FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Regular eye exams play a crucial role in detecting serious eye conditions, like glaucoma, a leading cause of blindness.
These exams go beyond ensuring optimal vision; they can catch underlying issues in their earliest, most treatable stages. SouthCoast Health emphasizes the importance of such screenings, especially for adults over 40.
Often, there’s confusion about which eye care professional can diagnose glaucoma. The answer is: Optometrists.
Equipped with the right tests, optometrists can assess your optic nerve and vision, diagnosing glaucoma during a detailed eye exam.
This article focuses on the crucial role of optometrists in detecting and managing glaucoma, aiming to dispel misunderstandings and emphasize the importance of regular eye check-ups.
Understanding Glaucoma
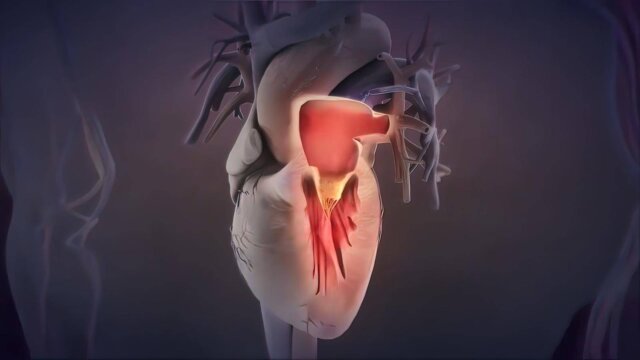
Glaucoma is a collection of eye conditions that damage the optic nerve, an essential component for good vision.
The optic nerve carries visual information from the eye to the brain and its damage often links to high eye pressure (Mayo Clinic). This damage results in gradual vision loss.
Glaucoma can strike at any age, but it is more prevalent in older adults and is a leading cause of blindness for those over 60 (American Academy of Ophthalmology).
Certain risk factors increase the likelihood of developing glaucoma, such as being over 40, having a family history of the condition, and long-term use of steroid medications.
Early detection and treatment are crucial as the condition’s effect is so gradual that you may not notice a change in vision until the later stages.
Regular eye exams can help detect glaucoma in its early stages before significant damage occurs. If recognized early, vision loss can be slowed or even prevented (Mayo Clinic).
Qualifications and Training of Optometrists

Optometrists are healthcare professionals trained to diagnose and manage eye diseases, but they differ significantly from ophthalmologists in terms of education and training.
They receive an “O.D.” degree after four years in optometry school, which does not necessitate postgraduate training like a medical doctor’s degree (source).
Despite not being medical doctors, optometrists acquire a wealth of knowledge and skills in detecting and managing eye diseases. They are capable of prescribing medications and performing certain procedures, albeit restricted by the terms of the optometry license in their respective states (source).
However, the push for full patient-care parity with ophthalmologists has been met with resistance. Critics argue that to achieve parity, optometrists must undergo equivalent training, supervised experience, and evaluation as ophthalmologists, thereby ensuring patient safety and quality of care (source).
Techniques and Tools Used for Glaucoma Diagnosis

When it comes to diagnosing glaucoma, several reliable techniques and tools are employed by optometrists. The commonly used methods are eye pressure measurement, visual field testing, and imaging techniques.
- Eye Pressure Measurement: Often regarded as the first line of defense in glaucoma diagnosis, this process involves checking the intraocular pressure (IOP). High eye pressure may indicate a higher risk of glaucoma.
- Visual Field Testing: This test is used to evaluate the peripheral or ‘side’ vision of a patient, typically affected in glaucoma patients before central vision.
- Imaging: Tools like optical coherence tomography (OCT) help in obtaining detailed images of the eye’s interior, allowing for the assessment of the optic nerve, retina, and corneal thickness.
These diagnostic tools are vital for a comprehensive eye exam, ensuring the accurate detection and timely diagnosis of glaucoma.
Role of Optometrists in Managing and Treating Glaucoma
Optometrists play a pivotal role in the detection and management of glaucoma, often working in collaboration with ophthalmologists to ensure comprehensive care. Their expertise in managing glaucoma-related health issues is invaluable, as they are often the first line of defense in patient healthcare.
One of the key areas of management involves medication, with optometrists well-versed in the latest treatments and their applications.
Dr. Jackie Burress, an experienced practitioner, emphasizes that optometry education provides the necessary training to manage this multifaceted disease, with continuous learning resources readily available for updating knowledge on new tools and medications (source).
In addition to medication, optometrists can also administer laser treatments, such as Selective Laser Trabeculoplasty (SLT), which is becoming more common in practice.
However, it’s important to note that SLT isn’t the best choice for every glaucoma patient and careful patient selection is crucial (source).
Despite significant gains in scope expansion, there’s still a need for more optometrist involvement in glaucoma care. The number of patients with glaucoma is projected to increase significantly by 2050, underscoring the crucial role of optometrists in managing this disease (source).
Limitations and Challenges for Optometrists
In the landscape of glaucoma care, optometrists are increasingly stepping in to fill the gap left by the dwindling number of ophthalmologists in the United States.
However, their role is not without limitations and challenges. The main issue they face is the time-consuming and bureaucratic nature of glaucoma treatment, which makes it a laborious task for many.
Review of Optometry found that 8.3% of optometrists don’t treat glaucoma because their practice requires them to refer out.
Timely Referral
There is an importance of timely referral to ophthalmologists for more complex cases. However, some optometrists may feel they’ve plateaued in their ability to manage glaucoma, leading to a reluctance to refer out. This could be due to a gap between their training and current practice.
Challenges and Controversies
Despite the high level of agreement between optometrists and ophthalmologists on glaucoma diagnosis and treatment, there are still disagreements, mostly on the lower end of the severity scale. These disagreements could lead to unnecessary reviews and increased costs, as found by a study.
In conclusion, while optometrists play a crucial role in glaucoma care, there are limitations and challenges that need to be addressed. More training, better guidelines, and increased public awareness could help overcome these issues.
Conclusion
In the battlefield against glaucoma, optometrists serve as the early warning system. They play a critical role in early detection and management of this condition, often being the first to identify signs of increased intraocular pressure – a key indicator of glaucoma.
Regular eye exams are, therefore, not just a routine procedure but a crucial strategy for preserving vision.
Optometrists are also instrumental in monitoring patients, from those with a high risk of developing glaucoma to those already diagnosed with mild and moderate cases. This close surveillance helps in reducing the risk of vision loss over a lifetime, making the optometrist-patient relationship an essential part of glaucoma management.
Finally, remember that your optometrist is a valuable resource. Consult with them if you have any concerns about glaucoma or other eye diseases. Early detection and treatment can make a world of difference.