FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
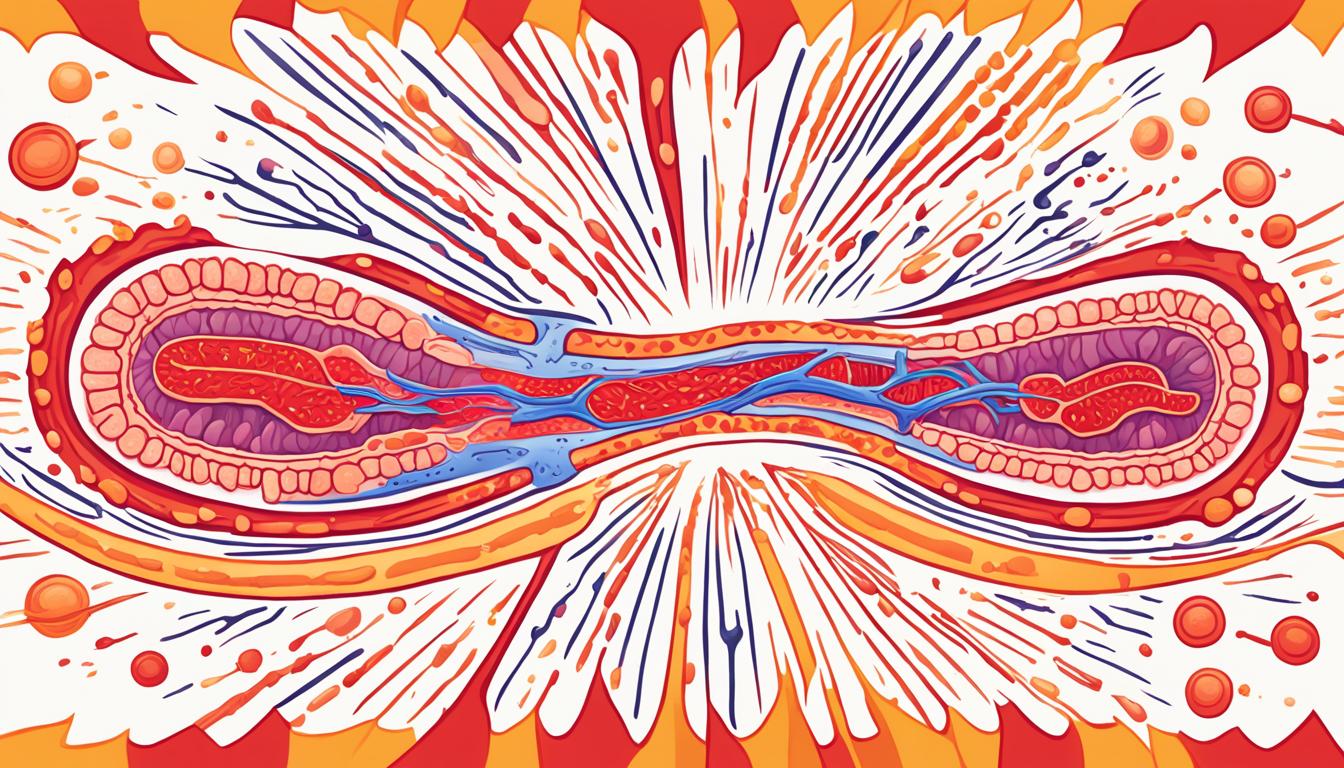
About 1 million Americans live with ulcerative colitis. This is a serious condition that affects the large intestine’s lining. It causes ongoing inflammation and ulcers, greatly affecting life quality. It leads to bad gut symptoms and raises the risk of serious problems.
Ulcerative colitis is hard to understand because we don’t know what causes it. It might be related to an immune issue, genes, and the environment. Knowing what causes it helps us find better treatments for those who have it.
Key Takeaways
- Ulcerative colitis is a chronic inflammatory bowel disease that affects the lining of the large intestine.
- It is estimated that around 1 million Americans are living with ulcerative colitis, making it the most common form of inflammatory bowel disease.
- The exact cause of ulcerative colitis is unknown, but it may involve an abnormal immune response and genetic factors.
- Symptoms can include diarrhea, bloody stools, abdominal pain, fatigue, and weight loss.
- Diagnosis involves a combination of medical history, blood tests, stool tests, and endoscopic procedures.
What is Ulcerative Colitis?
Ulcerative colitis is a long-term condition that affects the colon’s lining. It causes inflammation and ulcers in the colon. It usually starts at the rectum and moves to the left side of the colon. Sometimes, it can affect the whole colon, known as extensive colitis or pancolitis.
There are different types of ulcerative colitis, each with its own symptoms and how much the colon is affected. These include ulcerative proctitis, proctosigmoiditis, left-sided colitis, pancolitis, and acute severe ulcerative colitis. It’s a kind of inflammatory bowel disease (IBD), which also includes Crohn’s disease.
Crohn’s colitis can affect any part of the gut from mouth to anus. It may have healthy tissue between inflamed areas, unlike ulcerative colitis. Microscopic colitis is another type linked to autoimmune diseases. It needs a microscope to diagnose.
People between 15 and 30 years old are more likely to get ulcerative colitis. Symptoms can be different and may include diarrhea, blood in stool, and stomach pain.
Causes of Ulcerative Colitis
The exact cause of ulcerative colitis is still a mystery. Researchers think it’s due to a mix of immune system issues, genes, and the environment. Knowing these factors helps us understand this chronic bowel disease better.
Immune System Dysfunction
Ulcerative colitis starts with an immune system problem. Normally, the immune system fights off bad stuff. But in this case, it attacks the colon lining instead. This leads to ongoing inflammation and symptoms.
Genetic and Environmental Factors
Genes play a big part in getting ulcerative colitis. If you have a family member with it, your risk goes up to 1.6% to 30%. Some genes make you more likely to get it.
Things like diet, stress, and infections can also start ulcerative colitis. These things can work with your genes and immune system to cause inflammation in the gut.
“The exact cause of ulcerative colitis remains a mystery, but researchers are making progress in understanding the complex interplay of immune system dysfunction, genetic factors, and environmental triggers that contribute to this chronic condition.”
We don’t fully get why ulcerative colitis happens yet. But research is helping us learn more about it. By looking at how the immune system, genes, and environment work together, doctors can find new ways to treat it.
Risk Factors for Ulcerative Colitis
Ulcerative colitis is a complex condition with many risk factors. About a million Americans have it, making it the top inflammatory bowel disease in the U.S. It usually starts before people turn 30, and family history and ethnicity matter a lot.
If you have a family member with ulcerative colitis, you’re more likely to get it. Having a first-degree relative with it can raise your risk by up to 30%. People of Ashkenazi Jewish descent are even more at risk.
Diet and stress don’t directly cause ulcerative colitis, but they can make symptoms worse. Being inactive, smoking, and being around certain bacteria or chemicals can also play a part.
Risk Factor | Increased Risk |
|---|---|
Age | Most people diagnosed between 15-30 or over 60 years old |
Ethnicity | Ashkenazi Jews have the highest risk |
Family History | Up to 30% increased risk if a first-degree relative has ulcerative colitis |
Environmental Factors | Exposure to bacteria, chemicals, and a sedentary lifestyle |
Knowing the risk factors for ulcerative colitis helps with early detection and management.
Symptoms of Ulcerative Colitis
Gastrointestinal Symptoms
Ulcerative colitis mainly shows up with stomach issues. Mild symptoms may include having fewer than four bowel movements a day and sometimes passing blood with stool. For those with more severe cases, symptoms can be worse.
They may have more than six bowel movements a day and pass blood with stool most of the time. In the worst cases, people may have more than 10 bloody bowel movements in a day. Other common symptoms include stomach pain, cramps, and feeling the need to go to the bathroom all the time.
Systemic Symptoms
Ulcerative colitis can also affect the whole body. Symptoms like feeling very tired, having a fever, nausea, or vomiting, and losing weight are more likely if it’s severe or affects more of the large intestine. It usually starts between 15 and 40 years old.
Common symptoms include diarrhea with blood, mucus, or pus, stomach pain, and going to the bathroom a lot. In bad cases, people may feel short of breath, have a fast or uneven heartbeat, and a high fever.
It’s important to know the different symptoms of ulcerative colitis. This helps with getting the right treatment fast.

“Severe ulcerative colitis is characterized by experiencing six or more bowel movements per day during an attack.”
Diagnosis of Ulcerative Colitis
Doctors use a detailed approach to diagnose ulcerative colitis. This includes looking at your medical history, doing a physical check-up, and running tests. These tests help find out if you have the condition, how bad it is, and rule out other possible causes of your symptoms.
Blood Tests
Blood tests are key in diagnosing ulcerative colitis. They look for signs of infection and check for anemia, which could mean bleeding in the colon or rectum. Tests also check albumin levels, which might be low with ulcerative colitis, and C-reactive protein, a sign of inflammation.
Stool Tests
Stool tests give clues about your gut’s health. They can spot white blood cells in the stool, which suggests inflammation from ulcerative colitis.
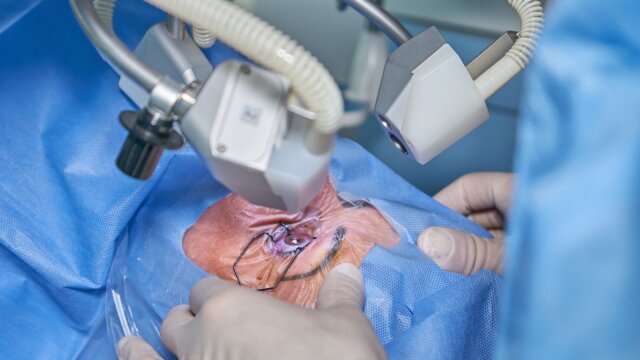
Endoscopic Procedures
Endoscopic tests like sigmoidoscopy and colonoscopy are key for diagnosing ulcerative colitis. Sigmoidoscopy looks at the lower colon and rectum, while colonoscopy checks the whole colon. These tests let doctors see the colon’s condition and take tissue samples for more checks.
Chromoendoscopy is another method that uses a blue dye to highlight changes or polyps in the colon. It’s painless and helps understand how severe the condition is.
Imaging Tests
Tests like X-rays, CT scans, and MRIs help diagnose ulcerative colitis too. X-rays give a detailed view of the gut with the help of a contrast agent. CT scans and MRI show the bowel wall’s condition and help rule out other issues.
Tests for ulcerative colitis usually happen outside the hospital. Doctors might give you brochures to explain the diagnosis and treatment options.
Using these tests together helps doctors accurately diagnose ulcerative colitis. They can then create a treatment plan that fits the patient’s needs.
Ulcerative Colitis Treatment
Managing ulcerative colitis means reducing inflammation and easing symptoms for long-term remission. Doctors use medication, diet changes, and sometimes surgery to help.
Medication Management
For mild to moderate ulcerative colitis, aminosalicylates like mesalamine are first choice. These drugs help keep the condition in check with few side effects. When symptoms get worse, corticosteroids like prednisolone are used to reduce inflammation fast. But, they can make you gain weight and change your mood.
Immunosuppressants, such as azathioprine and tacrolimus, help during flare-ups or to keep the condition in remission. They can raise the risk of infections and anemia. For those with severe cases, biologic therapies target immune system proteins. New treatments like JAK inhibitors and Ozanimod are also available for those who don’t respond to standard treatments.
Dietary and Lifestyle Changes
Along with medicine, changing your diet and lifestyle can help manage ulcerative colitis. Eating soft, bland foods can ease discomfort more than spicy or high-fiber foods. Good nutrition is key to healing and meeting your body’s increased energy needs. Drinking plenty of water and managing stress can also help control symptoms.
Surgical Intervention
If the condition is severe or doesn’t get better with treatment, surgery might be needed. About 25-33% of people with ulcerative colitis might need surgery. Surgery can include removing the colon and creating an ileostomy or internal pouch. These surgeries can be done with laparoscopic or open methods and can stop symptoms.
Handling ulcerative colitis often means using a mix of medication, diet changes, and sometimes surgery. With the help of a healthcare team, people with ulcerative colitis can find a treatment plan that works. This plan helps reduce flare-ups and keeps symptoms under control.
Complications of Ulcerative Colitis
Ulcerative colitis is a chronic condition that causes inflammation in the colon. It can lead to serious problems. One big issue is bleeding from the rectum or colon. This can cause anemia.
It also raises the chance of getting osteoporosis, which makes bones weak. This is a big worry for kids and young people with the condition. It can stop them from growing right.
Ulcerative colitis can also cause inflammation outside the colon. This happens in about 1 in 3 people and can affect joints, skin, or eyes. It can also lead to primary sclerosing cholangitis. This is a rare condition that affects the bile ducts and raises the risk of colon cancer.
In severe cases, it can cause fulminant colitis or toxic megacolon. Fulminant colitis is a sudden, severe form that can make the colon rupture if not treated fast. Toxic megacolon makes the colon very swollen and can also be deadly.
Long-term inflammation from ulcerative colitis also raises the risk of colon cancer. People with it, especially those with a lot of colon involvement, are at higher risk. Regular colonoscopy checks are advised to catch colon cancer early.
In summary, ulcerative colitis can cause many problems like bleeding, anemia, and osteoporosis. It can also lead to serious conditions like fulminant colitis and toxic megacolon. Keeping a close eye on it and getting the right treatment is key to managing these issues and improving health.
Ulcerative Colitis Flare-ups and Remission
Ulcerative colitis is a chronic condition that causes flare-ups and remission. During flare-ups, the colon gets inflamed and ulcers form. This leads to pain, diarrhea, and bleeding. Remission is when symptoms lessen, making life easier. Understanding these cycles is key for managing the condition.
About 90% of people can’t take sulfasalazine but can take mesalamine, which is less likely to cause side effects. A 2022 study showed stress can make flare-ups more likely. Also, probiotics might help control UC symptoms.
Keeping in remission is vital for ulcerative colitis. The Crohn’s & Colitis Foundation says most people have some level of remission each year. Not having enough vitamin D is common in people with IBD, and exercise might help prevent UC.
A 2020 review found curcumin could help keep UC in remission. The goal now is to keep symptoms away and prevent damage. This could also lower the risk of colorectal cancer.
Knowing how to handle flare-ups and remission is important for those with ulcerative colitis. By avoiding stress and certain foods, people can manage their condition better.

“Achieving and maintaining deep remission is a recent focus in the treatment of ulcerative colitis, as it aims to extend the duration of remission and possibly reduce the risk of colorectal cancer.”
Living with Ulcerative Colitis
Living with ulcerative colitis means facing many challenges. It’s key to handle both the physical and emotional sides to improve life quality.
Coping Strategies
Creating good coping strategies helps manage ulcerative colitis better. Stress-reducing activities like yoga, meditation, or deep breathing can lessen flare-ups and ease symptoms. Eating well, staying active, and resting enough also help.
Support Groups
Being in a support group is very helpful for those with ulcerative colitis. These groups offer a place to share challenges and find support from others who get it. It makes people feel less alone and more in control.
Talking to healthcare pros like gastroenterologists and mental health therapists is also key. They can help with managing meds, diet, and mental health.
Remember, dealing with ulcerative colitis is personal. Using coping strategies, finding support, and talking with doctors helps manage the condition and boost well-being.
“Managing ulcerative colitis is a journey, not a destination. With the right tools and support, it’s possible to live a fulfilling life despite the challenges.”
Ulcerative colitis is chronic, but with the right approach, people can manage symptoms and live well.
Coping Strategies | Support Groups |
|---|---|
|
|
Ulcerative Colitis in Children and Adolescents
Ulcerative colitis is a type of inflammatory bowel disease that can affect kids and teens. It mostly hits older kids and young adults. It can affect how they grow and develop. It’s important to understand the challenges they face for better care and support.
It doesn’t favor boys or girls in kids. Kids and teens with this condition go through ups and downs, just like adults do. They often take several medicines together to manage it. Eating right is also key to help them grow and develop well.
Sometimes, surgery is needed if medicines don’t work. Kids and teens with ulcerative colitis need to see a doctor who specializes in gut health for life.
New studies have shed light on how to handle ulcerative colitis in kids. They show the need for a team approach with doctors, nutritionists, and mental health experts to help young patients.
| Key Statistics on Pediatric Ulcerative Colitis |
|---|
| Prevalence of pediatric ulcerative colitis in the US from 2007 to 2016: |
| Rate of colectomy in patients with pediatric-onset ulcerative colitis: |
| Risk factor associated with the development of chronic pouchitis in pediatric ulcerative colitis: |
| Duration of venous thromboembolism in pediatric inflammatory bowel disease: |
| Outcomes prediction in pediatric ulcerative colitis for management optimization: |
Ulcerative colitis is less common in young kids but more in teens. Kids often have worse symptoms than adults. Young patients face a higher risk of getting colorectal cancer, with some having it by age 20. About 40% are at risk by age 35. Some teens might also get arthritis not related to their gut. Regular check-ups are key for kids with a special surgery for colon issues.

Helping kids and teens with ulcerative colitis needs a full team effort. By understanding how the disease affects their growth and health, doctors can better manage it. This helps improve life for young patients and their families.
Emerging Therapies and Research
The field of ulcerative colitis (UC) treatment is always changing. Researchers are looking into new and better ways to handle this inflammatory bowel disease (IBD).
They are looking at things like biologic medications, Janus kinase (JAK) inhibitors, and sphingosine 1-phosphate (S1P) receptor modulators. These could help people with UC feel better and live better lives.
Biologic therapies have changed how we treat UC. These medicines target certain parts of the immune system. They help bring inflammation down and keep it under control. JAK inhibitors are a new kind of pill that stops inflammation. S1P receptor modulators also look promising in studies.
Scientists are still working to understand UC better. They want to find new ways to treat it that work better for everyone. They are looking at new medicines, making old ones better, and checking out things like traditional Chinese medicine and therapy.
New treatments for UC are coming out. In 2023, the FDA approved mirikizumab-mrkz (Omvoh) and etrasimod (Velsipity) for UC. These new options give doctors and patients more choices. With ongoing research, we might see even better ways to manage UC in the future.
As we learn more about UC, we might find treatments that are just right for each person. Doctors and researchers are working hard to make sure people with UC get the best treatments.
Prevention of Ulcerative Colitis
The exact cause of ulcerative colitis, an inflammatory bowel disease, is still unknown. But, some lifestyle and diet choices might help prevent it. Eating well and staying active can lower the risk of getting ulcerative colitis. Also, managing stress and avoiding certain foods might help prevent it.
If you have a family history or other risk factors for ulcerative colitis, taking steps early is key. A healthcare provider can help make a plan to keep you healthy. Catching the disease early can stop it from getting worse.
There’s no sure way to stop ulcerative colitis from happening. But, living a healthy life can help. This includes:
- Eating a Mediterranean or anti-inflammatory diet
- Being active
- Staying calm
- Not smoking or drinking too much alcohol
These habits can lower the risk and keep your gut healthy. Being proactive can make a big difference.

Even with these steps, there’s no guarantee you won’t get ulcerative colitis. If you’re at risk, talk to your doctor about how to stay healthy.
Preventive Measure | Potential Benefits |
|---|---|
Balanced, anti-inflammatory diet | Reduces inflammation and gut imbalance |
Regular exercise | Decreases inflammation, strengthens intestinal lining, and boosts gut microbiome |
Stress management | Reduces systemic inflammation and positively impacts gut health |
Avoiding processed foods, red meats, and refined carbohydrates | Reduces inflammation and gut imbalance |
By doing these things, you can lower your risk of getting ulcerative colitis and stay healthy. But, always talk to a doctor for advice and to manage any risk factors.
“Maintaining a healthy lifestyle and addressing known risk factors can significantly reduce the likelihood of developing ulcerative colitis, though there is no guaranteed way to completely prevent the condition.” – Dr. Elizabeth Mayer, Gastroenterologist
Conclusion
Ulcerative colitis is a chronic condition that affects many people’s lives. There’s no cure, but new treatments and research help manage it better. Working with doctors, changing habits, and getting support can help those with ulcerative colitis live better lives.
The number of people with ulcerative colitis is growing, possibly because of our modern lifestyle and diet. But, thanks to ongoing research, there’s hope for better treatments. This means people with this chronic condition can manage their symptoms and live better.
Dealing with ulcerative colitis is tough, but things are looking up. By working together with healthcare teams and keeping up with new research, people with ulcerative colitis can take charge of their health. This helps them improve their lives and feel better.
FAQ
What is ulcerative colitis?
Ulcerative colitis is a disease that causes inflammation and ulcers in the large intestine, or colon. It’s a chronic condition.
What are the types of ulcerative colitis?
There are different types of ulcerative colitis. These include ulcerative proctitis, proctosigmoiditis, left-sided colitis, pancolitis, and acute severe ulcerative colitis. Each type has its own symptoms and how much of the colon it affects.
What causes ulcerative colitis?
We don’t fully know what causes ulcerative colitis. But it seems to involve an immune system problem. Genetics and environment might play a part too.
What are the risk factors for developing ulcerative colitis?
Being older, certain ethnicity, and having a family history increase your risk of getting ulcerative colitis.
What are the common symptoms of ulcerative colitis?
Symptoms include diarrhea, often with blood or pus, and stomach pain. You might also feel rectal pain and bleeding. There’s a constant urge to go to the bathroom. You could also feel feverish, tired, lose your appetite, lose weight, and get anemia.
How is ulcerative colitis diagnosed?
Doctors use your medical history, physical check-up, blood tests, stool tests, and endoscopies to diagnose ulcerative colitis. Endoscopies include colonoscopy or flexible sigmoidoscopy.
How is ulcerative colitis treated?
Treatment aims to reduce inflammation and ease symptoms. It includes medicines, diet changes, and sometimes surgery.
What are the potential complications of ulcerative colitis?
Complications can include bleeding, anemia, osteoporosis, dehydration, and inflammation in other organs. There’s also a higher risk of liver disease and colon cancer.
How do ulcerative colitis flare-ups and remission periods work?
Ulcerative colitis is chronic, with ups and downs in symptoms. Understanding these cycles is key to managing the condition.
How can individuals cope with ulcerative colitis?
Living with ulcerative colitis means managing physical and emotional challenges. This includes stress management, diet changes, staying active, and getting support from doctors and groups.
How does ulcerative colitis affect children and adolescents?
Kids and teens with ulcerative colitis face challenges to their growth and development. They need a team of doctors, nutritionists, and mental health experts to help them.
What are the emerging therapies and research for ulcerative colitis?
Researchers are exploring new treatments like biologics, JAK inhibitors, and S1P receptor modulators. These could help manage symptoms and achieve remission.
Can ulcerative colitis be prevented?
There’s no sure way to prevent ulcerative colitis. But eating well, exercising, and managing stress might lower your risk, especially if you have a family history.