FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Pericardial diseases are a big health issue, with up to 5% of hospital visits for chest pain due to acute pericarditis. These diseases affect the sac around the heart but are often missed. This can lead to serious problems if not treated. This article will cover the different types of pericardial diseases, their causes, symptoms, how they are diagnosed, and the latest treatments.
Key Takeaways
- Pericardial diseases are many conditions that affect the pericardium, the sac around the heart.
- Common types include Acute pericarditis, Chronic pericarditis, Pericardial effusion, and Constrictive pericarditis.
- Causes can be viral infections, autoimmune disorders, cancer, trauma, or unknown reasons.
- Symptoms like chest pain, shortness of breath, fatigue, and fever need quick medical help.
- Doctors use electrocardiograms, echocardiograms, cardiac imaging, and sometimes fluid analysis to diagnose.
Introduction to Pericardial Diseases
The pericardium is a thin, protective sac that surrounds the heart. It keeps the heart in place and protects it from infection and inflammation. Pericardial diseases include inflammation, fluid buildup, and scarring. These can affect the heart’s function if not treated.
There are many types of pericardial diseases, each with its own effects. One type is pericarditis, which causes inflammation of the pericardium. It can be acute, subacute, or chronic. Another type is pericardial effusion, where fluid builds up in the pericardial sac. This can lead to a serious condition called cardiac tamponade. Constrictive pericarditis is rare but serious. It makes the pericardium thick and scarred and affects the heart’s function.
Pericardial diseases can greatly affect a person’s health, leading to a lot of suffering and death. Knowing the different types, causes, symptoms, and treatments is important.
“Pericardial diseases can have a significant impact on an individual’s health, contributing to substantial morbidity and mortality.”
Pericardial Disease | Description | Prevalence |
|---|---|---|
Acute Pericarditis | Inflammation of the pericardium, often due to viral infections or autoimmune disorders. | Common, with a recurrence rate of up to 50% in patients treated with steroids. |
Chronic Pericarditis | Persistent inflammation of the pericardium, lasting more than 3 months. | It is uncommon, but it can lead to significant morbidity if left untreated. |
Pericardial Effusion | Accumulation of fluid within the pericardial sac, potentially leading to cardiac tamponade. | Common, with a wide range of underlying causes, including infections, autoimmune disorders, and cancer. |
Constrictive Pericarditis | Thickening and scarring of the Pericardium impair the heart’s ability to function properly. | Rare, but requires prompt diagnosis and treatment to prevent further complications. |
Types of Pericardial Diseases
Pericardial diseases affect the sac around the heart. They include acute pericarditis, chronic pericarditis, Pericardial effusion, and constrictive pericarditis.
Acute Pericarditis
Acute pericarditis is when the pericardium gets inflamed. It causes chest pain, a pericardial friction rub, and changes on an electrocardiogram (ECG). This condition usually gets better on its own. It often starts 3–14 days after a heart attack or surgery. Most of the time, it’s caused by a virus.
Chronic Pericarditis
Chronic pericarditis means the inflammation doesn’t stop. It can make scar tissue over time. Sometimes, it comes back and is called Dressler’s syndrome or postcardiotomy syndrome.
Pericardial Effusion
Pericardial effusion is when fluid builds up around the heart. This can make the heart work less well. Sometimes, this fluid can be removed, and it helps a lot. Trauma, a certain type of aorta problem, or heart rupture can cause bleeding into this space.
Constrictive Pericarditis
Constrictive pericarditis makes the pericardium scar and thicken. This makes it hard for the heart to fill up and work right. It often happens after tuberculosis or bleeding into the pericardium. It’s hard to tell apart from another heart condition.
Type of Pericardial Disease | Description |
|---|---|
Acute Pericarditis | Inflammatory process involving the pericardium, resulting in chest pain, pericardial friction rub, and ECG changes. Viral pericarditis is the most common type. |
Chronic Pericarditis | Persistent or recurrent inflammation of the pericardium leads to scar tissue formation. Relapsing episodes are referred to as Dressler’s syndrome or postcardiotomy syndrome. |
Pericardial Effusion | Fluid accumulation between the two layers of the pericardium can compress the heart and impair its function. Trauma, aortic dissection, and cardiac rupture can cause hemopericardium. |
Constrictive Pericarditis | Scarring and thickening of the pericardium lead to impaired ventricular filling and reduced cardiac output. It can most commonly follow tuberculous pericarditis or hemopericardium. |
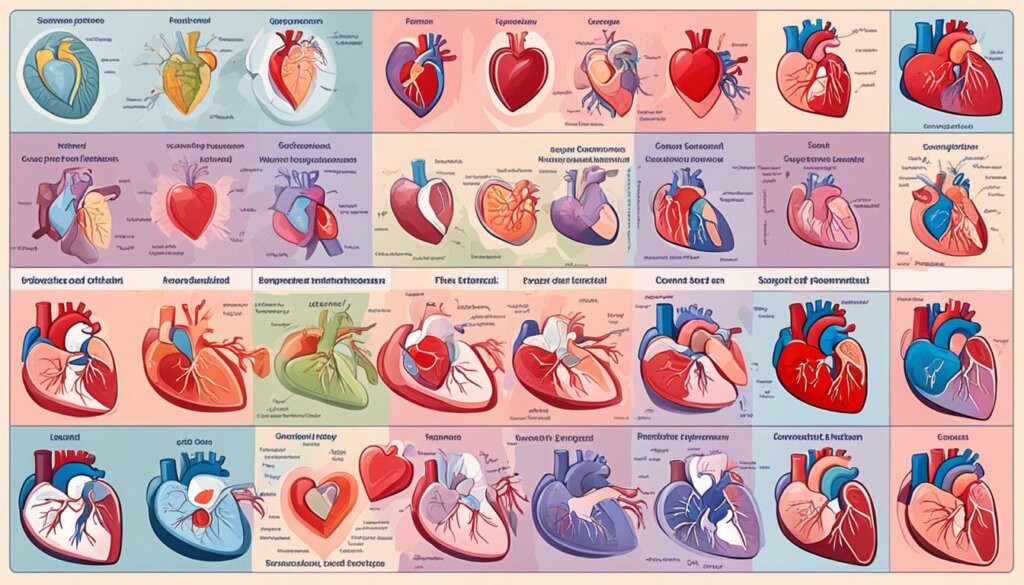
There are many pericardial diseases, like acute and chronic pericarditis, pericardial effusion, and constrictive pericarditis. Each one affects the heart in different ways. If not treated, they can really harm the heart’s function.
Causes of Pericardial Diseases
Pericardial diseases can result from viral or bacterial infections, autoimmune disorders, or cancer. Knowing the causes helps with diagnosis and treatment.
Viral Infections
Viral infections are a top cause of pericarditis. Coxsackievirus B and echovirus are the main viruses causing it.
Bacterial Infections
Bacterial infections can lead to serious pericarditis. This is more common in people with weak immune systems or those with pneumonia.
Autoimmune Disorders
Autoimmune diseases like rheumatoid arthritis and lupus can cause pericarditis. This is called autoimmune pericarditis.
Cancer
Cancer can also cause pericardial diseases. This happens when cancer spreads to the pericardium from other parts of the body. Common cancers include lung, breast, and lymphoma.
Doctors must know the causes of pericardial diseases. This helps them treat patients correctly. Whether the disease is caused by a virus, bacteria, autoimmune issues, or cancer, the right treatment is key to good results.
“Pericardial diseases can have far-reaching consequences if not properly diagnosed and managed. Recognizing the underlying causes is the first step in providing the best possible care for patients.” – Dr. Sarah Linden, Cardiologist
Symptoms of Pericardial Diseases
Pericardial diseases show many symptoms that help doctors figure out what’s wrong. These signs include:
- Acute, severe, and sharp chest pain that may spread to the neck, shoulders, or back.
- A pericardial friction rub is a scratchy or grating sound heard during auscultation.
- Electrocardiogram (ECG) changes, like diffuse ST-segment elevation.
- Pericardial effusion can squeeze the heart and cause shortness of breath and low blood pressure.
The symptoms a patient has can tell doctors a lot about the disease. For instance, sudden, severe chest pain is often seen in acute pericarditis. On the other hand, chronic pericarditis comes on slowly with ongoing symptoms. Also, hearing a pericardial friction rub or seeing ECG changes can help tell it apart from other heart issues.
Patients should be aware of these pericardial disease symptoms and seek help immediately if they notice them. Quick action is key to avoiding serious problems and getting better.
Diagnosis of Pericardial Diseases
Diagnosing pericardial diseases takes a detailed look at the patient’s history, physical check-ups, and tests. These tests help find the cause and guide treatment.
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a simple test that shows the heart’s electrical signals. It can spot signs like ST-segment elevation, helping diagnose acute pericarditis.
Echocardiogram
An echocardiogram is key to determining whether there is fluid around the heart and how well it works. It shows the heart’s pumping power and checks for fluid buildup.
Cardiac CT Scan
Cardiac CT scans use X-rays to see the heart and chest. They help spot thickening that might mean constrictive pericarditis.
Cardiac MRI
Cardiac MRI uses magnetic fields and radio waves for detailed heart images. It’s great for finding tissue changes or inflammation around the heart.
Sometimes, tests like fluid analysis or biopsy are needed to find the cause of pericardial disease.
“The clinical diagnosis of pericarditis is confirmed when at least two of four clinical criteria are present: typical chest pain, pericardial friction rub, widespread ST-segment elevation, and pericardial effusion.”
Getting the diagnosis right is key to treating pericardial diseases. Clinical checks and tests allow doctors to fully understand the patient’s issue and offer tailored care.
Treatment of Pericardial Diseases
Pericardial diseases need different treatments based on their cause and severity. The main goals are to ease symptoms, control swelling, and prevent further problems.
Medications
Anti-inflammatory drugs are often the first choice for treating pericardial diseases. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen help lessen swelling and ease pain. Colchicine, an anti-inflammatory drug, can lower the chance of returning pericarditis. Corticosteroids, such as prednisone, might be given for severe cases or when other treatments don’t work.
Surgical Interventions
For big pericardial effusion or constrictive pericarditis, surgery might be needed. Pericardiocentesis is a procedure that uses a needle to drain fluid from the pericardial space. This is often done with the help of imaging like echocardiography. If fluid keeps coming back or the pericardium gets thick and stiff, a pericardiectomy might be suggested. This surgery removes part or all of the pericardium.
The treatment for pericardial diseases is tailored to the patient and the cause of the problem. Keeping a close eye on the patient is key to ensuring the treatment is working and catching any new problems.
“The key to successful management of pericardial diseases is a thorough understanding of the underlying cause and selecting the appropriate treatment strategy to address the specific needs of the patient.”
Treatment Modality | Purpose |
|---|---|
Anti-inflammatory Medications | Reduce inflammation and alleviate symptoms |
Colchicine | Prevent the recurrence of pericarditis |
Corticosteroids | Manage severe cases or when other medications are ineffective |
Pericardiocentesis | Drain excess fluid from the pericardial space |
Pericardiectomy | Remove part or all of the thickened and stiff pericardium |
Pericardial Diseases in Special Populations
Some groups of people face special challenges with pericardial diseases. Immunocompromised patients, like those with HIV or cancer treatment, are more at risk. They can get pericarditis from infections like tuberculosis.
People who have had heart surgery or a heart attack might get pericarditis later. This needs special care. Those with kidney problems or autoimmune diseases are also more likely to get pericardial diseases.
Population | Pericardial Disease Risk | Considerations |
|---|---|---|
Immunocompromised Patients | Increased susceptibility to infectious pericarditis | Requires vigilant monitoring and tailored treatment, including for conditions like tuberculosis |
Post-Cardiac Surgery Patients | Higher risk of post-cardiac injury syndrome and post-MI pericarditis | Needs specialized management and monitoring for these conditions |
Patients with Underlying Conditions | Increased propensity for pericardial diseases | Comprehensive evaluation and personalized care are essential |
Healthcare providers can better help these special groups by understanding their needs. This way, they can manage pericardial diseases well and prevent serious issues.
Complications of Pericardial Diseases
Pericardial diseases can lead to serious issues if not treated early. These problems can harm the heart’s function and overall health. They can even be life-threatening.
Cardiac tamponade is a big worry. It happens when fluid builds up around the heart too fast, making it hard for the heart to fill and pump. Constrictive pericarditis is another issue. It causes the pericardium to scar and thicken, hurting the heart’s ability to fill and work well.
Pericardial diseases can also cause heart failure. This is because the heart gets inflamed or compressed, and it can’t work properly. These diseases can also mess with the heart’s electrical signals, leading to arrhythmias.
It’s key to catch these diseases early and treat them right. This can stop serious problems. Early action can make a big difference. It lowers the risk of these big issues.
“Untreated or severe pericardial diseases can lead to various complications, including cardiac tamponade, constrictive pericarditis, heart failure, and arrhythmias. Prompt diagnosis and appropriate management are essential to prevent these potentially life-threatening issues.”
Prevention of Pericardial Diseases
Some pericardial diseases can’t be stopped, but we can lower the risk. Keeping infections away and treating them fast can stop infectious pericarditis. Getting vaccines for viruses like flu and COVID-19 can also help. A healthy life, managing health issues, and avoiding injuries can also prevent these diseases.
- Infection control: Treating infections quickly stops infectious pericarditis.
- Vaccination: Vaccines for flu and COVID-19 can lower the risk of viral pericarditis.
- Lifestyle modifications: Living healthy, managing health issues, and avoiding injuries help prevent pericardial diseases.
Acting early on causes and risks can greatly help prevent pericardial diseases.
“Preventing and promptly treating underlying infections is key to reducing the risk of infectious pericarditis.”
Preventive Measure | Rationale |
|---|---|
Infection control | Treating viral or bacterial infections can help prevent infectious pericarditis. |
Vaccination | Vaccines against common viral causes, such as influenza and COVID-19, may lower the risk of viral pericarditis. |
Lifestyle modifications | Maintaining a healthy lifestyle and avoiding activities that could lead to traumatic pericardial injury can help prevent pericardial diseases. |
Doing these things can lower our risk of getting pericardial diseases and keep our hearts healthy.
Prognosis and Recovery from Pericardial Diseases
The outcome and recovery time for pericardial diseases depend on the cause, severity, and treatment success. Most people with acute pericarditis get better with the right medicine in a week or two. However, chronic or recurring pericarditis might need ongoing care and could lead to serious issues like constrictive pericarditis.
Most people with pericardial diseases get better in 2 to 3 months if treated quickly. But, diseases caused by infections or cancer have a tougher outlook, depending on the disease itself.
About 15% to 50% of people who have had pericarditis before might get it again. This can lead to heart muscle scarring and thickening, known as constrictive pericarditis. Following up with doctors and sticking to the treatment plan is key for long-term health.
Genetics, lifestyle, and rare conditions can raise the risk of getting pericarditis and make it come back. Knowing these things helps doctors and patients make a good plan to deal with pericardial diseases.
In short, pericardial diseases have different outcomes and recovery times. But with quick and right treatment, most people do well. Monitoring health and following the treatment plan to prevent further problems is important.
Living with Pericardial Diseases
People with pericardial diseases might need to change their lifestyle to manage their condition well. These changes can lessen symptoms, stop complications, and boost well-being.
Activity Restrictions
Those with pericardial diseases might be told to skip hard exercise and competitive sports when they’re first sick. This helps avoid putting too much strain on the heart and lowers the chance of problems.
Symptom Management
It’s key to manage symptoms like chest pain and shortness of breath from pericardial diseases. Patients might need to take medicines, eat a low-sodium diet, and use other methods to ease their symptoms.
Regular Monitoring
Seeing a doctor regularly is important for those with pericardial diseases. These visits help monitor the condition, spot any issues early, and change treatment plans if needed.
Type of Pericardial Disease | Prevalence |
|---|---|
Pericarditis | About 28 people per 100,000 get this disease every year. |
Recurrent Pericarditis | 15 to 30% of people with the first episode get it again. |
Pericardial Effusion | This can cause cardiac tamponade, a serious condition where the heart can’t fill with blood. |
Constrictive Pericarditis | This is rare. It happens when fluid in the pericardium gets thick, and the layers stick together. |
Living with pericardial diseases means making lifestyle changes, managing symptoms, and seeing a doctor often. Knowing what you need to do helps you handle your condition better and live a good life.
“The key to managing pericardial diseases is to work closely with your healthcare team and be proactive in your care. With the right treatment and lifestyle adjustments, many individuals can lead fulfilling lives despite the challenges of their condition.”
Conclusion
Pericardial diseases include many conditions that affect the heart’s protective sac, the pericardium. Knowing the types, causes, symptoms, and treatments for these diseases is key. This knowledge helps with early diagnosis and better management.
Early spotting of symptoms like chest pain and pericardial effusion is important. It helps people get medical help fast and lowers the risk of serious problems.
Research and new treatments are improving care for pericardial diseases. Doctors from different fields are working together, and they’ve found new things, like how IL-1 affects pericarditis and how new treatments work.
As we learn more about pericardial diseases, early diagnosis and specific treatments become more important. This allows people to take charge of their heart health and manage their conditions well.
In short, knowing about pericardial diseases and how to deal with them is crucial. By being informed and getting medical help early, people can keep their hearts healthy and get better outcomes.
FAQ
What are the main types of pericardial diseases?
The main types include acute and chronic pericarditis, pericardial effusion, and constrictive pericarditis.
What are the common causes of pericardial diseases?
They can be viral or bacterial infections, autoimmune disorders, or cancer.
What are the typical symptoms of pericardial diseases?
Symptoms include sharp chest pain, a rub sound, ECG changes, and fluid buildup. This can cause shortness of breath and low blood pressure.
How are pericardial diseases diagnosed?
Doctors use ECG, echocardiogram, CT scans, and MRI to diagnose them. Sometimes, they need to analyze fluid or perform a biopsy.
What are the treatment options for pericardial diseases?
Treatments include drugs and surgery. The choice depends on the cause and how severe it is.
Are there any special considerations for certain populations with pericardial diseases?
Yes, people with weak immune systems or those with past heart surgery or heart attacks need special care. So do those with kidney problems or autoimmune diseases.
What are the potential complications of untreated or severe pericardial diseases?
Without treatment, these diseases can cause cardiac tamponade, constrictive pericarditis, heart failure, and arrhythmias.
How can pericardial diseases be prevented?
Prevention involves treating infections early, getting vaccines, and living healthy.
What is the prognosis and recovery timeline for pericardial diseases?
Outcomes depend on the cause, severity, and treatment. Acute cases usually have a good prognosis. However, chronic or infectious cases may be harder to treat.
What lifestyle adjustments may be necessary for individuals living with pericardial diseases?
People with these diseases may need to limit their activities, manage symptoms, and see their doctor regularly.