FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Arthritis isn’t just a singular narrative of joint pain; it’s an umbrella term encompassing various conditions that can affect not only bones but also the symphony of tissues and organs in concert with them.
Understanding the nuanced differences between its types, such as rheumatoid arthritis (RA) and osteoarthritis (OA), is crucial for effective management and treatment.
This article aims to shine a light on the dichotomy between RA, an autoimmune assault on the joints, and OA, a tale of wear and tear on cartilage.
We will navigate through the labyrinth of symptoms and treatments, distinguishing the inflammatory onslaught of RA from the gradual erosion characteristic of OA.
Acknowledging these differences equips us with the knowledge to tailor our approach to arthritis care, ensuring a narrative where quality of life remains the protagonist.
Understanding Rheumatoid Arthritis and Osteoarthritis
Rheumatoid Arthritis (RA) and Osteoarthritis (OA) are two distinct forms of arthritis that affect millions globally.
RA is an autoimmune condition where the body’s immune system erroneously targets joint linings, leading to inflammation and joint damage.
This can occur at any age and tends to develop rapidly, often symmetrically affecting both sides of the body.
In contrast, OA is the wear-and-tear deterioration of joint cartilage due to mechanical stress, typically emerging later in life and progressing gradually.
While both conditions share symptoms like joint pain and reduced function, RA also presents with systemic symptoms such as fever, fatigue, and loss of appetite.
OA symptoms are usually localized to the affected joints without systemic manifestations.
In terms of prevalence, OA is more common, affecting around ten times more individuals than RA.
Understanding these differences is crucial for diagnosis and tailoring effective treatment strategies.
Risk Factors for Rheumatoid Arthritis and Osteoarthritis
Both Rheumatoid Arthritis (RA) and Osteoarthritis (OA) share common risk factors such as advanced age and gender, with OA being more frequent in individuals over 65 and RA slightly more prevalent in women after the age of 45.
Lifestyle choices also play a significant role; for instance, smoking has been linked to increased RA risk, while excess weight can exacerbate both conditions by promoting inflammatory processes detrimental to joint health.
However, the risk factors for RA and OA can diverge, reflecting their distinct pathologies. RA, an autoimmune condition, may be influenced by factors like gum disease and changes in the microbiome, while OA is often related to mechanical wear and tear.
Thus, a history of joint injury may specifically elevate OA risk, emphasizing the mechanical aspect of its development.
Diagnosis and Treatment
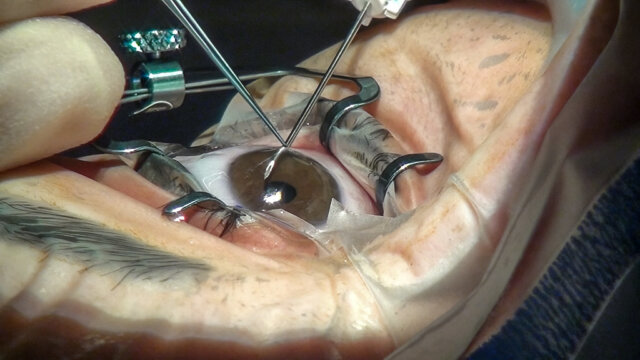
Diagnosing Rheumatoid Arthritis (RA) begins with a medical history review and a physical exam, supplemented by blood tests and imaging, such as X-rays, to detect joint damage and inflammation.
Imaging might include ultrasound or MRI, which are more sensitive in the early stages of RA.
In contrast, Osteoarthritis (OA) diagnosis focuses on medical history, physical examination, and imaging studies like X-rays, which may show joint space narrowing and bone spurs, characteristic of OA.
Treatment for RA often involves immunosuppressive therapies like methotrexate and biologics to control systemic inflammation.
OA management typically includes pain relief through nonsteroidal anti-inflammatory drugs and may progress to surgical intervention.
Both conditions benefit from lifestyle modifications, including exercise, weight loss, and stress management, which help maintain joint function and reduce symptoms.
The effectiveness of treatments varies; for RA, achieving remission is possible, while OA treatments aim to slow progression and alleviate discomfort. Accurate diagnosis is crucial as it guides these tailored treatment strategies, optimizing patient outcomes.
Impact on Daily Life
Arthritis is not just a medical diagnosis; it’s a daily challenge that weighs heavily on the lives of those affected.
When we talk about Rheumatoid Arthritis (RA) and Osteoarthritis (OA), we’re addressing two culprits that can turn simple tasks into daunting hurdles.
RA, with its characteristic morning stiffness and inflammation affecting multiple joints, can make a morning routine feel like running a marathon.
On the flip side, OA often brings a deep, aching pain to the weight-bearing joints like the knees and hips, turning a quick grocery run into a test of willpower.
The ripple effect of these conditions can be far-reaching, influencing one’s ability to work, engage in social activities, and maintain independence.
Tasks that once seemed effortless, such as opening jars, climbing stairs, or even walking, can become marathons of discomfort. Furthermore, both conditions can lead to severe joint pain and joint damage, escalating the risk of disability.
While the physical toll is evident, the emotional and psychological impacts are equally significant. The persistent discomfort and functional limitations can contribute to feelings of frustration and depression, creating a feedback loop that exacerbates the impact on daily life.
Therefore, recognizing the signs early and seeking timely medical care is crucial in preserving the quality of life and well-being.
Complementary Treatments
When it comes to managing the symptoms of rheumatoid arthritis (RA) and osteoarthritis, complementary treatments such as physical therapy and supplements can play a supportive role alongside conventional medicine.
Physical therapy, for instance, has been recognized for its ability to improve joint function and reduce pain.
Supplements like turmeric, ginger, and valerian root are touted for their anti-inflammatory properties, though the research is still evolving.
Evidence from clinical trials suggests that some natural supplements may reduce symptoms like swelling and morning stiffness in RA.
However, the efficacy of these treatments can vary, and not all have been backed by rigorous scientific research.
For instance, systematic reviews have shown that interventions like acupuncture and capsaicin cream have a favorable risk-benefit profile, while the evidence for others, such as homeopathy, remains weak or contradictory.
It’s crucial that patients consult with a healthcare professional before trying any complementary treatments to ensure they are appropriate and safe, taking into account individual health conditions and potential interactions with current medications.
A collaborative approach to care is key in managing these complex conditions.
Management and Self-Care
Managing rheumatoid arthritis and osteoarthritis extends beyond clinical treatments; it requires a daily commitment to self-care. Key lifestyle adjustments can significantly ease discomfort and improve joint function.
Exercise is crucial; low-impact activities such as swimming or yoga maintain joint flexibility without exacerbating pain. A balanced diet rich in anti-inflammatory foods can also help manage disease activity.
- Weight management is essential, as excess weight puts additional stress on individual joints, especially the knees and hips.
- Ensuring sufficient rest is another pillar of self-care, allowing the body to recover and reduce symptoms.
- Pain can be alleviated through both heat and cold treatments, which help to soothe stiff joints and reduce swelling, respectively.
Remember, everybody is unique. It is important to work in tandem with health care providers, like those at the Mayo Clinic, to tailor a self-care plan that optimizes your quality of life.
Whether it’s modifying activities to reduce joint strain or exploring different drug treatments and nonsteroidal anti-inflammatory drugs (NSAIDs), each step taken is a stride toward managing arthritis more effectively.
When in doubt, consulting with your doctor is the safest course of action to ensure that self-care measures complement prescribed treatments.
Conclusion
Understanding the distinctions between Rheumatoid Arthritis (RA) and Osteoarthritis (OA) is key to managing these pervasive joint conditions.
RA, an autoimmune disorder, targets the body’s joints symmetrically, often leading to systemic inflammation and even flu-like symptoms.
Contrastingly, OA, which is not autoimmune, stems from the deterioration of cartilage due to wear and tear, typically affecting joints asymmetrically and without the systemic effects seen in RA.
Both conditions can lead to significant joint pain and stiffness, but their underlying causes and treatment approaches vary considerably. Acknowledging these differences is crucial for effective management and improved quality of life.