FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
About 1.25 million Americans have type 1 diabetes. This condition harms the cells that make insulin in the pancreas. It’s a big challenge for those who have it. Type 1 diabetes usually starts in kids and young adults, but it can happen to anyone. Without the right treatment, it can cause serious problems. But, thanks to new treatments, people with type 1 diabetes can live better lives.
Key Takeaways
- Type 1 diabetes is a chronic condition that affects the insulin-producing cells in the pancreas.
- It often develops in children and young adults but can occur at any age.
- Lifelong insulin therapy is generally required to manage the condition.
- Advancements in technology, such as insulin pumps and continuous glucose monitoring, have improved the treatment of type 1 diabetes.
- While there is no known cure, proper management can help prevent complications and improve everyday life for those living with type 1 diabetes.
What is Type 1 Diabetes?
Type 1 diabetes is an autoimmune disorder. It happens when the body’s immune system attacks the insulin-producing cells in the pancreas. This means the pancreas can’t make enough insulin. Insulin is key for controlling blood sugar levels.
Without insulin, glucose builds up in the blood. This can lead to high blood sugar levels and serious health problems.
Type 1 diabetes can start at any age, but it’s most common in kids and young adults. In people with this type, the pancreas doesn’t make much insulin. This leads to high glucose levels in the blood. It’s an autoimmune disorder, meaning the immune system attacks the cells that make insulin.
How Type 1 Diabetes Affects the Body
Symptoms include feeling very thirsty, hungry, and tired, and having blurry vision. You might also feel numb in your feet, lose weight without trying, and need to go to the bathroom a lot. Serious signs include deep, fast breathing, dry skin, and a fruity smell from your mouth.
Other signs include nausea, vomiting, and stomach pain. Low blood sugar can make you feel weak, shaky, and sweaty.
Diagnostic Tests for Type 1 Diabetes | Criteria for Diagnosis |
|---|---|
Fasting Blood Glucose | ≥126 mg/dL |
Oral Glucose Tolerance Test (OGTT) | 2-hour blood glucose ≥200 mg/dL |
Hemoglobin A1C | ≥6.5% |
Random Blood Glucose | ≥200 mg/dL with symptoms |
People with type 1 diabetes often have high levels of antibodies against pancreas proteins. This shows it’s an autoimmune disorder, different from other diabetes types.
“Type 1 diabetes is an autoimmune disorder where the body’s immune system mistakenly destroys the insulin-producing beta cells in the pancreas.”
Causes of Type 1 Diabetes
The exact cause of type 1 diabetes is still a mystery. But, it’s thought to be an autoimmune disorder. In this condition, the immune system attacks the insulin-producing cells in the pancreas. Having a family history also matters, as it can raise your risk.
Other factors like viruses or environmental triggers might also start the autoimmune response. But, eating habits and exercise don’t directly cause type 1 diabetes. Yet, they can affect how the disease progresses.
Type of Diabetes | Percentage of People Affected | Prevalence in U.S. |
|---|---|---|
Type 1 Diabetes | 5-10% of all diabetes cases | More common in White individuals compared to African American and Hispanic/Latino individuals |
Type 2 Diabetes | 90-95% of all diabetes cases | Influenced by factors like overweight, obesity, physical inactivity, insulin resistance, and genetics |
Gestational Diabetes | Not applicable | Linked to hormonal changes during pregnancy, genetic predisposition, and excess weight gain during pregnancy |
Some medical conditions, like cystic fibrosis, can also lead to diabetes. Certain medicines can harm the cells that make insulin or mess with insulin’s function, causing diabetes.
To sum up, type 1 diabetes is caused by an autoimmune disorder and genetics. Viruses and other environmental factors might also play a part.
“Type 1 diabetes is a complex condition, and understanding the underlying causes is crucial for effective management and prevention strategies.”
Symptoms of Type 1 Diabetes
Type 1 diabetes often starts suddenly, especially in young people. Common signs include feeling very thirsty, needing to pee a lot, feeling very hungry, losing weight without trying, feeling tired, weak, and having blurry vision. Kids with type 1 diabetes might also have slow-healing cuts and wetting the bed.
If not treated, type 1 diabetes can cause a serious condition called diabetic ketoacidosis (DKA). This includes hard breathing and often getting infections. Some kids might be diagnosed with diabetes while already in DKA, needing to go to the hospital right away.
Type 1 diabetes can happen to anyone, not just kids and young adults. Adults can get it too and might be first thought to have type 2 diabetes.
Finding and treating type 1 diabetes early is key to avoiding serious problems and staying healthy. If your family has a history of type 1 diabetes, you might get tested for islet autoantibodies early.
Some people with type 1 diabetes may have a “honeymoon” period where they make enough insulin on their own. But this doesn’t last forever. Taking insulin is always needed for type 1 diabetes.
There are many ways to help manage type 1 diabetes, like learning, recipes, fitness advice, and support groups. Doctors and nurses also have tools to screen for diabetes, help prevent it, train for school nurses, and guide diabetes care.
Diagnosis of Type 1 Diabetes
Diagnosing type 1 diabetes often means doing blood tests. The A1C test looks at your blood sugar levels over 2-3 months. It’s a good way to see if you have diabetes. You can also do a fasting blood sugar test by not eating for 8 hours before the test. Or, a random blood sugar test can be done at any time, no matter when you last ate.
These tests help tell if you have diabetes and what kind it is. Your doctor might check for autoantibodies in your blood. This shows if your body is attacking itself, which is common in type 1 diabetes. They might also look for ketones in your blood or urine. This could mean you have diabetic ketoacidosis, a serious problem.
Type 1 diabetes usually hits kids and young adults, but it can happen at any age. Symptoms come on fast, in a few days to weeks. Getting diagnosed and treated quickly is key to managing it and avoiding problems.
“In 2016, the U.S. Food and Drug Administration approved a type of artificial pancreas system called a hybrid closed-loop system.”
There have been studies on artificial pancreas devices funded by the NIDDK. They help people with type 1 diabetes manage their disease. The NIDDK also looks into pancreatic islet transplantation for those who can’t control their blood sugar well.
Treatment for Type 1 Diabetes
Insulin Therapy and Delivery Methods
For people with type 1 diabetes, insulin therapy is key. Their pancreas doesn’t make much insulin. So, they need insulin from outside through different ways.
There are many types of insulin, like rapid-acting and long-acting. Each type works at different speeds. You can get insulin through needles, pens, pumps, and new tech like the artificial pancreas.
Keeping blood sugar levels in check is very important. Some people with type 1 diabetes need to take insulin several times a day or use a pump. They also need to check their blood sugar often, using meters or CGM devices.
Insulin can cost a lot, with some types more expensive than others. Sometimes, people with type 1 diabetes take pills like metformin too, especially if they have gestational diabetes.
New ways to give insulin, like pens and pumps, make giving shots easier. These new techs help people with type 1 diabetes manage their condition better and live fuller lives.
Researchers are always working on new insulins and treatments for type 1 diabetes. They aim to make managing diabetes easier and better for everyone.
Blood Glucose Monitoring
Keeping an eye on blood glucose levels is key for managing type 1 diabetes. You can use a traditional blood glucose meter or a continuous glucose monitoring (CGM) device. CGM devices track glucose levels all day with a sensor under the skin. They alert you if levels get too high or too low.
Checking blood sugar all day helps keep levels healthy. This prevents serious issues like hypoglycemia and hyperglycemia.
Importance of Monitoring
Checking blood glucose often is vital for those with type 1 diabetes. The American Diabetes Association says to test at least four times a day. If you use an insulin pump or are pregnant, you might need to test more.
Keeping blood sugar in check can stop or slow down serious problems. These include nerve damage, kidney disease, and heart issues.
It’s important to check your blood glucose meter’s accuracy now and then. If readings are off by more than 15%, there might be a problem. Things like the type of strip, expired strips, and some medicines can affect readings.
Continuous Glucose Monitoring (CGM)
CGM devices give a full view of blood glucose levels day and night. They use a sensor under the skin for real-time data and alerts. CGM is great for those with a lot of hypoglycemia or big changes in glucose levels.
Some CGM systems last 180 days, while others need a new sensor every 7 to 14 days. They’re usually accurate but sometimes need a fingerstick for calibration. Many devices let you share glucose levels with others, which can be really helpful.
By watching blood glucose closely, people with type 1 diabetes can manage their diabetes better. This lowers the risk of problems and improves health and happiness.
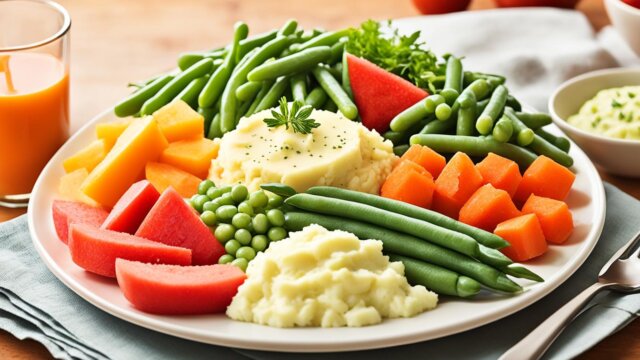
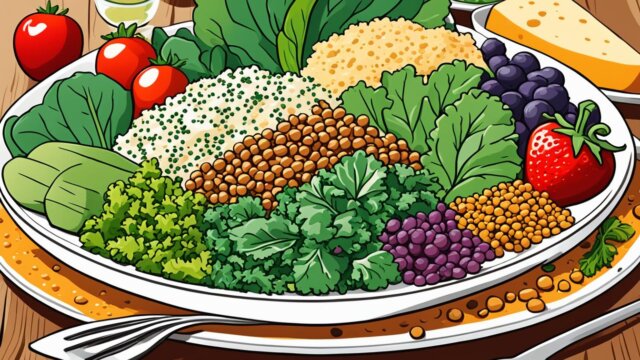
Carbohydrate Counting and Diet Management
For people with type 1 diabetes, managing their diet is key. They must count carbs in their meals and snacks to keep their blood sugar stable. Those with type 1 or some type 2 diabetes on intense insulin therapy use a ratio to control their blood sugars.
Carb counting means tracking carbs in what you eat and drink. Most with type 1 diabetes eat 150-250 grams of carbs a day, making up 45-65% of their calories. Packaged foods have labels that show how many carbs they have, helping with counting.
Keeping a healthy diet is vital for blood sugar control. Carbs are the main energy source and include many foods like fruits, dairy, and sugars. Eating a lot of fiber (25 to 30 grams daily) helps keep blood sugar stable and meets A1C goals.
Diabetes education helps figure out how many carbs you need and when to eat them. Keeping track of what you eat and your blood sugar before and after meals helps see how foods affect you.
Using carb counting and a balanced diet helps manage blood sugar in type 1 diabetes.
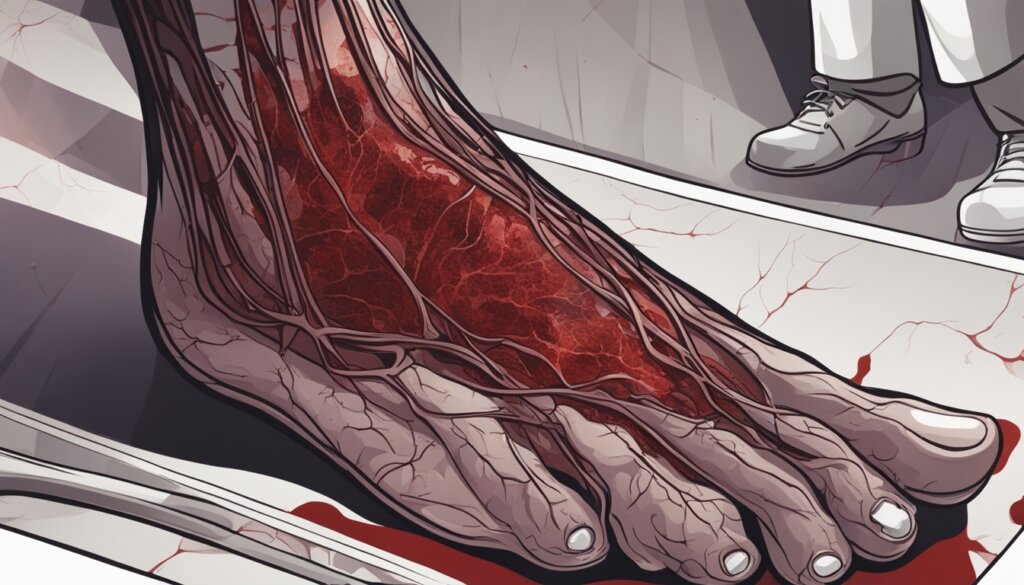
Complications of Type 1 Diabetes
If not managed well, type 1 diabetes can cause serious problems. Diabetic ketoacidosis, a dangerous condition from not having enough insulin and hypoglycemia, very low blood sugar, are big risks. Over time, it can lead to nerve damage, kidney disease, heart disease, and vision loss. Keeping blood sugar under control is key to avoiding these issues.
Potential Long-Term Complications
Nerve damage, or diabetic neuropathy, can cause numbness, pain, and tingling. Diabetes also raises the chance of kidney disease, which could lead to kidney failure if not treated. People with type 1 diabetes are more likely to get heart disease and stroke. Diabetic retinopathy can cause vision problems and even blindness.
Complication | Description |
|---|---|
Nerve Damage | Numbness, pain, and tingling in various body parts |
Kidney Disease | Can lead to kidney failure if left untreated |
Heart Disease | Increased risk of heart disease and stroke |
Vision Loss | Diabetic retinopathy can lead to sight problems and blindness |
Living a healthy life and seeing the doctor regularly are key to managing type 1 diabetes and lowering risks. Working with doctors and sticking to a treatment plan helps reduce the effects of these problems. This way, people with type 1 diabetes can live a better life.
“Proper management of type 1 diabetes is key to preventing or delaying the onset of serious complications.” – Dr. Jane Doe, Endocrinologist
Type 1 Diabetes in Children and Adolescents
Children and teens often get type 1 diabetes. As a pediatric endocrinologist, I know the challenges they face. Type 1 diabetes can start at any age, especially between ages 5 to 7 and during puberty. More cases happen in fall and winter.
It’s hard to manage type 1 diabetes in kids and teens because of growth and hormonal changes. They need to work closely with their pediatric endocrinologist. This doctor specializes in diabetes and other hormone-related conditions. The child’s medical team and family must also support them for the best care.
More boys and men get type 1 diabetes. In the U.S., about 20 to 30 new cases are found per 100,000 people each year. Over 1.25 million people have it, with about 500,000 being kids.
Family history and genes affect the risk of type 1 diabetes in kids. If a parent or sibling has it, the risk goes up. Certain genes make it more likely too. It’s more common in white kids in the U.S. than in other groups.
Type 1 diabetes can cause serious problems in kids, like heart and nerve damage. Research aims to stop or delay it and protect islet cells.
I’m committed to helping kids and teens with type 1 diabetes. With the right care, they can live healthy lives despite the challenges.
Living with Type 1 Diabetes
Living with type 1 diabetes means making big changes in your life. You’ll need to check your blood sugar often and might need to do it at night too. Eating right, exercising, and taking insulin are key to keeping your blood sugar stable.
Joining diabetes education programs and support groups is a big help. They offer advice and support for you and your family. These groups help you understand your condition, manage daily life, and deal with the emotional side of having a chronic illness.
Addressing Mental Health Challenges
Type 1 diabetes can really affect your mental health. It can make you feel down more often. Getting help from mental health experts is important for dealing with these feelings.
| Key Considerations for Living with Type 1 Diabetes |
|---|
| Closely monitoring blood sugar levels and administering insulin |
| Maintaining a healthy diet and regular exercise routine |
| Participating in diabetes education programs and support groups |
| Addressing mental health challenges and seeking professional support |
By making these lifestyle changes and getting the right support, people with type 1 diabetes can manage their condition well.

“Managing type 1 diabetes is a lifelong journey, but with the right support and resources, individuals can thrive and live fulfilling lives.”
Emerging Treatments and Research
Researchers are working hard to find new treatments for type 1 diabetes. They are looking at islet cell transplantation. This is when they move insulin-making cells from a donor pancreas into someone with type 1 diabetes. This could help control blood sugar levels and might even mean no more insulin shots.
They are also looking at pancreas transplants. But these are risky and usually for people with serious diabetes problems. Scientists are also looking into stem cell therapy. This could lead to an artificial pancreas that can manage blood sugar on its own.
Islet Cell Transplantation and Ongoing Research
Islet cell transplantation is a big hope for a cure. Studies show it’s working well. A drug called DFMO might help keep insulin levels stable in people with type 1 diabetes. Early tests showed it helped, and more studies are proving it’s safe and works well.
DFMO is already approved for other diseases, which could speed up its use for diabetes. If it gets the green light, it could replace insulin shots for some people. More studies are being done to see how well it works for diabetes.
Researchers are also looking at teplizumab, an antibody that might slow down diabetes progression. Early tests look good, offering hope for a new way to manage the disease.
Then there’s VX-880, a stem cell therapy that’s showing big promise. It turns stem cells into islets that can make insulin, possibly ending the need for insulin shots. The early results are very encouraging, showing its huge potential.
The future looks bright for people with type 1 diabetes. These new treatments could mean better lives and maybe even a cure.
Conclusion
Type 1 diabetes is a lifelong condition that needs careful management. But, with the right treatment and support, people with this disease can live full, healthy lives. Insulin therapy, checking blood sugar often, eating right, and staying active are key to managing type 1 diabetes.
Research is looking into new treatments and tech. This includes better insulin delivery, devices to monitor glucose levels, and treatments to fight the disease. These could make life better for people with type 1 diabetes. Also, getting good diabetes education and support helps people understand and manage their diabetes better. This leads to better self-care and overall health.
Type 1 diabetes brings its own set of challenges. But, with the right care, support, and new medical advances, people with this condition can do well. By staying informed, taking care of their health, and using the right resources, those with type 1 diabetes can face their challenges with confidence and strength.
FAQ
What is type 1 diabetes?
Type 1 diabetes is a chronic condition. It affects the insulin-making cells in the pancreas. People with this condition don’t make enough insulin. Insulin is key for cells to store sugar and make energy.
What causes type 1 diabetes?
This type of diabetes is an autoimmune disorder. The body’s immune system attacks the insulin-producing cells in the pancreas. Genetic factors and environmental triggers, like infections or viruses, may also play a role.
What are the symptoms of type 1 diabetes?
Symptoms include increased thirst, frequent urination, and extreme hunger. You might also experience unintended weight loss, fatigue, blurred vision, and mood changes.
How is type 1 diabetes diagnosed?
Doctors use blood tests like the A1C test, fasting blood sugar test, or random blood sugar test to diagnose it. They may also check for autoantibodies and ketones to confirm the diagnosis.
How is type 1 diabetes treated?
People with type 1 diabetes need insulin therapy for life. They can get insulin through injections, pens, or pumps. The amount of insulin depends on their needs.
Why is blood glucose monitoring important for type 1 diabetes?
Monitoring blood glucose levels is key to managing the condition. You can use a traditional meter or a continuous glucose monitoring (CGM) device. These alert you if levels get too high or too low.
How does diet management affect type 1 diabetes?
Keeping track of carbohydrates in food and drinks is crucial. It helps figure out the right insulin dose. People with type 1 diabetes use an insulin-to-carb ratio for this purpose.
What are the potential complications of type 1 diabetes?
Without proper management, it can lead to short-term issues like diabetic ketoacidosis and hypoglycemia. Long-term, it can cause nerve damage, kidney disease, heart disease, and vision loss.
How is type 1 diabetes managed in children and adolescents?
It’s tough to manage in kids and teens because of growth, hormonal changes, and lifestyle changes. Close monitoring, insulin therapy, and support from doctors and family are key for good outcomes.
What kind of support and resources are available for people with type 1 diabetes?
Diabetes education programs and support groups offer great help. They provide guidance and support. It’s also important to address the mental health challenges that come with managing diabetes.
What are some of the emerging treatments and research for type 1 diabetes?
Researchers are looking into new treatments like islet cell transplantation, pancreas transplants, stem cell therapy, and an artificial pancreas. These could improve managing type 1 diabetes.