FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
About 3% of new cancer cases in the U.S. are multiple myeloma. This blood cancer affects plasma cells in the bone marrow. It’s a big deal, causing nearly 1.8% of all cancer deaths. Knowing about multiple myeloma is key to managing it well.
Multiple myeloma happens when plasma cells, a type of white blood cell, grow too much. These cells make antibodies to fight infections. But in myeloma, they grow out of control, making bad antibodies called M proteins. These cells stay in the bone marrow, not moving around in the blood.
Key Takeaways
- Multiple myeloma is a type of blood cancer that affects plasma cells in the bone marrow.
- Cancerous plasma cells, or myeloma cells, can be distributed throughout the bone marrow or occur in a single location.
- Myeloma cells produce abnormal antibodies called M proteins, which can lead to various complications.
- Understanding the nature of multiple myeloma is crucial for effective management of this complex disease.
- Treatments for multiple myeloma have significantly improved in recent years, leading to better outcomes for patients.
Treatments for multiple myeloma have gotten much better since the late 1990s. Now, we have therapies that work well and don’t hurt as much. These treatments include different phases, like induction and maintenance, and often include high-dose chemotherapy and stem cell transplants.
Supportive treatments help with the side effects of myeloma on bones. Sometimes, treatments like radiation or surgery are used for specific cases.
The Malignant Hematology Program at Moffitt Cancer Center is all about blood cancers, like multiple myeloma. A team of experts works together to care for patients with this tough disease.
What is Multiple Myeloma?
Multiple myeloma is a cancer that affects plasma cells in the bone marrow. Plasma cells help fight infections by making antibodies. But in multiple myeloma, these cells grow out of control and crowd out healthy cells.
Plasma Cells and Their Role
Plasma cells make antibodies to fight off infections. In multiple myeloma, these cells produce too much of one antibody. This can cause health problems.
Malignant Plasma Cell Growth
The bad plasma cells in multiple myeloma grow fast. They take over the bone marrow, making it hard for other cells to work right. This leads to many symptoms and problems.
Understanding plasma cells and their growth helps us see what multiple myeloma is.
Causes and Risk Factors
The exact cause of multiple myeloma is still a mystery. But, researchers have found some genetic mutations and risk factors. These can make someone more likely to get this blood cancer. Certain genetic changes can turn plasma cells into cancerous myeloma cells.
Genetic Mutations
Even though it’s not passed down through genes, having a family history can raise your risk. Also, those who had a solitary plasmacytoma before are more likely to get multiple myeloma.
Age and Gender
Most people get multiple myeloma when they’re over 65. Men are a bit more likely to get it than women.
Racial Disparities
African Americans face more than double the risk of getting multiple myeloma compared to white Americans. The Middle East, North Africa, and the Mediterranean also see more cases.
Working with harmful chemicals or radiation can increase your risk. This includes jobs in carpentry, furniture making, and paper manufacturing. Being overweight or obese also raises your risk.
Risk Factor | Increased Risk |
|---|---|
Age (over 65) | Majority of cases |
Gender (male) | Slightly higher risk |
Race (African American) | More than twice the risk |
Family history | Increased risk |
Solitary plasmacytoma | Higher risk of progression |
MGUS | Higher risk of progression |
Radiation exposure | Elevated risk |
Chemical exposure (benzene, pesticides, herbicides) | Elevated risk |
Obesity | Higher risk |
Symptoms of Multiple Myeloma
Multiple myeloma is a rare cancer. Its symptoms may not show up until it’s advanced. But as it gets worse, patients face many symptoms that hurt their life quality.
Bone pain, especially in the spine and ribs, is common. This pain can be very bad. It makes people weak, uncomfortable, and more likely to break bones. Patients also get sick more often, feel tired, and lose weight without trying.
As the disease gets worse, patients get “CRAB” symptoms. These include:
- Calcium (hypercalcemia)
- Renal dysfunction (kidney problems)
- Anemia
- Bone lesions
Anemia is often the first sign of multiple myeloma. It makes people short of breath, tired, and dizzy. It also causes leg swelling.
The disease can also cause fever, chills, and sweating. This makes people more likely to get sick. Low platelet count can cause easy bruising and bleeding.
Other symptoms include hypercalcemia and hyperviscosity syndrome. Hypercalcemia makes people feel sick to their stomach and weak. Hyperviscosity syndrome causes headaches and vision problems.
Cryoglobulinemia and renal failure are also symptoms. Cryoglobulinemia causes joint pain and skin problems. Renal failure makes people feel weak and have trouble breathing.
It’s important for patients to tell their doctors about any symptoms. Early treatment can make a big difference in how well patients do.
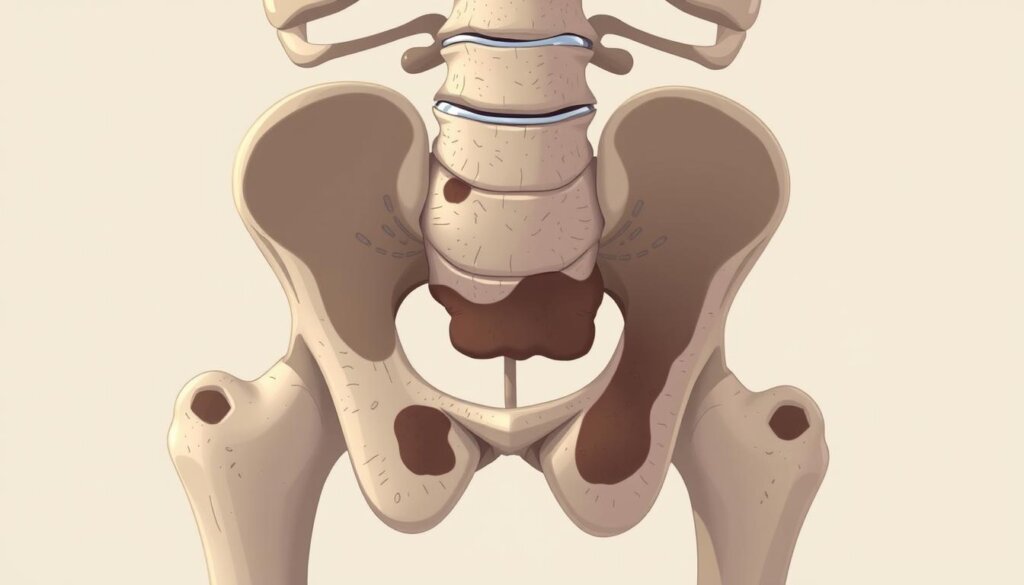
Bone Complications
Multiple myeloma can harm a patient’s bones a lot. It causes osteolytic lesions, which are weak spots in bones. These spots can make bones break easily, especially in the spine, pelvis, and ribs.
Myeloma cells also break down bones, leading to too much calcium in the blood. This is called hypercalcemia. High levels of calcium can cause confusion, nausea, and even coma if not treated.
Managing Bone Complications
There are treatments for bone problems in multiple myeloma. Bone-strengthening drugs like bisphosphonates and RANKL inhibitors can help. Radiation therapy can also shrink tumors and ease pain.
Doctors use different methods to manage pain, like opioids and antidepressants. They also suggest massage and acupuncture. But, it’s important to avoid NSAIDs because they can harm cancer treatments.
By treating bone issues in multiple myeloma, doctors can make patients’ lives better. They can also lower the chance of serious bone problems.
Anemia and Blood Cell Disorders
Multiple myeloma, a blood cancer, messes with bone marrow’s blood cell making. Anemia, a big problem, means fewer red blood cells. About 65% of patients have anemia when they’re first diagnosed. This can make them feel tired, weak, and short of breath.
Multiple myeloma also weakens the immune system by lowering white blood cells. This makes it easier to get sick. It also makes it harder for blood to clot, leading to more bleeding and bruising.
Anemia can be caused by many things, like iron deficiency, which makes you tired and short of breath. But, multiple myeloma doesn’t directly cause iron deficiency anemia. Even so, these two can happen together.
Other blood issues with multiple myeloma include sickle cell anemia and thalassemia. Sickle cell anemia changes red blood cells, causing blockages. Thalassemia might need blood transfusions for severe cases. Vitamin deficiency anemia, from low B-12 and folate, also affects red blood cells’ oxygen-carrying ability.
If you’re always tired or weak, get a blood test. Knowing and treating these blood issues is key to managing multiple myeloma well.
Kidney Impairment and Failure
Multiple myeloma, a common blood cancer, can harm the kidneys in up to 85% of patients. This happens because the extra M proteins from myeloma cells damage the kidneys. They stop the kidneys from filtering waste and extra fluids from the blood. In fact, kidney failure is the second biggest reason patients with multiple myeloma die after infections.
Kidney issues in multiple myeloma can show up in different ways. Cast nephropathy is when M proteins form casts that block the kidney tubules. It’s found in 40% to 60% of kidney biopsies in patients with multiple myeloma and kidney disease. Also, monoclonal gammopathies, including multiple myeloma, makeup about 1% to 2% of all cancers and just over 17% of blood cancers.
In the US, about 7 people per 100,000 males and females get multiple myeloma each year. Kidney failure affects 20% to 50% of these patients, either at the start or during the disease. Kidney problems in multiple myeloma mean a poor outlook and higher death rates.
Kidney Complications in Multiple Myeloma | Prevalence |
|---|---|
Kidney involvement at presentation | Up to 50% |
Cast nephropathy | 40% to 60% of renal biopsies |
Renal failure | 20% to 50% of patients |
People with diabetes, artery disease, infections, smoking, or dehydration are more likely to have kidney problems. These issues can get worse with chemotherapy and other treatments for multiple myeloma. It’s important to treat the myeloma quickly and well to manage kidney issues and avoid total kidney failure.
“Renal failure is the second most common cause of mortality in patients with multiple myeloma, after infections.”
Diagnosis and Staging
Diagnosing multiple myeloma is a detailed process. It includes blood and urine tests, and imaging. These steps confirm the disease and give insights into its stage and severity.
Blood and Urine Tests
Blood tests are key in diagnosing multiple myeloma. Doctors look for M proteins, which are abnormal antibodies from myeloma cells. They also check blood components like albumin and beta-2-microglobulin for disease clues. Urine tests find Bence Jones proteins, another myeloma marker.
Imaging Techniques
Doctors also use imaging to check multiple myeloma. X-rays, CT scans, and MRIs find bone lesions and disease stages. These scans are crucial for seeing bone damage and finding problem areas.
After testing, doctors stage the myeloma. This helps choose the best treatment. The Revised International Staging System (RISS) is used. It divides myeloma into stages based on blood tests and other factors.
Other things like kidney function and age also matter. Doctors use these to make a care plan for each patient.
“The Revised International Staging System is a critical tool not only for determining progression and intensity of treatment but also in discussing survival statistics with patients.”
Multiple Myeloma Treatment Options
Multiple myeloma can’t be cured, but there are ways to manage it. The main treatment for new cases includes induction therapy, stem cell transplant, and maintenance therapy. Induction therapy is a mix of drugs given over several weeks.
Stem cell transplants use the patient’s own cells. Maintenance therapy helps keep the disease from coming back. For those who relapse, there are different treatments based on their history.
Myeloma stages range from 1 to 3, with stage 1 growing slowly and stage 3 growing fast. Sometimes, no treatment is needed for smoldering myeloma. Treatments include targeted therapy, immunotherapy, and chemotherapy.
Solitary plasmacytomas are treated with radiation. Low-risk smoldering myeloma might not need immediate treatment. High-risk smoldering myeloma patients may get lenalidomide to prevent disease progression.
Active myeloma is treated with a mix of drugs. Standard-risk myeloma might get stem cell transplants or lenalidomide. High-risk myeloma patients often get a 4-drug regimen and stem cell transplants.
If the initial treatment fails, other options are tried. Newer treatments like BiTEs and CAR T-cell therapy are considered.
Conclusion
Multiple myeloma is a tough blood cancer that needs a team effort to manage well. We still don’t know all the causes, but new research and treatments have helped a lot. By knowing the signs, getting tested, and working with doctors, people with this cancer can help manage it better.
New treatments have made a big difference in fighting this cancer. These include thalidomide, lenalidomide, and bortezomib. They help avoid harsh treatments and make recovery better. Also, keeping up with these treatments can lead to longer, better health.
More research is key to finding the best treatments for everyone. Tailoring care to each person’s needs is also important. By staying updated and working with doctors, patients can face this disease with hope and better chances.
FAQ
What is multiple myeloma?
Multiple myeloma is a blood cancer. It affects the plasma cells in the bone marrow. Plasma cells help fight infections.
In multiple myeloma, these cells grow too much. They make bad antibodies called M proteins.
What causes multiple myeloma?
We don’t know exactly why multiple myeloma happens. But it might be due to genetic changes.
These changes make plasma cells turn bad. Age, gender, and race can also play a part.
What are the symptoms of multiple myeloma?
At first, multiple myeloma might not show any symptoms. But as it gets worse, you might feel bone pain.
You could also get infections easily, feel tired, or have kidney problems. Other symptoms include nausea, constipation, and feeling confused.
What are the bone complications associated with multiple myeloma?
Multiple myeloma can cause bone damage. This makes bones weak and more likely to break.
It can also lead to too much calcium in the blood. This is called hypercalcemia.
How does multiple myeloma affect the blood cells?
It messes with how blood cells are made. This can cause anemia, where you don’t have enough red blood cells.
It also weakens your immune system. This makes you more likely to get sick. And it can make it hard to stop bleeding.
How does multiple myeloma affect the kidneys?
The bad proteins from myeloma cells can hurt your kidneys. This can make your kidneys not work right.
In some cases, it can even cause kidney failure. More than half of people with myeloma will see their kidney function drop.
How is multiple myeloma diagnosed?
Doctors use blood and urine tests to find multiple myeloma. They also do imaging studies like X-rays and CT scans.
These tests help see if there are bone lesions. They also check how far the disease has spread.
What are the treatment options for multiple myeloma?
There’s no cure for multiple myeloma. But there are ways to manage it. Doctors might use chemotherapy, targeted drugs, or stem cell transplants.
They also offer supportive care to help with symptoms. The treatment plan depends on the disease’s stage and how it’s behaving.