on the procedure | Risks associated with the procedure itself |
Studies have shown that surgical and catheter-based procedures are effective for treating atrial fibrillation. These methods can be good options for patients who haven’t found relief with other treatments.
Lifestyle Changes for Atrial Fibrillation
Keeping a heart-healthy lifestyle is key for managing atrial fibrillation. Experts suggest making these changes:
- Eat more fruits, veggies, and whole grains, and less sugar, salt, and saturated fats.
- Do 30-60 minutes of exercise most days to help control weight, sleep better, and strengthen your heart.
- Keep a healthy weight by losing at least 10% of your body weight through diet and exercise.
- Stop smoking and avoid nicotine to prevent making atrial fibrillation worse and to lower heart disease risk.
- Drink less alcohol, as too much can cause atrial fibrillation, especially if you’re on blood thinners.
- Manage stress with activities like meditation or yoga, which can cause irregular heartbeats.
- Get 7 to 9 hours of sleep each night, as many people with atrial fibrillation have sleep problems.
- Drink less caffeine, as it can make heart rhythm issues worse in people with atrial fibrillation.
People with atrial fibrillation can better manage their condition and improve their heart health by changing their lifestyle.
Lifestyle Factor | Recommended Changes | Impact on Atrial Fibrillation |
|---|---|---|
Diet | Increase fruits, vegetables, and whole grains; Limit sugar, salt, and saturated fats. | It helps manage blood pressure and cholesterol levels, supporting heart health |
Exercise | Engage in regular physical activity for 30-60 minutes most days | It aids in weight control, improves sleep, and strengthens the heart muscle |
Weight Management | Lose at least 10% of body weight through diet and exercise | Crucial for managing atrial fibrillation in obese individuals |
Smoking and Nicotine | Quit smoking and avoid nicotine consumption | It helps prevent exacerbation of atrial fibrillation and reduces cardiovascular risks |
Alcohol | Limit alcohol intake, especially for those taking blood thinners | Excessive consumption can trigger atrial fibrillation episodes |
Stress Management | Engage in stress-reducing activities like meditation or yoga | Stress can trigger episodes of irregular heart rhythm |
Sleep | Ensure 7-9 hours of sleep per night | Sleep disturbances are common in individuals with atrial fibrillation |
Caffeine | Limit caffeine intake from sources like coffee, tea, energy drinks, and chocolate. | Caffeine consumption can trigger heart palpitations in those with atrial fibrillation. |
People with atrial fibrillation can manage their condition by making these lifestyle changes and boosting their heart health.
Conclusion
Atrial fibrillation (AFib) is a serious but treatable heart rhythm disorder. It affects 2.7 to 6.1 million people in the U.S., which could reach nearly 12.1 million by 2030. AFib becomes more common with age, hitting about 10% of people by age 80. This condition raises the risk of stroke, heart failure, dementia, and death.
Understanding AFib’s causes, symptoms, and treatments helps patients work with their doctors. Together, they can create a plan to manage AFib and lower the risk of serious problems.
Diagnosing and managing AFib is key because it can harm the heart and increase pressure in the lungs, leading to heart failure. People with AFib may feel tired, short of breath, dizzy, have palpitations, chest pain, or pass out. A 12-lead ECG is the best way to spot AFib, showing no P waves, F waves, and an irregular heart rhythm.
Living a heart-healthy life can help prevent or manage AFib. With the right care, many people with AFib can lead active, healthy lives. As AFib becomes more common, we must spread awareness and support effective management. This will help patients and ease the load on healthcare.
FAQ
What is atrial fibrillation?
Atrial fibrillation (AFib) is when the heart beats irregularly and too fast. This can cause blood clots in the heart. It also raises the risk of stroke, heart failure, and other heart problems.
What causes atrial fibrillation?
Various heart diseases and health issues can cause AFib. These include congenital heart defects and sick sinus syndrome. Other causes include sleep apnea, heart attack, and high blood pressure.
Coronary artery disease, thyroid disease, and infections can also trigger it. Drinking too much alcohol or caffeine, using drugs, smoking, and certain medicines can lead to AFib episodes.
What are the symptoms of atrial fibrillation?
AFib symptoms include a fast, fluttering heartbeat and chest pain. You might feel dizzy, tired, lightheaded, or have trouble exercising. Some people with AFib don’t have any symptoms.
How is atrial fibrillation diagnosed?
Doctors use tests to diagnose AFib. These include blood tests and an electrocardiogram (ECG or EKG) to check the heart’s electrical activity. Other tests like a Holter monitor and echocardiogram may also be done.
They might also use an exercise stress test and a chest X-ray.
What are the treatment options for atrial fibrillation?
Treatment for AFib focuses on controlling the heart rate and preventing blood clots. Doctors may prescribe medications like beta blockers and anticoagulants. If these don’t work, procedures like cardiac ablation may be needed.
Other options include the surgical maze procedure and left atrial appendage closure.
How can I prevent atrial fibrillation?
To lower the risk of AFib, follow a healthy lifestyle. This means controlling high blood pressure, cholesterol, and diabetes. Avoid smoking and eat a diet low in salt and fat.
Exercise regularly, get enough sleep, and maintain a healthy weight to help prevent AFib.
What are the complications of atrial fibrillation?
AFib can lead to blood clots, which increase the risk of stroke. The risk of stroke goes up with age and in people with certain health conditions. AFib can also cause bleeding in the brain, digestive system, or urinary tract.
It can lead to heart failure as well.