FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Basal cell carcinoma is the most common skin cancer, hitting nearly 3 million people in the U.S. each year. It’s a treatable form of non-melanoma skin cancer. It usually shows up as a clear or pearly bump on the skin, often in places that get a lot of sun like the head and neck.
Knowing the symptoms, causes, and how to prevent basal cell carcinoma is key. It helps catch it early and treat it well.
Key Takeaways
- Basal cell carcinoma is the most prevalent type of skin cancer, accounting for the majority of cases.
- It commonly manifests as a bump or growth on sun-exposed areas of the skin, often the head and neck.
- Chronic sun exposure and fair skin are major risk factors for developing basal cell carcinoma.
- Early detection and prompt treatment, often through Mohs surgery, are critical for successful outcomes.
- Protecting your skin from UV radiation, performing self-exams, and regular skin checks with a dermatologist can help prevent basal cell carcinoma.
By understanding basal cell carcinoma, you can protect your skin. This helps lower your risk of this common, but treatable, skin cancer.
What is Basal Cell Carcinoma?
Overview and Definition
Basal cell carcinoma (BCC) is the most common skin cancer, making up 80% of all skin cancers. It starts in the basal cells of the epidermis, the skin’s outer layer. These cells produce new skin cells as old ones die. BCC looks like a clear bump on the skin and is caused by UV radiation from the sun or tanning beds.
It often shows up on sun-exposed areas like the face, head, neck, and arms.
In the U.S., BCC is the most common skin cancer, with 3.6 million cases each year. BCCs rarely spread and are less likely to spread than SCC. But, if not treated, BCC can grow and invade deeper into the skin.

BCC is treatable if caught early. Knowing its signs is key for early detection and treatment.
Signs and Symptoms of Basal Cell Carcinoma
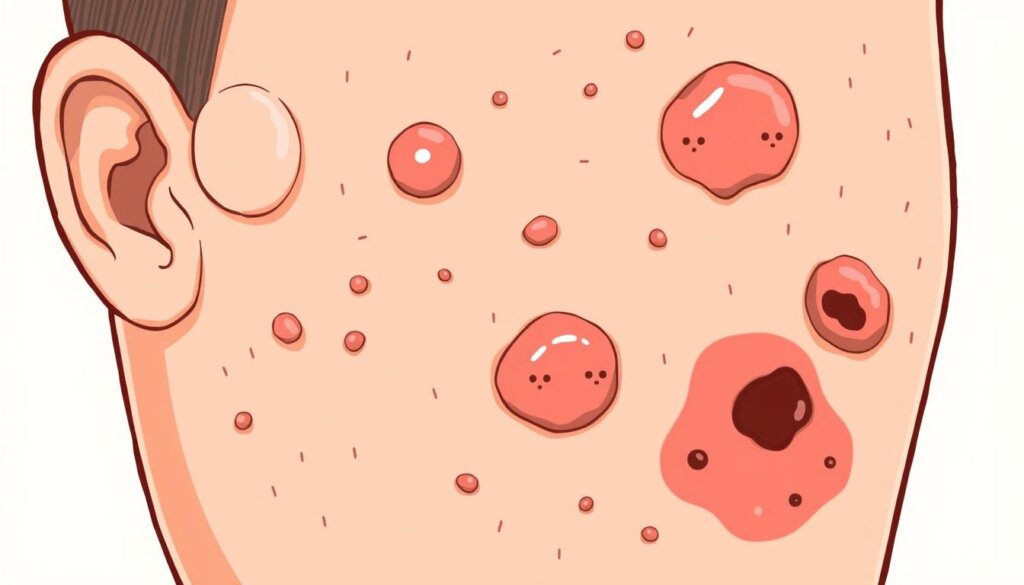
Basal cell carcinoma is the most common skin cancer. It shows up as a shiny, skin-colored bump on sun-exposed areas. These can be on the face, ears, neck, scalp, chest, shoulders, and back.
Lesions can look different. They might be translucent or pearly white, or brown, black, or blue. They can also have a raised, translucent border.
Some lesions look like a flat, scaly patch or a white, waxy, scar-like spot. They don’t have a clear border.
One sign of basal cell carcinoma is that the lesions can bleed and scab over. It’s important to watch for any skin changes. Report them to a dermatologist early for the best treatment.
Most basal cell carcinomas can be removed without problems if caught early.
Basal cell carcinomas can appear anywhere on the body. But they often show up on sun-exposed areas. Two or more warning signs are often present in a BCC tumor.
BCCs on the nose, ears, and lips are more likely to come back. So, it’s important to stay vigilant and get regular check-ups.
If you see new, changing, or unusual skin growths, see a dermatologist. Early detection and treatment are key to managing basal cell carcinoma.
Remember, daily sun protection helps prevent skin cancer. It’s also good to have an annual skin exam by a dermatologist if you’ve had BCC, SCC, or precancerous lesions.
Causes and Risk Factors
Ultraviolet Light Exposure and Other Causes
Basal cell carcinoma often comes from UV light from the sun or tanning beds. This light can harm DNA in basal cells, making them grow too fast. More than 90% of nonmelanoma skin cancers, like basal cell carcinomas, are caused by UV light.
Also, over 419,000 skin cancer cases in the U.S. each year are linked to indoor tanning. About 245,000 of these are basal cell carcinomas.
Sun exposure is the main reason, but basal cell carcinomas can also happen on hidden skin. This shows other factors might play a part in some cases. Other risk factors include radiation therapy, fair skin, and getting older. Also, a family history of skin cancer, using immune-suppressing drugs, and arsenic exposure can increase risk.
People who have tanned indoors have a 29% higher risk of basal cell carcinoma. Any indoor tanning history before 40 raises the risk by 69%. Men are more likely to get basal cell carcinoma than women. The number of new cases has gone up, especially in young adults, due to more UV exposure and indoor tanning.
Those with lighter skin are at higher risk of basal cell carcinoma. People with light skin, blond or red hair, and blue, green, or grey eyes face the highest risk. This is especially true if they have sun exposure or indoor tanning history. Those who have had basal cell carcinomas are at risk of getting more over time.
“Exposure to ultraviolet (UV) rays is a major risk factor for most skin cancers, with sunlight being the main source of UV rays.”
Basal Cell Carcinoma: Symptoms, Treatment & Prevention
Basal cell carcinoma is the most common skin cancer. It shows up as a clear bump on sun-exposed skin, like the head and neck. Long-term sun or tanning bed use causes it.
Surgery is the main treatment for basal cell carcinoma. Removing the growth can cure it for small, early cancers. Mohs surgery is another method, curing up to 99% of first-time tumors. Other options include cryosurgery, radiation, and creams like 5-FU and Imiquimod.
To avoid basal cell carcinoma, stay out of the sun, use sunscreen, and wear protective clothes. Regular skin checks can catch problems early, making treatment more likely to work.
Treatment Approach | Cure Rate |
|---|---|
Curettage and Electrodesiccation | Close to 95% for small BCCs |
Mohs Surgery | Up to 99% for tumors treated for the first time |
Excisional Surgery | Above 95% for small, early BCCs |
Radiation Therapy | 90% |
Cryosurgery | 85-90% for smaller, superficial BCCs |
Topical Medications (5-FU, Imiquimod) | 80-90% for superficial BCCs |
For advanced basal cell carcinoma, drugs like Vismodegib and Sonidegib, or Cemiplimab, might be used.

Regular skin checks and quick treatment are key to managing basal cell carcinoma. Knowing the symptoms, treatments, and prevention helps protect your skin from this common cancer.
Diagnosis and Testing
Medical History, Skin Exam, and Biopsy
Doctors start by asking about your medical history. They want to know about any skin changes or symptoms. Then, they do a full-body skin check for any odd growths.
If they find something odd, they’ll take a skin sample. This sample goes to a lab for tests. This step is key to confirming the cancer type.
Basal cell carcinoma is the most common skin cancer in the U.S. It’s caused by sun damage, mainly from UV rays. Catching it early is vital, as it can spread and harm tissue and bone if not treated.
“People with certain risks, like organ transplant patients, are very likely to get skin cancer.”
Your doctor might also do more tests. This includes lymph node biopsies or scans if the cancer has spread. These tests help figure out how far the cancer has gone. This is important for planning treatment.
Treatment Options
When treating basal cell carcinoma, the main goal is to remove the cancer completely. There are surgical and non-surgical ways to do this. The best plan depends on the patient’s needs.
Surgical Treatments
Surgical methods include excision and Mohs surgery. Excision removes the cancer and some healthy tissue. Mohs surgery removes layers until no cancer is left. Mohs surgery works best for high-risk cancers, with a cure rate over 99%.
After removing the cancer, skin grafts or flaps might be needed. These help the skin heal and look normal again.
Non-Surgical Treatments
For those not good for surgery or small, low-risk cancers, non-surgical options exist. Radiation therapy is good for hard-to-reach areas or high-risk patients. Cryosurgery (freezing) and creams or lotions are also options.
After treatment, follow-up care is key. Basal cell carcinomas can come back. People treated are at higher risk for new skin cancers. Protecting your skin from the sun is also important to prevent recurrence.
“The success of treatment depends on various factors including the location, size, depth of the tumor, general health, medical history, and prior treatment of the tumor.”
Prevention Strategies
Keeping your skin safe from harmful UV rays is key to avoiding basal cell carcinoma. UV rays are a big risk for this skin cancer. To stay safe, avoid too much sun, especially when it’s strongest in the middle of the day.
Wear clothes that protect your skin from the sun. Use sunscreen with SPF 30 or higher. And don’t use tanning beds to avoid skin damage.
Doing regular skin checks is also important. This helps spot new growths or changes in moles and freckles early. Catching skin cancer early is crucial for treatment success. Being careful and quick to notice skin changes helps prevent this cancer.
Prevention Strategies | Benefits |
|---|---|
Avoid excessive sun exposure | Reduces UV radiation exposure, a primary risk factor for basal cell carcinoma |
Use broad-spectrum sunscreen (SPF 30+) | Helps protect against both UVA and UVB rays, which can cause skin damage and cancer |
Wear sun-protective clothing | Covers and shields the skin from harmful UV rays |
Avoid tanning beds | Tanning beds emit harmful UV rays that contribute to long-term skin damage and cancer risk |
Perform regular skin self-exams | Enables early detection of new growths or changes in existing moles, freckles, or lesions |
By using these prevention tips, you can significantly reduce your risk of developing basal cell carcinoma. This helps keep your skin healthy for a long time.
“Protecting your skin from the sun’s harmful UV rays is one of the most effective ways to prevent basal cell carcinoma.”
Complications and Outlook
Basal cell carcinoma (BCC) is the most common skin cancer in the US, hitting nearly one in five people. It’s treatable, but knowing the risks and needing ongoing checks is key.
BCC can come back, even after treatment. Up to 10% of cases can return within five years. So, regular skin checks are vital to catch any new or coming back growths early.
People who’ve had BCC are at higher risk for other skin cancers, like squamous cell carcinoma. It’s important to keep an eye on your skin and protect it from the sun to avoid more cancers.
In rare cases, BCC can spread to lymph nodes or other areas, known as metastatic BCC. This serious form needs strong treatments, like surgery or special medicines.
But, if caught early, BCC’s outlook is good, with low risks of serious problems or death. Treatments like surgery, freezing, or Mohs surgery have cure rates over 95%.
Keeping an eye on your skin and protecting it from the sun are crucial for managing BCC risks. Early detection and the right treatment mean most people with BCC can do well in the long run.
“Basal cell carcinoma is the most common type of skin cancer, but it is also one of the most treatable when caught early. Regular skin checks and sun protection are essential to managing this condition and reducing the risk of recurrence or other complications.”
Conclusion
Basal cell carcinoma is the most common skin cancer. It’s caused by UV radiation from the sun or tanning beds. It often shows up as a growth on sun-exposed skin. Early detection and treatment are key, as it can spread if not treated.
Protecting your skin from UV damage is important. Regular sun protection and self-exams can lower your risk. Also, seeing a doctor for any skin changes can lead to early treatment and a better outcome.
Knowing about basal cell carcinoma’s symptoms and prevention is vital for your skin health. By taking care of your skin and being careful, you can manage your skin cancer risk. This way, you can have a healthier and more confident future.
FAQ
What is basal cell carcinoma?
Basal cell carcinoma is a common skin cancer. It starts in the basal cells of the skin’s outer layer. These cells make new skin as old ones die.
It often looks like a clear bump on the skin.
What are the common signs and symptoms of basal cell carcinoma?
It usually shows up on sun-exposed areas, like the head and neck. Signs include a shiny, clear bump or a brown, black, or blue spot.
It can also look like a flat, scaly patch or a white, waxy scar. These spots may bleed and scab.
What causes basal cell carcinoma?
Long-term sun exposure or tanning bed use damages skin cells. This leads to rapid cell growth. Other risks include fair skin, age, and family history of skin cancer.
Immune-suppressing drugs and arsenic exposure also increase risk.
How is basal cell carcinoma diagnosed?
Doctors start with a medical history and skin exam. They look for any changes or growth.
If they find something suspicious, they might take a skin biopsy. This involves removing a small tissue sample for lab testing.
What are the treatment options for basal cell carcinoma?
Treatment aims to remove the cancer completely. Common methods include surgical excision and Mohs surgery.
These remove the cancer and healthy tissue around it. In some cases, radiation, freezing, or topical treatments are used.
How can I prevent basal cell carcinoma?
Avoid too much sun, especially during the day. Wear protective clothing and use sunscreen with at least SPF 30.
Stay away from tanning beds. Regular self-exams help catch any new growths or changes.