FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Did you know endometrial cancer is the most common gynecological cancer in Australia? It starts in the uterus lining and affects thousands yearly. Knowing symptoms, risks, and treatments is key for early detection and better health. We’ll explore endometrial cancer deeply, giving you the knowledge to handle it.
Endometrial cancer often hits women over 50 who have menopause. But it can also affect younger women, transgender males, and intersex people. It has four stages, and symptoms include abnormal bleeding, watery discharge, and weight loss. Other signs are trouble urinating and stomach pain.
Key Takeaways
- Endometrial cancer is the most common gynecological cancer in Australia.
- It primarily affects women over 50 who have gone through menopause but it can also occur in younger individuals.
- Symptoms include abnormal vaginal bleeding, discharge, weight loss, and pelvic pain.
- Early detection and proper treatment are crucial for improving outcomes.
- Treatment options may include surgery, radiation therapy, chemotherapy, and hormone therapy.
What is Endometrial Cancer?
Definition and Overview
Endometrial cancer starts in the lining of the uterus, called the endometrium. It’s the most common cancer in the female reproductive system. In the U.S., it causes about 66,200 new cases each year.
This cancer usually starts in the inner lining of the uterus. Most cases are adenocarcinomas.
The most common type is endometrioid adenocarcinoma, making up 80% of cases. But, there are rarer types like clear-cell carcinoma and serous adenocarcinoma. These grow and spread faster than the common type.
It’s often found early because of symptoms like irregular bleeding. Finding it early can greatly improve treatment chances.
Knowing about endometrial cancer’s types and subtypes is key for good care. It’s a big health issue for women. We need more research and awareness to fight it.
Symptoms of Endometrial Cancer
Endometrial cancer is the most common type of uterine cancer. It often shows clear symptoms that tell women to see a doctor. The main sign is abnormal vaginal bleeding. This can be bleeding between periods or after menopause.
Women with endometrial cancer may also feel pelvic pain and have trouble or pain when urinating.
These symptoms happen when cancer cells grow and change the uterine lining. It’s important for women to watch for any unusual bleeding or pelvic pain. They should see a healthcare professional right away.
Early detection and diagnosis can greatly help treatment and improve life chances.
Also, endometrial cancer symptoms can include unexplained weight loss, fatigue, and feeling a mass or fullness in the pelvic area. Spotting these signs and getting medical help quickly can improve life quality for those with this disease.

“Prompt medical attention is crucial if any of these symptoms develop, as early detection can significantly improve treatment outcomes and prognosis.”
Risk Factors for Endometrial Cancer
Endometrial cancer has many risk factors. Knowing these can help find it early and manage it better.
Factors Contributing to Increased Risk
Obesity is a big risk factor. It makes endometrial cancer twice as common in overweight women and three times more common in obese women. Gaining weight and weight cycling also raise the risk after menopause.
Hormone imbalances, especially too much estrogen, increase risk. Estrogen therapy without progesterone can cause cancer. But, birth control pills can lower the risk, especially with long-term use.
Certain genetic disorders, like Lynch syndrome, raise the risk. This condition affects DNA repair genes, leading to a higher risk of colon and endometrial cancer.
Using the breast cancer drug tamoxifen also raises the risk, especially in postmenopausal women.
Other risk factors include early menstruation, late menopause, never being pregnant, and certain ovarian tumors.
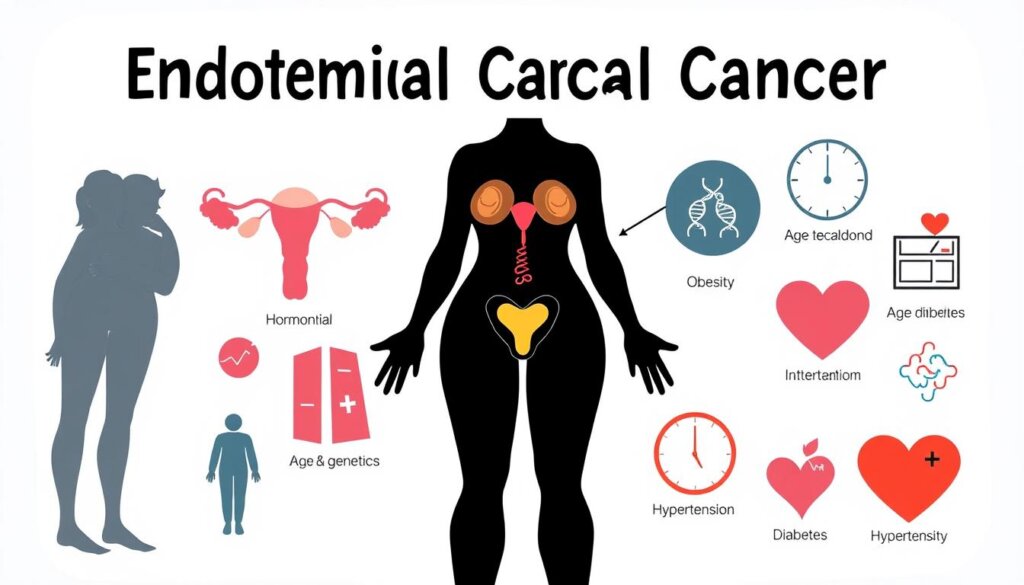
Understanding these risk factors helps take steps to lower them. Regular screenings and early detection are key to better outcomes in endometrial cancer.
Endometrial Cancer Diagnosis
Diagnosing endometrial cancer often includes pelvic exams, transvaginal ultrasounds, and endometrial biopsies. A pelvic exam lets your gynecologist check your vagina, cervix, and uterus for any issues. Transvaginal ultrasounds use sound waves to show detailed images of your uterus and ovaries.
An endometrial biopsy is key in finding cancer. It removes a small part of the uterine lining for lab tests. This helps find cancer cells. These biopsies are very accurate, especially in postmenopausal women.
Your doctor might also order more tests like chest X-rays or MRIs. Blood tests, like a CBC, can also help understand your health and the disease’s progress.
Endometrial cancer is graded from 1 to 3 based on cell similarity to normal tissue. This grading helps decide treatment and gives a hint about your prognosis. Tests for gene and protein changes can also guide treatment, including immunotherapy for advanced cases.
There’s no standard test for endometrial cancer, but regular check-ups are key. Reporting any unusual symptoms, like abnormal bleeding, is also important for early detection. Working with your healthcare team ensures a personalized approach to your care.

Endometrial cancer is often curable, with treatment usually starting with surgery. At Dana-Farber Brigham Cancer Center, a team of pathologists specializes in gynecologic cancers. They review thousands of cases a year, ensuring accurate diagnosis and tailored treatment plans.
“Endometrial cancer is rarely detected through a Pap test, which does not serve as a screening tool for this type of cancer. The diagnosis of endometrial cancer typically involves an endometrial biopsy, dilatation and curettage, and transvaginal ultrasound.”
Types and Stages of Endometrial Cancer
Endometrial cancers are divided into two main types. Type I endometrial cancers, like endometrioid adenocarcinoma, are common and less aggressive. They have a better chance of recovery. Type II endometrial cancers, including serous carcinoma and clear cell carcinoma, are rarer but more aggressive.
These cancers are also staged to show how far they have grown and spread. The staging goes from Stage I to Stage IV. Lower numbers mean less advanced disease, and higher numbers mean more spread. The FIGO and AJCC TNM systems are used to classify them based on tumor size, lymph node involvement, and distant metastasis.
- Stage I endometrial cancer is in the uterus. Stage IA is in the endometrium, and Stage IB is in the inner half of the myometrium.
- Stage II endometrial cancer has spread to the cervix’s connective tissue but not beyond the uterus.
- Stage III endometrial cancer has spread to the vagina, parametria, or pelvic and/or para-aortic lymph nodes.
- Stage IV endometrial cancer is the most advanced. It has spread to the bladder, rectum, or distant organs like the lungs or liver.
The pathologic stage from surgery and the clinical stage from pre-surgery tests are key. They help decide the best treatment for endometrial cancer.
Knowing the type and stage of endometrial cancer is vital for treatment. This info helps doctors choose the right treatment. It could be surgery, radiation, chemotherapy, or a mix.
Treatment Options for Endometrial Cancer
Endometrial cancer is the most common gynecologic cancer in the U.S. It makes up 7% of all cancers in women. Treatment often combines surgery, radiation, and drugs. Each treatment is chosen based on the patient’s needs and cancer stage.
Surgical Therapies
Surgery is usually the first step in treating endometrial cancer. This might include removing the uterus and ovaries. Doctors also check lymph nodes to see if the cancer has spread.
Radiation Therapy
Some patients may also get radiation therapy. This can be used alone or with other treatments. External beam radiation therapy and brachytherapy (internal radiation) are common methods.
Systemic Therapies
For more advanced cancer, doctors might use chemotherapy, hormone therapy, targeted therapy, or immunotherapy. These treatments help slow cancer growth and may be used together.
Treatment Modality | Description |
|---|---|
Hysterectomy | Removal of the uterus is a common surgical procedure for endometrial cancer. |
Radiation Therapy | External beam radiation therapy and brachytherapy (internal radiation) are used to target and destroy cancer cells. |
Chemotherapy | A combination of drugs used to slow the growth or spread of endometrial cancer. |
Hormone Therapy | Drugs that can reduce or block hormones that may promote endometrial cancer growth. |
Targeted Therapy | Drugs that target specific molecules related to endometrial cancer growth and spread. |
Immunotherapy | Treatments that stimulate the body’s immune system to fight endometrial cancer. |
The treatment plan for endometrial cancer depends on several factors. These include the cancer’s stage and grade, and the patient’s health and preferences. At places like MD Anderson, a team of experts works together to create a personalized treatment plan for each patient.
“The treatment approach for endometrial cancer is determined by factors such as the stage and grade of the cancer, as well as the patient’s overall health and preferences.”
Research and clinical trials are always improving endometrial cancer treatment. Teams at cancer centers offer the latest care options. This helps patients get the best treatment for their disease.
Prevention and Risk Reduction
Endometrial cancer is the most common type of uterine cancer. It can often be prevented or its risk reduced through lifestyle and medical interventions. Women who are overweight or obese are up to 3 times more likely to develop endometrial cancer compared to women at a healthy weight. Higher levels of physical activity have also been linked to lower risks of endometrial cancer.
Hormone therapy is a key aspect of endometrial cancer prevention. Progestins can reduce the risk of endometrial cancer in women taking estrogen therapy. However, this combination increases the risk of breast cancer. Another effective preventive measure is the use of birth control pills for at least one year. This can significantly lower the risk of endometrial cancer.
There are other steps you can take to reduce your risk of endometrial cancer. Studies have shown promising results for the use of aspirin in carriers of hereditary colorectal cancer. This may also reduce the risk of endometrial cancer. Prophylactic surgery, such as hysterectomy or salpingo-oophorectomy, may also be considered for individuals with a high genetic risk, such as those with Lynch syndrome.
A combination of lifestyle modifications, hormone therapy, and medical interventions can help lower the risk of endometrial cancer and improve overall health. Discuss your specific risk factors and prevention strategies with your healthcare provider. This will help determine the best approach for you.
Endometrial Cancer
Endometrial cancer starts in the lining of the uterus, called the endometrium. It’s the most common uterine cancer and affects women’s reproductive systems. About 95% of uterine cancers are endometrial, with 66,200 new cases in the U.S. each year. Most cases happen in people over 60, with an average age of 60 at diagnosis.
Things that raise your risk include estrogen therapy without progesterone, being obese, having diabetes, and starting menstruation early. Early detection is key, with 95% of women surviving 5 years if caught early. But, if it spreads, only 25% of women survive 5 years. Complications can include anemia, uterus perforation, and surgery issues.
Endometrial cancer is treatable, especially if caught early. There’s no screening test, but high-risk women need regular check-ups. Keeping a healthy weight and using birth control pills can lower your risk.
If you’re worried about endometrial cancer, talk to your doctor. Early detection and treatment can greatly improve your chances.
Endometrial Cancer Statistics | Data |
|---|---|
Most common type of uterine cancer | Endometrial cancer accounts for 95% of uterine cancers. |
Estimated new cases of uterine cancer per year in the U.S. | There are an estimated 66,200 new cases of all types of uterine cancer in the United States each year. |
Average age at diagnosis | The average age at diagnosis for endometrial cancer is 60. |
5-year survival rate if cancer has not spread | 95% of women are alive 5 years after treatment if the endometrial cancer has not spread. |
5-year survival rate if cancer has spread to distant organs | Around 25% of women are still alive after 5 years if endometrial cancer has spread to distant organs. |
“Endometrial cancer is generally highly treatable, especially when detected and treated early.”
Prognosis and Survival Rates
The outlook for endometrial cancer changes a lot based on its stage. Those with localized cancer (cancer only in the uterus) have a 95% chance of living five years. But, this number drops to about 70% for regional cancer (cancer in nearby areas or lymph nodes). And it’s just 18% for distant metastatic cancer (cancer in other organs).
In England from 2016 to 2020, endometrial cancer survival was good. About 90% of patients lived at least a year, 75% for five years, and over 70% for ten years. Early detection and treatment are key because the cancer’s stage at diagnosis greatly affects survival.
Endometrial Cancer Stage | 5-Year Relative Survival Rate |
|---|---|
Stage 0 | 90% |
Stage IA | 88% |
Stage IB | 75% |
Stage II | 69% |
Stage IIIA | 58% |
Stage IIIB | 50% |
Stage IIIC | 47% |
Stage IVA | 17% |
Stage IVB | 15% |
Endometrial cancer survival rates also depend on SEER stages. Localized (95%), regional (70%), and distant (18%) stages have a 5-year survival rate of 81% overall. These numbers come from the Surveillance, Epidemiology, and End Results (SEER) database. They help understand the prognosis for those with this cancer.
In summary, endometrial cancer survival greatly depends on its stage at diagnosis. Survival rates are high for early stages but drop as the cancer spreads. Knowing these survival rates helps patients and doctors make better care plans.
Conclusion
Endometrial cancer is the most common type of uterine cancer. It affects the lining of the uterus and is treatable if caught early. A study from 2023 reported that it impacts many people, as shown by cancer statistics data.
Symptoms like abnormal vaginal bleeding are key to early detection. This is crucial for effective treatment and better outcomes. Research from 2021 shed new light on endometrial cancer, following updated guidelines.
Risk factors include obesity, diabetes, and estrogen-replacement therapy. Those with complex atypical hyperplasia face higher risks after diagnosis. Treatment may include surgery, radiation, and hormone or chemotherapy therapy. Survivors face lifestyle challenges.
Endometrial cancer is treatable, especially if caught early. Women should know the risk factors and talk to their doctors. It’s the 13th most common cancer in women, often found in those over 50.
Early detection and treatment can greatly improve survival rates. This is true for those with uterine cancer.
FAQ
What is endometrial cancer?
Endometrial cancer starts in the lining of the uterus. It’s the most common uterine cancer.
What are the symptoms of endometrial cancer?
Symptoms include abnormal vaginal bleeding and pelvic pain. You might also feel pain when you pee.
What are the risk factors for endometrial cancer?
Being overweight and having too much estrogen are risks. So is starting menstruation early or late menopause. Never being pregnant and older age also increases risk. Some genetic disorders, like Lynch syndrome, and taking tamoxifen for breast cancer also raise risk.
How is endometrial cancer diagnosed?
Doctors use pelvic exams, ultrasounds, and biopsies to diagnose it.
What are the different types and stages of endometrial cancer?
There are two main types: Type I is common and less aggressive, while Type II is rare but aggressive. Stages are based on tumor size and spread.
What are the treatment options for endometrial cancer?
Surgery is the main treatment, often including a hysterectomy. Radiation, chemotherapy, and hormone therapy may also be used.
How can I reduce my risk of endometrial cancer?
Talk to your doctor about hormone therapy risks. Using birth control pills for a year and staying healthy can help.
What is the prognosis and survival rate for endometrial cancer?
Survival rates vary by stage. Localized cancer has a 96% five-year survival rate. This drops to 72% for regional and 20% for distant metastasis.