FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
About 6.2 million people in the U.S. have heart failure, a serious condition. It makes the heart pump blood poorly. This issue is getting worse, with 7 million Americans affected now. Experts say 1 in 4 people might get it at some point.
This article will cover the types of heart failure, its causes, symptoms, and treatments.
Key Takeaways
- Heart failure is a condition where the heart muscle doesn’t pump blood as effectively as it should.
- Coronary artery disease, high blood pressure, and heart attacks are leading causes of heart failure.
- Symptoms of heart failure include shortness of breath, fatigue, swelling, and irregular heartbeat.
- Treatment options include lifestyle changes, medications, and in severe cases, surgical interventions.
- Early diagnosis and proper management are crucial for improving outcomes and quality of life for those living with heart failure.
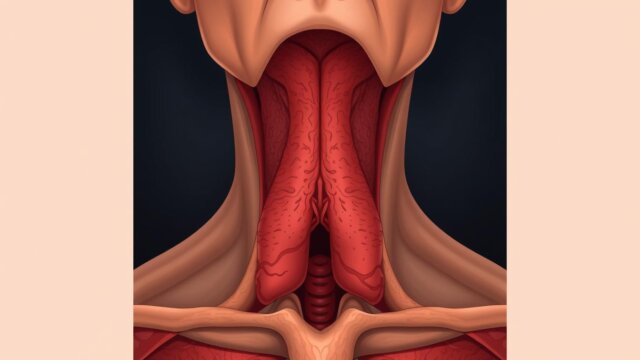
What is Heart Failure?
Overview of Heart Failure
Heart failure, also known as cardiac insufficiency or ventricular dysfunction, is a serious condition. It happens when the heart can’t pump blood well throughout the body. This is because the heart can’t do its job anymore, leading to not enough blood flow.
Even though heart failure can’t be cured, many people manage it well with medicine and a healthy life. Symptoms can be mild or severe. They include feeling short of breath, being very tired, and swelling in the legs and feet.
There are two main types of heart failure: left-sided and right-sided. It can happen to anyone, but it’s more common in people over 65. Things like age, gender, and race can affect how likely someone is to get it.
Factors Affecting Heart Failure Risk | Details |
|---|---|
Gender | Men often develop heart failure at a younger age than women. |
Age | Aging can weaken and stiffen the heart muscle, increasing the risk of heart failure. |
Race | African Americans are more likely to develop heart failure and have more serious cases at younger ages compared to other races. Factors such as stigma, discrimination, income, education, and geographic region can affect the risk of heart failure in African Americans. |
Understanding heart failure is key for both patients and doctors. It helps them manage the condition better and improve life quality for those affected.
Symptoms of Heart Failure
Heart failure can hit the left, right, or both sides of the heart. It’s often a long-term issue but can happen suddenly. Signs include coughing, feeling very tired, not wanting to eat, needing to pee a lot at night, an odd heartbeat, shortness of breath, swelling, and weight gain.
It can strike at any age but is most common in older folks. Some people see acute symptoms come on fast, while others notice chronic symptoms over time, like weeks or months.
Heart failure types are named by where they happen in the heart: left-sided heart failure, right-sided heart failure, and biventricular heart failure (both sides). Left-sided affects the left ventricle and is the top type, causing breathing symptoms. Right-sided affects the right ventricle and leads to swelling from fluid buildup. Biventricular hits both sides, mixing symptoms from the other types.
Acute heart failure comes on suddenly, often from a heart attack or irregular heartbeat. Chronic heart failure builds up over time from issues like high blood pressure or blocked heart arteries. Congestive heart failure means fluid backs up into the body, needing quick medical help.
Keeping an eye on heart failure means regular check-ups, every 3 to 6 months or more. Tests like the ECG and echocardiogram help diagnose and track the condition.
NYHA Functional Classification System | ACC/AHA Classification System |
|---|---|
|
|
There are two main ways to measure heart failure severity: the NYHA and ACC/AHA systems. The NYHA has stages from 1 (no symptoms) to 4 (big limitations and symptoms at rest). The ACC/AHA has stages from A (high risk) to D (not getting better with usual treatment).
Causes of Heart Failure
Conditions Leading to Heart Failure
Heart failure can happen for many reasons. These include coronary artery disease, heart attack, high blood pressure, heart valve disease, myocarditis (heart muscle inflammation), and congenital heart defects. Other causes are arrhythmias (bad heart rhythms), diabetes, HIV infection, thyroid disorders, and iron or protein buildup in the heart.
Bad habits like smoking, being too heavy, eating too much fat and cholesterol, and not moving enough can raise heart failure risk. If someone has had a heart attack before, they’re more likely to get heart failure.
Heart valve issues make the heart work too hard, leading to failure. Diseases like dilated cardiomyopathy, hypertrophic cardiomyopathy, or myocarditis also raise the risk. Congenital heart defects from birth can make heart failure worse by making the heart work too hard.
Sometimes, severe anemia, hyperthyroidism, and abnormal heart rhythms can cause heart failure symptoms that go away once treated.
“22% of cases of heart failure are associated with hypertension, and 41% are attributable to coronary artery disease.”
Other facts show 69% of heart failure cases have hard-to-manage high blood pressure. 13% are due to valvular heart disease, and 8% from cardiomyopathy. About 49% of cases come from other causes.
Genetics, salt intake, and other health issues can also lead to heart failure. Survival and death rates depend on the cause and severity of the heart failure. Heart failure is a big health issue worldwide, especially in places like Sub-Saharan Africa.
Types of Heart Failure
Heart failure can hit the right, left, or both sides of the heart. Right-sided failure causes fluid to gather in the belly, legs, and feet. Left-sided failure leads to fluid in the lungs. There are two main types of left-sided failure: one where the heart can’t pump enough, and another where it can’t fill with blood.
Heart failure types depend on how well the left ventricle pumps. Normally, it pumps 55% to 60% of blood. If it can’t pump well, it’s called systolic failure, with an ejection fraction under 40%. If it can’t fill with blood, it’s called diastolic failure, with an ejection fraction over 50%. There’s also a middle type, pumping between 41% and 49%.
Type of Heart Failure | Ejection Fraction |
|---|---|
Heart Failure with Reduced Ejection Fraction (HFrEF) | ≤ 40% |
Heart Failure with Mid-Range Ejection Fraction (HFmrEF) | 41% – 49% |
Heart Failure with Preserved Ejection Fraction (HFpEF) | ≥ 50% |
There’s also right-sided heart failure. It can happen with advanced left-sided failure or from lung issues like COPD. When both sides fail, it’s called biventricular failure, showing symptoms of both.
Heart failure has four stages: A, B, C, and D. Stage A is for those at risk but without symptoms. Stage B has those with heart disease but no symptoms yet. Stage C has current or past symptoms, and Stage D is for severe symptoms that affect daily life. The NYHA Functional Classification rates heart failure by how much it limits activity, from Class I to Class IV.
Risk Factors for Heart Failure
Conditions and Lifestyle Factors
Heart failure is a serious condition with many causes. Knowing the risk factors helps with prevention and early action. Key conditions include coronary artery disease, heart attacks, and high blood pressure. Diabetes, sleep apnea, and obesity also raise the risk.
Some lifestyle choices increase heart failure risk too. Viral infections can harm the heart muscle. Some diabetes and anti-inflammatory drugs can also raise the risk. Aging, too much alcohol, and smoking are other factors.
Risk Factor | Description |
|---|---|
Coronary Artery Disease | Buildup of plaque in the arteries that supply the heart with blood and oxygen, which can lead to heart attacks and weaken the heart muscle. |
Heart Attacks | Damage to the heart muscle caused by a sudden blockage in a coronary artery, which can impair the heart’s ability to pump effectively. |
High Blood Pressure | Chronic high blood pressure can put strain on the heart and lead to heart failure over time. |
Diabetes | High blood sugar levels can cause damage to the heart and blood vessels, increasing the risk of heart failure. |
Obesity | Excess weight puts additional strain on the heart, making it work harder to pump blood throughout the body. |
Knowing these risk factors and how to manage them can lower the chance of heart failure.
Complications of Heart Failure
If you have heart failure, seeing your doctor often is key, even if you feel better. Not treating heart failure can cause big problems like fluid in the lungs and limbs, damage to organs, more hospital stays, and a higher chance of sudden heart issues. It’s vital to keep an eye on and manage your heart failure to avoid these serious issues.
Pulmonary edema is a big problem with heart failure. It happens when fluid builds up in the lungs, making it hard to breathe. Also, the heart valves can get damaged as the heart gets bigger from pumping harder.
Heart failure can hurt other organs too, like the kidneys and liver. Kidney disease can make heart failure worse by causing fluid buildup and high blood pressure. This can lead to kidney failure, needing dialysis or a new kidney. The liver can also be affected, making it less efficient at cleaning toxins and storing bile.
Anemia is common in heart failure patients and can get worse due to kidney damage. Heart failure can also change how muscles and fat work, leading to weight loss and muscle weakness.
Severe heart failure can be very dangerous if not treated. That’s why it’s important to follow a treatment plan that includes managing weight, eating right, exercising, and taking your medicines. Keeping an eye on and managing heart failure is key to avoiding these bad outcomes and staying healthy.
Diagnosis of Heart Failure
Your doctor will take a detailed medical history and do a physical exam to diagnose heart failure. They might also order tests like blood tests, an echocardiogram, an EKG, a cardiac catheterization, and a stress test.
Tests and Procedures
Blood tests check for heart or kidney issues. A B-type natriuretic peptide (BNP) blood test measures a hormone from the heart. Chest X-rays show the heart’s size and shape. An echocardiogram looks at the heart’s structure and how it works.
An EKG checks the heart’s electrical activity. A cardiac catheterization lets doctors see the heart’s arteries. Stress tests show how the heart does during exercise.
These tests help doctors find out why heart failure is happening and what to do next. Knowing the type and severity of heart failure, doctors can make a plan just for you. This helps improve your life quality.
Management and Treatment of Heart Failure
The main goals in managing heart failure are to ease symptoms, stop it from getting worse, and make life better. Most people with heart failure need a mix of treatments. This includes changing your lifestyle, taking medicines, and sometimes surgery.
Changing your lifestyle is often the first step. This means losing weight, eating foods low in sodium, and exercising regularly through cardiac rehab. Stress management can also help.
Doctors often give medicines to help with heart failure symptoms. These include ACE inhibitors, ARBs, beta-blockers, diuretics, and mineralocorticoid receptor antagonists. These drugs help the heart work better, relax blood vessels, and control fluid levels.
For serious cases, you might need medical procedures or surgery. This could be coronary bypass surgery, fixing heart valves, getting a pacemaker or defibrillator, or a heart transplant. These steps aim to make your heart work better and improve your health.
It’s important to work closely with your healthcare team, no matter the treatment. Regular check-ups, watching your weight, and reviewing medicines help keep your treatment working well.
Handling heart failure needs a full plan that fits your needs and condition. By working with your healthcare providers, you can help manage your symptoms and get better overall.
Living with Heart Failure
Self-Care and Support
Living with heart failure means taking good care of yourself. This means watching your symptoms, taking your medicine, eating right, exercising, and managing stress. Joining a support group can also help you feel less alone and learn how to deal with heart failure.
It’s important to keep in touch with your doctors. Try to see them at least every 6 months to talk about your heart failure and treatment. Also, getting the flu and pneumococcal vaccines can help keep you safe.
Watch how much alcohol you drink. Don’t have more than 14 alcohol units a week. If heart failure makes it hard to work, you might be able to get disability benefits. People caring for someone with heart failure can also get support and benefits.
As heart failure gets worse, planning for the end is important. You might need palliative care. Talking with your doctors about what you want can help make sure you get the care you want.
Living with heart failure is tough, but there are ways to make it easier. By taking care of yourself and getting support, you can live well with this condition.
| Statistic |
|---|
| Regular contact with the GP or care team to monitor heart failure condition at least every 6 months. |
| Offered the annual flu vaccine and the one-off pneumococcal vaccination for individuals with heart failure. |
| Advisable not to exceed the recommended limit of more than 14 alcohol units a week for individuals with heart failure. |
| Disability and sickness benefits may be claimed if one can no longer work due to heart failure. |
| Carers may also be entitled to some benefits when caring for individuals with heart failure. |
| Heart failure usually gets gradually worse over time and may eventually reach a severe stage where palliative care is needed. |
| Planning in advance for care in the terminal stage is recommended for individuals with heart failure. |
| According to the American Heart Association, of the more than 6 million American adults living with heart failure, about 10% have advanced heart failure. |
| Monitoring symptoms and follow-up care are crucial for individuals with heart failure to properly manage the condition. |
| It is mentioned that friends and family may initially feel distant or uncomfortable when dealing with a loved one’s heart failure diagnosis, indicating a potential social challenge that individuals may face. |
| The text highlights the importance of seeking support and recognizing the emotional impact of heart failure on individuals. |
| The significance of gradual return to normal daily activities as a means of managing heart failure symptoms is emphasized. |
| Access to resources for managing heart failure symptoms, including guidance on physical changes to report, caregiver support, and emotional well-being, is recommended. |
Heart Failure: Outlook and Prognosis
Heart failure’s outlook depends on how severe it is, the causes, and how well treatment works. Many people with heart failure can manage their symptoms and live for years with the right care. Studies show that people under 65 have a 5-year survival rate of 78.8 percent after heart failure. Those over 75 have a 5-year survival rate of 49.5 percent.
But, heart failure raises the risk of going to the hospital and dying, especially if it’s severe or getting worse fast. More than half of people with heart failure live 5 years after being diagnosed. About 35% make it to 10 years. Survival depends on things like how well the heart pumps and other health issues.
Checking in regularly and sticking to treatment plans are key to a better outlook and handling symptoms. This might mean making some lifestyle changes, like:
- Staying away from too much alcohol, no more than two drinks a day for men and one for women with CHF
- Keeping an eye on how much fluid you drink, usually no more than 2 quarts a day
- Watching your weight to catch fluid buildup
- Stopping smoking to help with CHF symptoms
- Wearing loose clothes to prevent blood clots
- Handling stress with support and relaxation
Even with heart failure, the right care and management can help people live well for years. Things like age, how well the heart pumps, and other health issues affect survival. This shows why it’s important to keep an eye on things and manage heart failure well.
“The key to improving prognosis for heart failure patients is a combination of early diagnosis, personalized treatment plans, and consistent disease management. With the right care and support, many individuals can lead fulfilling lives despite the challenges of this condition.”
– Dr. Sarah Linder, Cardiologist
Heart Failure Prevention
Not all heart failure cases can be stopped, but you can lower your risk. Keeping a healthy lifestyle with a balanced diet, regular exercise, and avoiding smoking and too much alcohol helps a lot. It’s also key to manage conditions like high blood pressure, coronary artery disease, and diabetes to prevent heart failure. And, always take your medicines as told to keep your heart healthy.
Stopping smoking can make your heart healthier right away. The risk of heart disease goes down a lot within a day of quitting. After a year, it’s almost half the risk of a smoker. Doing at least 150 minutes of moderate exercise each week, like brisk walking, can also lower your heart disease risk. Keeping a healthy weight is important too. Being overweight can lead to high cholesterol and high blood pressure.
Regular check-ups for high blood pressure and high cholesterol can catch heart disease risks early. Managing health issues, sleeping well, and reducing stress can also lower your heart failure risk.
By changing your lifestyle, managing health issues, and following your doctor’s advice, you can help prevent or delay heart failure. These steps can make your heart healthier and lessen the impact of this condition on you and the healthcare system.
Preventive Measure | Impact on Heart Health |
|---|---|
Quitting smoking | Risk of heart disease drops significantly within a day of quitting, and after a year, the risk is about half that of a smoker. |
Regular exercise (150 mins/week) | Lowers the risk of heart disease. |
Maintaining a healthy weight (BMI | Reduces the chances of heart disease by lowering cholesterol and blood pressure levels. |
Regular health screenings | Helps detect and address potential heart disease risk factors early on. |
Managing underlying conditions | Crucial for preventing or delaying the onset of heart failure. |
Adhering to medication as prescribed | Key for maintaining heart health and preventing heart failure. |
“Prevention is better than cure, and that’s especially true when it comes to heart health. By making lifestyle changes and managing underlying conditions, you can take proactive steps to reduce your risk of heart failure and improve your overall well-being.”
Even though you can’t prevent all heart failure, using these strategies every day can really help keep your heart healthy and avoid serious problems.
Heart Failure Research and Advancements
Researchers are working hard to find new ways to treat heart failure. They are looking into new medicines, better devices, and new surgery methods. They also explore stem cell and gene therapies.
Clinical trials are testing these new ways to help the heart work better. They aim to lessen symptoms and improve life for those with heart failure. Groups and research centers are working to better understand and manage this condition.
The AMP HF Study is looking into new treatments for a specific type of heart failure. The Pumps for Kids, Infants, and Neonates trial is testing a heart pump for young ones waiting for a new heart.
The WISE study looks at women with heart issues but no blockages. It aims to understand the risks of heart damage and early death.
The TRANSFORM-HF trial compares two diuretics for heart failure. The UCLA-UCI Center works on health disparities in diverse populations.
The CARDIA study has been going since 1985 to study heart health over time. The Mechanisms of Exercise Intolerance in Heart Failure study looks for the best exercises for heart failure patients.
The HeartShare program aims to find personalized treatments for heart failure. The Avoiding (Heart) Failure study looks at treating people with HIV to prevent heart failure.
High blood pressure has increased by over 30% since the 1990s. It affects nearly half of U.S. adults, but many don’t control their blood pressure well. Taking high doses of Zilebesiran lowered blood pressure in some people.
In China, 456 stroke patients got better after endovascular thrombectomy. In Europe and Canada, 253 patients also saw better outcomes and lower death rates. Using OCT to place stents made sure the stents were big enough and safe for complex heart issues.
“Advancements in medical technologies and research initiatives are crucial in improving the lives of those affected by heart failure. The progress being made in areas like precision treatments, mechanical devices, and cost-effective interventions holds great promise for the future.”
Conclusion
Heart failure is a serious condition that affects millions worldwide. It happens when the heart can’t pump enough blood. This can be due to many reasons like heart disease, high blood pressure, or genes.
But, there’s good news. Thanks to new treatments and management, people with heart failure have better chances now. Treating the main causes, like high blood pressure, and new therapies have made a big difference. We’re also seeing more ways to prevent and manage this disease.
Learning about heart failure helps you take charge of your health. Work with your doctors to get the best care. With self-care, support, and new medical advances, people with heart failure can live better lives.
FAQ
What is heart failure?
Heart failure happens when the heart can’t pump blood well. This leads to blood backing up and fluid in the lungs. It causes shortness of breath.
What are the symptoms of heart failure?
Symptoms include shortness of breath and feeling very tired. You might also have swelling in your legs and feet. Other signs are a fast or uneven heartbeat, trouble doing things you used to do, wheezing, chest pain, and feeling sick to your stomach.
What causes heart failure?
Heart failure can come from conditions that harm the heart. These include coronary artery disease, heart attacks, high blood pressure, and heart valve problems. Some infections or genetic issues can also cause it.
What are the different types of heart failure?
Heart failure can affect the right, left, or both sides of the heart. There are two main types on the left side. They are heart failure with reduced ejection fraction and heart failure with preserved ejection fraction.
What are the risk factors for developing heart failure?
Risk factors include coronary artery disease, heart attack, and heart valve issues. High blood pressure, irregular heartbeats, and diabetes are also risks. Other factors are sleep apnea, obesity, certain medicines, aging, alcohol use, and smoking.
How is heart failure diagnosed?
Doctors diagnose heart failure by looking at your medical history and doing a physical exam. They may also order tests like blood tests, chest X-rays, echocardiograms, EKGs, and stress tests.
How is heart failure treated?
Treatment aims to stop the condition from getting worse and ease symptoms. It includes lifestyle changes, medicines, cardiac rehab, and sometimes surgery or a heart transplant.
How can I manage my heart failure on a daily basis?
Managing heart failure means watching your symptoms, taking your medicines, eating a low-sodium diet, exercising regularly, and managing stress. Joining a cardiac rehab program or support group can also help a lot.
What is the prognosis for someone with heart failure?
The future for people with heart failure depends on how bad it is, the causes, and how well they respond to treatment. Even with heart failure, many people can manage their symptoms and live a long time with the right care. It’s important to follow your treatment plan closely.
Can heart failure be prevented?
Not all heart failure can be prevented, but you can lower your risk. Keep a healthy lifestyle, manage conditions like high blood pressure and diabetes, and take your medicines as told.