FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
More than 23.5 million people in the United States have autoimmune diseases. This shows how common these conditions are. They happen when the body’s immune system attacks its own cells and tissues. This leads to chronic inflammation and symptoms that can really affect someone’s life.
These diseases can affect many parts of the body. They can hit the joints, skin, organs, and nervous system. Some common ones are Type 1 diabetes, multiple sclerosis (MS), rheumatoid arthritis (RA), lupus, Crohn’s disease, and psoriasis. Finding out you have one of these diseases can be hard. The symptoms can be like other illnesses, making it hard to diagnose.
Key Takeaways
- Autoimmune diseases are conditions in which the immune system mistakenly attacks the body’s own healthy cells and tissues.
- Over 23.5 million people in the United States are affected by autoimmune diseases, with a significant proportion being women.
- Common autoimmune diseases include Type 1 diabetes, multiple sclerosis, rheumatoid arthritis, lupus, Crohn’s disease, and psoriasis.
- Diagnosis of autoimmune diseases can be challenging, often taking months or years to confirm due to the similarity of symptoms with other conditions.
- Treatment for autoimmune diseases involves a range of medications and therapies to manage symptoms and prevent further damage.
What are Autoimmune Diseases?
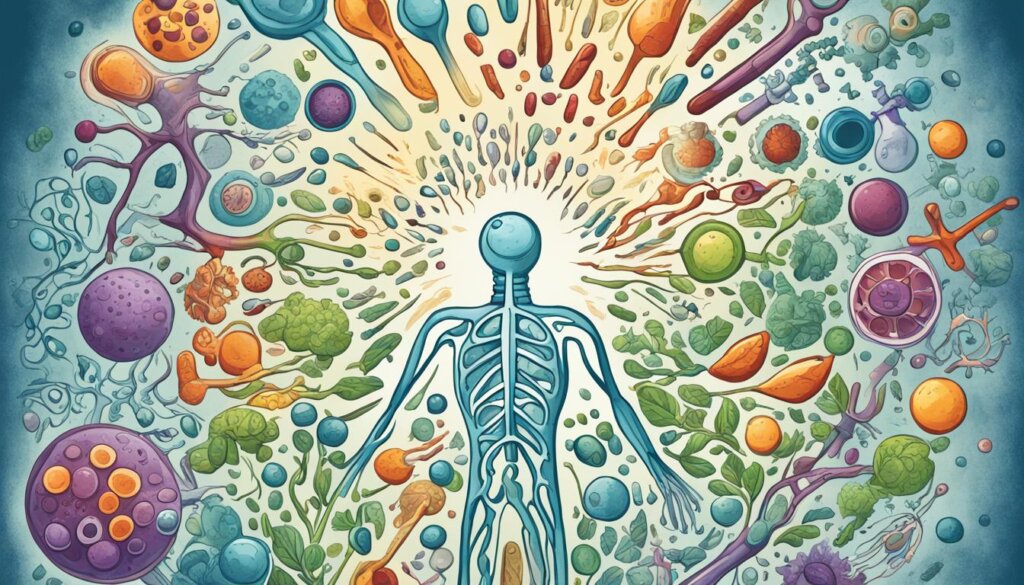
Autoimmune diseases happen when the immune system attacks the body’s own cells by mistake. This leads to the production of autoantibodies. These proteins harm the body’s tissues, causing inflammation and pain.
Overview of the Immune System Malfunction
Normally, the immune system knows the difference between the body’s cells and invaders. But in autoimmune diseases, it gets mixed up. This makes it attack the body’s own tissues and organs. This can affect the skin, joints, muscles, and internal organs, causing many symptoms.
Autoantibodies and Healthy Cell Damage
Autoantibodies, made by the immune system, wrongly target and harm the body’s healthy cells. This leads to autoimmune diseases. These autoantibodies can attack different parts of the body, like the thyroid gland, joints, or nervous system, based on the disease.
Managing autoimmune diseases can be tough because symptoms change a lot. But with the right treatment and lifestyle changes, many people can live well with their condition.
Autoimmune Disorder | Affected Body Part | Symptoms |
|---|---|---|
Rheumatoid Arthritis | Joints | Joint pain, swelling, stiffness |
Lupus | Multiple Organs | Fatigue, joint pain, skin rashes |
Multiple Sclerosis | Central Nervous System | Muscle weakness, vision problems, cognitive impairment |
Autoimmune diseases are complex and hard to manage. But understanding them better helps people work with their doctors to find good treatments. This can improve their health and well-being.
“The immune system is a complex network of cells, tissues, and organs that work together to protect the body from infection and disease. In autoimmune diseases, this delicate balance is disrupted, leading the immune system to attack the body’s own healthy cells.”
Common Symptoms of Autoimmune Diseases
Autoimmune diseases show many symptoms that are hard to spot. Early signs include feeling very tired, dizzy without reason, having a low fever, muscle pain, and swelling without cause. These signs are often thought to be something else, so it’s key to work with doctors to find the real cause.
Flare-ups and Remission Cycles
Many autoimmune diseases go through ups and downs. When they get worse, symptoms can make life hard. Then, they might get better, giving relief from symptoms. Knowing and handling these ups and downs is important for a good life.
“Autoimmune diseases can be challenging to manage due to the cyclical nature of symptoms. Patients must learn to navigate periods of increased discomfort and then find ways to maintain their health during remission.”
Autoimmune diseases have many different symptoms, but they all happen when the immune system attacks the body. To manage these diseases, you might need medicine, to change your lifestyle, and to work closely with doctors.
Autoimmune Diseases
Autoimmune diseases are a wide range of conditions that affect many people around the world. Over 100 different autoimmune diseases have been found, including rheumatoid arthritis, lupus, multiple sclerosis, type 1 diabetes, and more. Each disease targets specific parts of the body, causing unique symptoms and problems.
These diseases happen when the body’s immune system attacks its own healthy cells and tissues. This can lead to inflammation, pain, and damage to organs. The reasons for these diseases are complex, involving both genes and the environment.
Autoimmune Disease | Affected Body Part(s) | Symptoms |
|---|---|---|
Rheumatoid Arthritis | Joints | Joint pain, swelling, and stiffness |
Lupus | Multiple organs | Fatigue, joint pain, skin rashes, and organ damage |
Multiple Sclerosis | Central nervous system | Muscle weakness, numbness, vision problems, and cognitive impairment |
Type 1 Diabetes | Pancreas | High blood sugar, increased thirst and urination, weight loss |
Inflammatory Bowel Disease | Digestive system | Abdominal pain, diarrhea, and weight loss |
Diagnosing and managing autoimmune diseases can be tough because of similar symptoms and the need for special care. But, with the right treatment and lifestyle changes, many people can control their symptoms and live better lives.
“Autoimmune diseases are complex, but with increased awareness and research, we can better understand and manage these conditions to improve the lives of those affected.”
Causes and Risk Factors
We don’t fully know why autoimmune diseases happen. But, it seems that genes and the environment play a big part. Genetic predisposition makes some people more likely to get an autoimmune disease. Things like infections, chemicals, or toxins can also trigger the immune system and lead to these diseases.
Genetic Predisposition
If your family has autoimmune diseases, you might be more likely to get one too. Some genes make people more prone to these conditions. These genes can be passed down through families.
Environmental Triggers
Things around us can also cause autoimmune diseases. Smoking, being overweight, and some medicines can increase the risk. The SARS-CoV-2 virus has been linked to autoimmune diseases like Guillain-Barre syndrome and lupus.
Being a woman also raises the risk, as most people with these diseases are women. Some diseases, like lupus and Sjogren’s syndrome, mostly affect women. Women are also more likely to get arthritis and multiple sclerosis.
Some things that increase the risk of autoimmune diseases are out of our control. But, we can make choices to lower the risk. Eating well, exercising, and avoiding toxins and infections can help.
Autoimmune Disease | Prevalence in the United States |
|---|---|
Total Autoimmune Diseases | 24 million people |
Sjogren’s Disease | 400,000 to 3.1 million adults |
Inflammatory Bowel Diseases (IBD) | Approximately 3 million people |
Graves’ Disease | 1 in 200 people |
Hashimoto’s Thyroiditis | 5 in 100 people |
Systemic Lupus Erythematosus (Lupus) | 1.5 million people in the U.S., 5 million worldwide |
Rheumatoid Arthritis | 1.3 million U.S. adults |
Psoriatic Arthritis | Develops in about 3 in 10 people with psoriasis |
Psoriasis | More than 8 million people or 2-3% of the world’s population |
Celiac Disease | May affect as many as 2 million people in the U.S. |
Type 1 Diabetes | 1 in 300 people in the U.S. by age 18 |
“Autoimmune diseases are a leading cause of death and disability in the United States.”
Type 1 Diabetes
Type 1 diabetes is an autoimmune disease. It happens when the body’s immune system attacks the cells that make insulin in the pancreas. Without insulin, the body can’t use glucose for energy. This leads to high blood sugar levels that can harm blood vessels, nerves, and organs over time.
Insulin-Producing Cell Destruction
The immune system in type 1 diabetes sees the insulin-producing beta cells as foreign. It attacks and destroys these cells. This means the person needs synthetic insulin for life to keep blood sugar levels healthy and avoid serious problems.
High Blood Sugar Complications
High blood sugar can cause big problems for people with type 1 diabetes. It can lead to heart disease, kidney damage, nerve damage, and vision loss if not managed. To avoid these risks, managing type 1 diabetes with insulin, checking blood sugar, and counting carbs is key.
Studies have looked into how common type 1 diabetes is and its link to other health issues. Knowing about type 1 diabetes and its related conditions helps doctors and people with the disease a lot.
“Insulin is the key to managing type 1 diabetes, but it’s a delicate balance that requires constant monitoring and adjustment. With the right care and support, individuals with this autoimmune disease can lead healthy, fulfilling lives.”
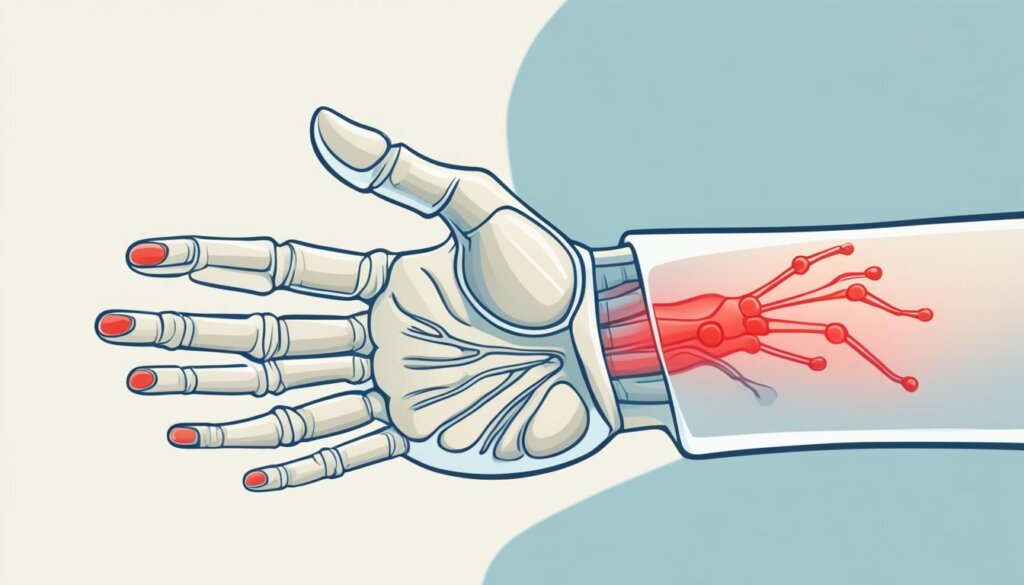
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune disease that mainly attacks the joints. It causes inflammation, swelling, and a lot of pain. This chronic condition happens when the immune system mistakenly attacks the synovial lining of the joints. This leads to damage over time. Unlike other arthritis types, RA often affects joints on both sides of the body equally.
At first, X-rays might not show any changes in the bones with RA. But, the disease can get worse fast, causing joints to deform and lose function if not treated. RA symptoms can be mild or severe. They can get worse with stress, environmental factors, or changes in medication.
RA can also affect parts of the body besides the joints, like the heart, lungs, blood, nerves, eyes, and skin. The American Diabetes Association (ADA) says RA is a disability if it greatly limits someone’s daily activities.
To manage RA well, you need to use many approaches. This includes medicines to calm down the immune system and reduce swelling. Making lifestyle changes also helps control symptoms. Starting treatment early is key to stop joint damage and make life better for those with this condition.
Characteristic | Description |
|---|---|
Joint Involvement | Rheumatoid arthritis mainly affects the joints, often in a symmetrical way. It commonly hits the wrists, hands, elbows, shoulders, feet, spine, knees, and jaw. |
Symptoms | Symptoms include joint pain, swelling, stiffness, loss of function, fatigue, occasional fevers, and loss of appetite. |
Systemic Effects | Rheumatoid arthritis can also affect areas outside the joints, like the heart, lungs, blood, nerves, eyes, and skin. |
Treatment Approach | Managing rheumatoid arthritis means using medicines to calm the immune system and reduce swelling. Making lifestyle changes also helps control symptoms. |
In summary, rheumatoid arthritis is an autoimmune disease that mainly targets the joints. It leads to inflammation, swelling, and pain. Early detection and full treatment are key to stop joint damage and make life better for those with this condition.
Psoriasis and Psoriatic Arthritis
Psoriasis is an autoimmune disease that makes skin cells grow too fast. This leads to thick, scaly patches on the skin. Sometimes, it also affects the joints, causing psoriatic arthritis. This brings inflammation, swelling, and pain to the joints. Stress, infections, and some medicines can trigger this overproduction of skin cells.
About 30% of people with psoriasis also get psoriatic arthritis. Around 40% of those with psoriatic arthritis have a family member with psoriasis or psoriatic arthritis. This condition usually starts in people between 30 and 55 years old, but can start in childhood too.
There’s no cure for psoriasis, but treatments help slow skin cell growth and reduce inflammation. Psoriatic arthritis can cause more problems like fatigue, swelling, and heart disease.
Skin Cell Overproduction
Psoriasis makes skin cells grow too fast, causing thick, scaly patches. This happens because the immune system attacks healthy skin cells by mistake.
Joint Inflammation and Pain
Psoriasis can also affect the joints, leading to psoriatic arthritis. This causes inflammation, swelling, and pain in the joints. It can make moving around hard and lower quality of life.
Condition | Symptoms | Risk Factors |
|---|---|---|
Psoriasis |
|
|
Psoriatic Arthritis |
|
|
“Psoriasis and psoriatic arthritis are complex autoimmune conditions that can have a significant impact on a person’s physical and mental well-being. Understanding the underlying causes and recognizing the early warning signs is crucial for timely diagnosis and effective management of these conditions.”
Multiple Sclerosis
Multiple sclerosis (MS) is an autoimmune disease. It targets the protective myelin sheath around nerve cells in the central nervous system. This damage to the myelin sheath slows down signals between the brain, spinal cord, and the body. This leads to symptoms like numbness, weakness, balance issues, and vision problems.
Myelin Sheath Damage: The Root Cause
In MS, the immune system attacks and damages the myelin sheath. This sheath is key for nerve signal transmission. This damage disrupts communication between the brain and the body. It leads to a variety of symptoms that can vary a lot in severity and progression.
MS can progress in different ways. Some people have relapses and remissions, while others get worse over time. This can affect mobility and daily life. Symptoms like muscle weakness, balance issues, and vision problems make everyday tasks hard. People with MS might need assistive devices or rehab to stay independent and live well.
Even though MS is complex, research and treatments offer hope. With a mix of medications, rehab, and lifestyle changes, people with MS can manage their symptoms. This helps slow the disease’s progress, letting them live fulfilling lives.
Key Facts about Multiple Sclerosis | Statistics |
|---|---|
Age of onset | MS can first appear in people between the ages of 20 and 40. |
Gender differences | Women are up to three times more likely than men to have relapsing-remitting MS. |
Genetic risk | The general population’s risk for MS is about 0.5%, but if a parent or sibling has MS, the risk increases to about 1%. |
Ethnic differences | People of Asian, African, and Native American ancestry have the lowest risk of developing MS. |
Comorbidities | Those with autoimmune thyroid disease, pernicious anemia, psoriasis, type 1 diabetes, or inflammatory bowel disease have a slightly increased risk of MS. |
The future looks promising as scientists learn more about multiple sclerosis and find new treatments.
Inflammatory Bowel Diseases
Inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis are autoimmune disorders. They cause inflammation and damage in the gut. These conditions can really affect someone’s life and increase the risk of serious problems, like blockages or perforations.
Crohn’s Disease and Ulcerative Colitis
Crohn’s disease can hit any part of the digestive system. Ulcerative colitis mainly affects the large intestine and rectum. Symptoms include diarrhea, stomach pain, bleeding from the rectum, and losing weight. People with IBD often have ups and downs, with times of flare-ups and times of feeling better.
Research shows that IBD might have a genetic link. It could be caused by a mix of genes, family history, and environment. About 20% of people with IBD have a family history of it. It’s more common in white people and those of Ashkenazi Jewish descent.
IBD can cause serious problems, like heavy bleeding, bowel perforation, or narrowing. It also raises the risk of colon cancer.
To diagnose IBD, doctors use tests like stool exams, blood tests, and imaging. Treatment includes medicines to calm the immune system and reduce inflammation. People with IBD should also focus on diet, managing stress, and joining support groups.
Statistic | Value |
|---|---|
Family history of IBD | As many as 20% of people with IBD have a family history of it. |
Race and ethnicity | IBD is more common in white people and individuals of Ashkenazi Jewish descent. |
Genetic factors | In 2006, the first gene associated with Crohn’s disease, the NOD2 gene, was identified. Since then, researchers have uncovered more than 200 related genomic regions for IBD. |
Flare-ups and remission | As with other chronic diseases, a person with IBD will generally go through periods in which the disease flares up and causes symptoms, followed by periods in which symptoms decrease or disappear and good health returns. |
Complications | IBD can lead to several serious complications in the intestines, including profuse intestinal bleeding from the ulcers, perforation or rupture of the bowel, narrowing and obstruction of the bowel (stricture), fistulae and perianal disease, toxic megacolon, and malnutrition. |
Colon cancer risk | IBD, particularly ulcerative colitis, increases the risk of colon cancer. |
Extraintestinal complications | IBD can also affect other organs, arthritis being the most common complication outside the intestines. |
About 1.6 million Americans have IBD, most getting diagnosed before they turn 35. Between 5% and 20% of those with IBD have a family link to the disease. IBD can make colon cancer risk go up to four times, especially in young people or those with a family history.
“IBD can lead to several serious complications in the intestines, including profuse intestinal bleeding from the ulcers, perforation or rupture of the bowel, narrowing and obstruction of the bowel (stricture), fistulae and perianal disease, toxic megacolon, and malnutrition.”
Experts say 10% to 43% of IBD patients might face eye problems like redness and swelling. Half of IBD patients might need surgery to fix damaged intestines or fix blockages and other issues.
In conclusion, IBD, including Crohn’s disease and ulcerative colitis, are complex conditions that can greatly affect life quality. Knowing about symptoms, causes, and complications is key for managing and preventing long-term health issues.
Other Common Autoimmune Disorders
There are many autoimmune diseases besides the ones we’ve talked about. Graves’ disease affects the thyroid gland. Hashimoto’s thyroiditis can make the thyroid work less well. Myasthenia gravis is a disorder of the nerves and muscles. Celiac disease happens when eating gluten. And vasculitis is when blood vessels get inflamed.
Lupus is most common in women and people in their teens to mid-40s. It’s also more common in African Americans, Native Americans, Native Alaskans, Native Hawaiians, and some Asian groups. Sjögren’s syndrome mostly affects women and is often found in people over 40.
Rheumatoid arthritis (RA) is more common in women and gets more likely with age. But it can start at any time. Psoriasis is more common in adults, not kids. Psoriatic arthritis often starts in adults too. It can be triggered by stress, injury, or illness.
Each autoimmune disorder has its own set of symptoms and treatments. This shows how complex and varied these conditions are.

“Autoimmune diseases are a diverse group of disorders in which the body’s immune system attacks its own healthy tissues, causing inflammation, tissue damage, and a wide range of symptoms depending on the specific condition.”
Diagnosis and Testing
Diagnosing autoimmune diseases is hard because many symptoms look like other health issues. Doctors start by taking a detailed history and doing a full physical check-up.
Blood Tests and Imaging
Blood tests can show clues about the disease. For example, high levels of CRP mean there’s inflammation and infection. High ferritin levels can mean you have an infection or cancer. Imaging tests like X-rays or MRIs check for damage from the disease.
Ruling Out Other Conditions
Doctors must rule out other possible causes of symptoms. They might do more blood tests to check for things like anti-CCP or RF antibodies. The aim is to get enough info for a correct diagnosis and treatment plan.
“The majority of patients diagnosed with serious autoimmune diseases faced significant challenges in getting a correct diagnosis.”
Getting a diagnosis for autoimmune diseases can take a long time and be hard for patients. It’s important to keep trying and work with your doctors to get through this tough process.
Treatment and Management
There is no cure for autoimmune diseases, but we can control symptoms and prevent damage. Doctors often use medications like corticosteroids and immunosuppressants first. These help reduce the immune system’s overactivity and lessen inflammation. Sometimes, therapies like plasma exchanges or stem cell transplants are used too.
Medications and Therapies
Immunotherapy targets proteins that cause inflammation in conditions like rheumatoid arthritis. It also treats issues like thyroid hormone or vitamin B12 shortages with supplements. But, using these medicines for a long time can raise the risk of infections and cancers.
New treatments like costimulatory blockade and regulatory T cell therapy are promising. They help manage autoimmune diseases by controlling T cell activity and boosting regulatory T cells. Researchers are also looking into antigen-induced tolerance and the interleukin-2 pathway to better manage autoimmune responses.
Symptom Management Strategies
Patients with autoimmune diseases can also make lifestyle changes to feel better. This includes managing stress, eating well, and exercising regularly. Some people try alternative therapies like acupuncture or Reiki to help with symptoms.
Practices like yoga and meditation can also help. They improve pain, flexibility, and muscle strength in people with autoimmune diseases. Supplements like curcumin and vitamin D might also help control inflammation and support the immune system in some cases.

“Integrating a combination of medical treatments, lifestyle modifications, and complementary therapies can be an effective approach in managing the symptoms and progression of autoimmune diseases.”
Treatment Approach | Potential Benefits |
|---|---|
Medications (Corticosteroids, Immunosuppressants, Biologics) | Reduce immune system overactivity, minimize inflammation |
Therapies (Plasma Exchange, Stem Cell Transplant) | Address specific immune system imbalances |
Lifestyle Changes (Stress Management, Healthy Diet, Exercise) | Alleviate symptoms, improve overall well-being |
Complementary Therapies (Acupuncture, Cupping, Hydrotherapy) | Potential to manage symptoms and enhance quality of life |
Mind-Body Interventions (Yoga, Meditation) | Improve pain perception, joint flexibility, muscle strength |
Nutritional Supplements (Curcumin, Vitamin D) | Regulate inflammation, support immune function |
Managing autoimmune diseases needs a mix of medicines, therapies, and lifestyle changes. This approach helps control symptoms, prevent damage, and improve well-being. Using a mix of these strategies can help manage the challenges of autoimmune disorders.
Conclusion
Autoimmune diseases are complex and attack the body’s own cells. They happen when the immune system gets mixed up. Genetic and environmental factors are key to their cause. These diseases can hit different parts of the body, causing many symptoms that change life a lot.
There’s no cure for autoimmune diseases, but treatments have gotten better. Doctors now know more about these conditions. This means they can help manage symptoms and slow the disease down. By spreading awareness and doing more research, people with autoimmune disorders get the support they need to live better.
The main points from this article are clear. Autoimmune diseases are complex and need a mix of genetic and environmental factors to understand. They require a detailed approach to manage and treat. Thanks to ongoing research, people with autoimmune diseases have hope and new ways to handle their health.
FAQ
What are autoimmune diseases?
Autoimmune diseases happen when the immune system attacks healthy cells in the body. They can affect many parts like joints, skin, nerves, and organs.
What causes autoimmune diseases?
They are caused by a problem in the immune system. The body’s defense system starts to attack its own cells. This leads to the production of autoantibodies that harm the body’s tissues.
What are the common symptoms of autoimmune diseases?
Symptoms include fatigue, dizziness, low-grade fever, muscle aches, and swelling. These can be confused with other conditions. Many autoimmune diseases have periods of flare-ups and remission.
What are some of the most common autoimmune diseases?
Common ones are rheumatoid arthritis, lupus, multiple sclerosis, type 1 diabetes, and inflammatory bowel diseases. Others include Graves’ disease, Hashimoto’s thyroiditis, and psoriasis.
What are the risk factors for autoimmune diseases?
Risk factors include genetics, environmental triggers like infections or chemicals, being female, and a family history of these disorders.
How are autoimmune diseases diagnosed?
Diagnosing them is tough because symptoms can be similar to other conditions. Doctors start by taking a detailed medical history and doing blood tests and imaging to look for autoantibodies and damage.
How are autoimmune diseases treated?
There’s no cure, but treatments can help manage symptoms and prevent damage. Doctors often use medications like corticosteroids and immunosuppressants. Making lifestyle changes, like managing stress and exercising, can also help.