FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Macular degeneration, a major cause of vision loss, affects millions globally, with age-related macular degeneration (AMD) being the most common form.
It exists in two primary types: wet and dry. The wet form is characterized by abnormal blood vessel growth beneath the retina, leading to leakage and vision impairment. Conversely, dry AMD involves the gradual thinning of the macula as part of the aging process.
Understanding these differences is crucial, as they dictate varying treatment approaches and patient prognoses. This article aims to demystify the distinctions between wet and dry macular degeneration, providing readers with a clear, scientific exploration of their impacts on vision and potential interventions.
The prevalence of this condition underscores the importance of recognizing symptoms early and seeking professional diagnosis and care.
- Wet AMD: Abnormal blood vessels damage vision through growth and leakage.
- Dry AMD: Macular thinning over time, potentially leading to geographic atrophy and severe vision loss.
Understanding Wet Vs Dry Macular Degeneration
Macular degeneration, a leading cause of vision loss, comes in two primary forms: wet (neovascular) and dry (atrophic).
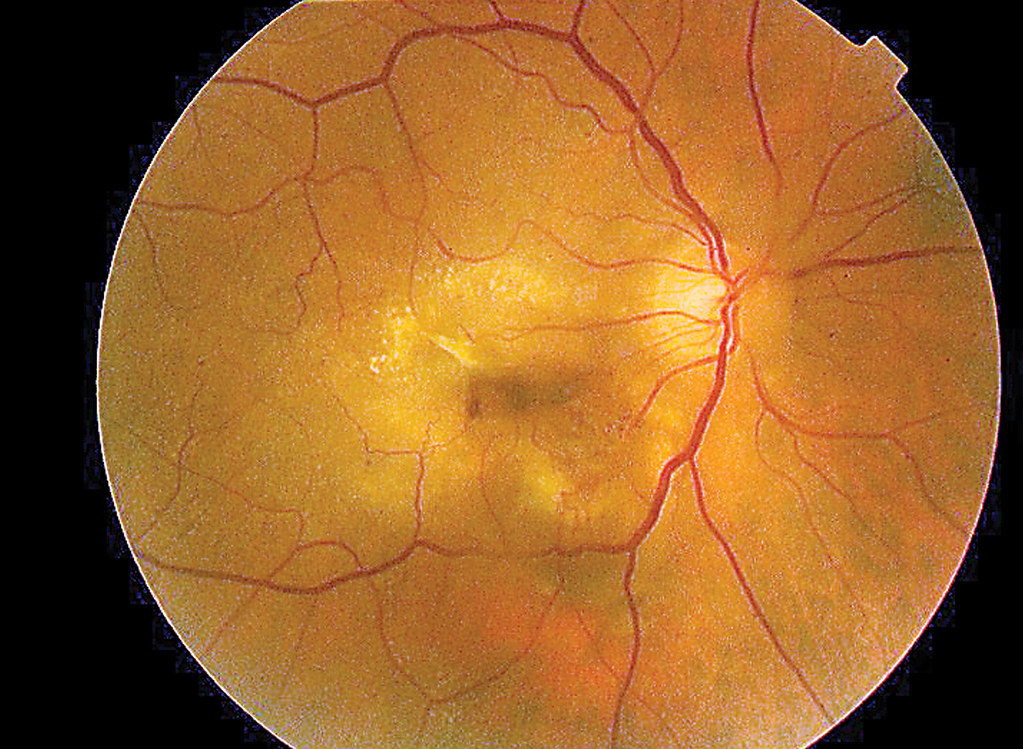
Dry macular degeneration is characterized by the presence of drusen—yellow deposits under the retina—and typically leads to a gradual loss of vision.
Conversely, wet macular degeneration involves the growth of abnormal blood vessels underneath the retina, which can leak fluid and cause rapid and serious vision impairment.
The key differences between these conditions lie in their progression and impact on vision. Dry AMD is more prevalent, accounting for about 90% of cases, yet it is often less severe.
On the other hand, wet AMD, though less common, is responsible for approximately 90% of severe vision loss related to the disease.
Symptoms of wet AMD can include distorted vision and blind spots, while dry AMD may present as a gradual blurring of central vision.
Understanding and early detection of these conditions are critical, as over 10 million individuals in the United States are affected by age-related macular degeneration.
Addressing lifestyle factors, such as smoking cessation and maintaining healthy blood pressure and cholesterol levels, can be instrumental in managing the risk and progression of both forms of macular degeneration.
Risk Factors and Prevention
Preventing the progression of macular degeneration, both wet and dry, hinges on understanding the risk factors and implementing preventive measures.
Age is the most significant risk factor, particularly affecting those over 60, leading to the term age-related macular degeneration (AMD). Other risk factors include a family history of the condition, smoking, high blood pressure, and obesity.
Early Detection and Eye Health
- Undergoing routine eye exams is vital for early detection and management of AMD.
- Protecting eyes from ultraviolet light and quitting smoking can also reduce risk.
Nutrition’s Role in Prevention
- A diet rich in leafy greens and fish provides nutrients like lutein and omega-3 fatty acids that are beneficial for eye health.
- Supplementing with specific vitamins and minerals, as suggested by the AREDS2 study, may slow disease progression.
Implementing these strategies can contribute to preserving good vision and potentially delaying the onset or progression of both dry and wet macular degeneration.
Diagnosing Wet and Dry Macular Degeneration
Diagnosing macular degeneration involves a deep dive into the eye’s inner landscape. For starters, the appearance of drusen, yellow deposits beneath the retina, can be a telltale sign of early-stage dry macular degeneration.
As the condition advances, the macula may suffer from atrophy, leading to a loss of light-sensitive cells. To detect changes in central vision, eye specialists may employ an Amsler grid, where distorted lines or a central blind spot can indicate disease progression.
Additional diagnostic tests include fluorescein angiography and indocyanine green angiography, which involve dye injections to highlight eye blood vessels for photographic examination.
Optical coherence tomography is another noninvasive tool that provides detailed images of the retina to identify swelling or other changes.
Common symptoms flagging the presence of macular degeneration range from blurred vision and difficulty perceiving colors to challenges with depth perception and adaptation to light changes.
Wet macular degeneration, the more severe form, can cause rapid central vision loss and make straight lines appear wavy.
Recognizing these symptoms is crucial, as early consultation with a doctor can lead to interventions that may slow disease progression and preserve vision.
Therefore, regular eye exams are essential for early detection and management of macular degeneration.
Treatment Options for Wet and Dry Macular Degeneration
When it comes to macular degeneration, the treatment battlefield is divided into two camps: dry and wet forms of the disease.
For those grappling with the more common dry macular degeneration, options are currently limited.
One beacon of hope is the AREDS2 supplement, a cocktail of vitamins and minerals that may decelerate the disease’s march during intermediate stages. Advanced dry AMD may be addressed with Syfovre, targeting geographic atrophy.
The wet form, characterized by rogue blood vessels, allows for a more aggressive treatment strategy. Anti-VEGF drugs such as Bevacizumab and Ranibizumab are injected directly into the eye, potentially improving vision by cutting off the growth of these vessels.
Although this treatment can be a game-changer, it’s not without risks, including infection or increased eye pressure. Less frequently, photodynamic therapy steps in as an alternative.
Without intervention, macular degeneration can lead to significant visual decline. However, the silver lining lies in the strides being made in treatment advancements. Ongoing clinical trials continue to promise new horizons in managing this vision-stealing ailment.
Coping with Macular Degeneration
When macular degeneration enters one’s life, it brings not just a blur in vision but also an emotional fog for those affected and their close circles. The condition can significantly alter daily routines, challenging individuals with tasks that were once effortless.
Emotional impacts such as anxiety and depression are common as individuals grapple with the loss of independence that comes with visual impairment. Practical impacts include difficulty reading, driving, and recognizing faces.
To navigate these murky waters, coping strategies are essential. Adaptation is key, such as using assistive technologies designed for low vision, increasing home safety to prevent falls, and modifying tasks to remain as autonomous as possible.
Maintaining a good quality of life also involves regular exercise, a healthy diet, and possibly vision rehabilitation.
One should never underestimate the power of support. Leaning on medical professionals for guidance, tapping into resources like the BrightFocus Foundation, and joining support groups can provide both practical advice and emotional solace.
These resources serve as lighthouses, offering direction and hope amidst the challenges of living with macular degeneration.
Expert Perspectives from Chicago
The “Windy City” bears witness to some of the foremost advancements in combating eye disease. Macular degeneration, a condition all too familiar in the corridors of Chicago’s medical institutions, is under the microscope of some of the most innovative minds in eye care. Experts from renowned
Midwest Eye Centers and the Eye Center of Texas share a common goal: to turn the tide against this vision-stealing ailment.
In a city famed for its architectural marvels, these doctors are constructing their own masterpieces in the form of cutting-edge treatments for both wet and dry macular degeneration.
They emphasize the importance of early stages diagnosis and staying abreast of the latest news in treatment methods.
One such method gaining attention is the use of anti-vascular endothelial growth factor (anti-VEGF) drugs for wet AMD, which target the abnormal blood vessels that characterize this type of condition.
Continuous research and clinical trials in Chicago’s medical community aim to refine these treatments, offering a beacon of hope for those grappling with the prospect of serious vision loss.
As they conduct in-depth studies into the inner workings of dry and wet macular degeneration, their collective efforts are a testament to the city’s dedication to advancing ocular health.
Conclusion
Distilling the essence of wet versus dry macular degeneration, we uncover that the former involves abnormal blood vessels that leak beneath the retina, while the latter is characterized by the gradual thinning of the macula due to aging.
The stakes are high, as these conditions are leading causes of vision loss in older adults. Understanding the nuances between them is crucial, as they each have distinct symptoms, progression rates, and treatments.
For dry AMD, a regimen of specific vitamins may slow deterioration, whereas wet AMD may require drugs to halt blood vessel growth.
It’s imperative for individuals to recognize early symptoms—like blurred vision or wavy lines—and seek medical advice promptly to preserve sight.
Embracing a healthy lifestyle, including smoking cessation and regular exercise, can be proactive measures against AMD. Ultimately, proactive prevention and management strategies are key to maintaining optimal eye health.
Contacting a Doctor for More Information
When facing the complexities of macular degeneration, reaching out to a medical professional is a crucial step in navigating your condition.
Whether you’re grappling with the more common dry AMD, characterized by the thinning of the macula, or the more severe wet AMD with its rapid vision loss due to abnormal blood vessel growth, a specialist’s guidance is invaluable.
To connect with a knowledgeable eye care professional, consider scheduling a comprehensive dilated eye exam with an optometrist or an ophthalmologist, who can offer a precise diagnosis and treatment options.
- Prepare a list of symptoms and any medications you’re taking ahead of your appointment.
- Enlist a friend or family member to accompany you, as dilated pupils may temporarily impair your vision.
- Compile a set of pertinent questions for your doctor regarding your diagnosis, safety concerns such as driving, and potential treatments.
Effective communication with your eye doctor can illuminate the path to maintaining your vision and quality of life despite the challenges posed by macular degeneration.