FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
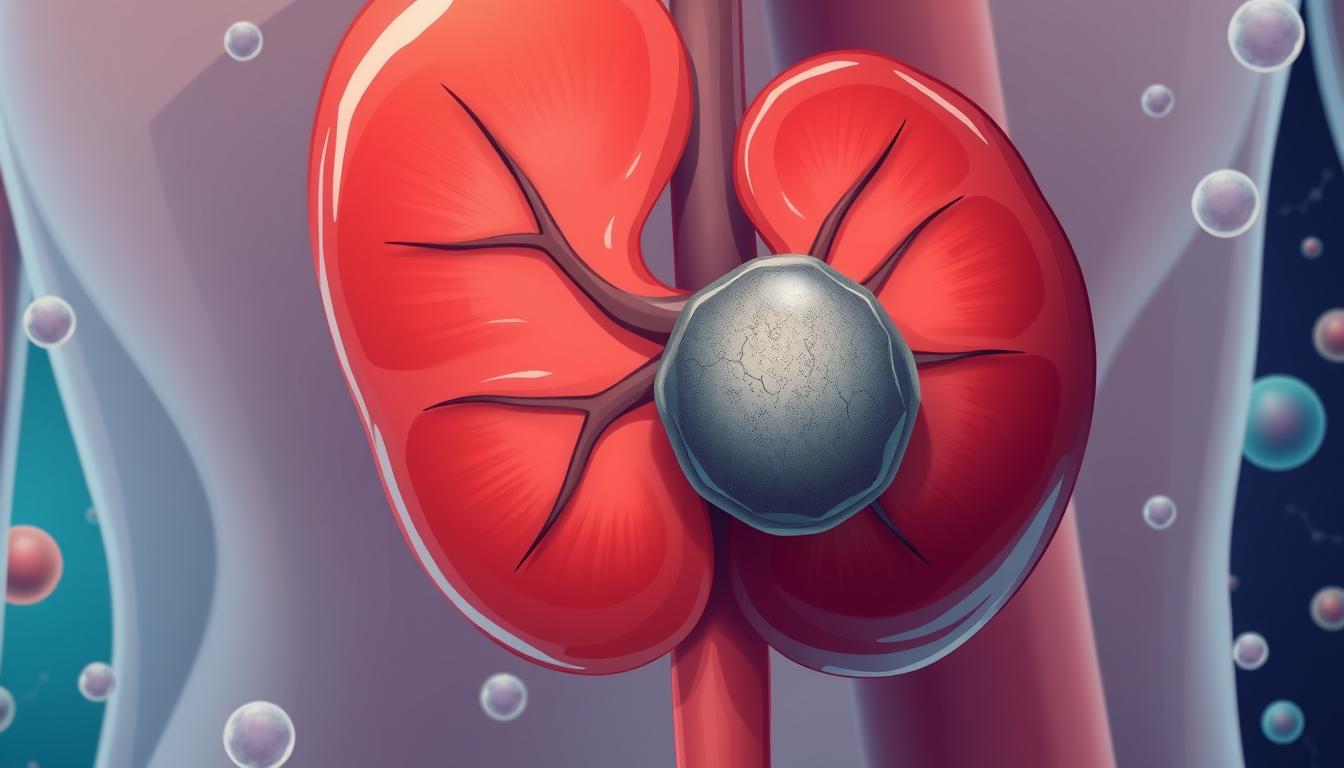
Kidney cancer is a big health problem. Renal cell carcinoma, or RCC, is the main type of kidney cancer. It makes up over 90% of all kidney cancers.
This cancer is common in adults in Europe. It happens in about 26 cases per 100,000 men and 12 cases per 100,000 women. Knowing about hypernephroma is key to managing it better.
Key Takeaways
- Renal cell carcinoma, or hypernephroma, is the most common type of kidney cancer in adults, accounting for over 90% of all renal malignancies.
- The incidence of RCC is higher in men than women, with a median age of diagnosis between 65 and 70 years for men and over 70 years for women.
- Clear cell carcinomas are the most prevalent subtype, representing 75-80% of kidney tumors, with diverse histological and genetic characteristics.
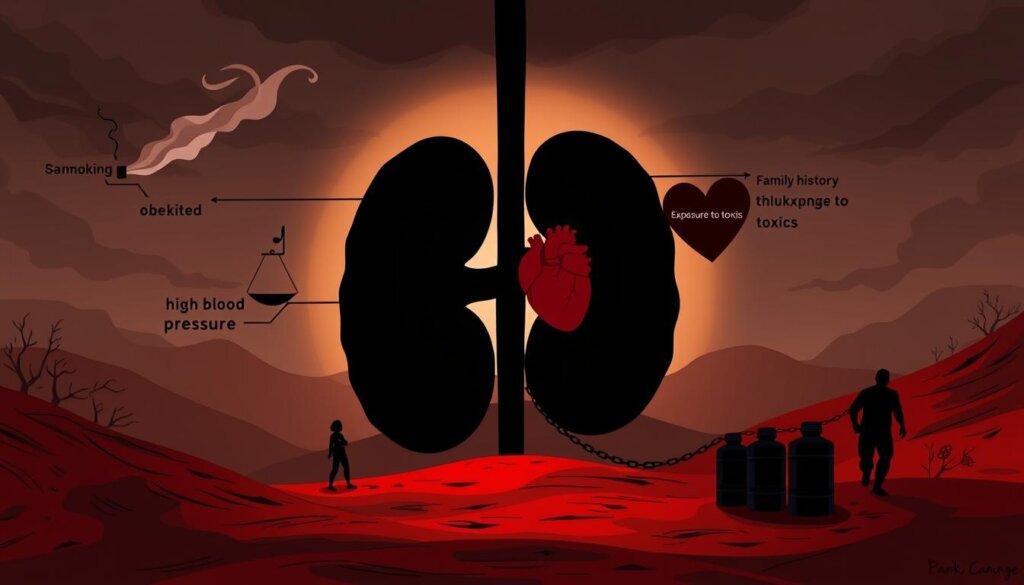
- Smoking, obesity, chronic kidney disease, and genetic factors are among the key risk factors for developing RCC.
- Advancements in diagnostic imaging and early detection have led to more cases being discovered incidentally, often at earlier stages.
Introduction to Renal Cell Carcinoma
Definition and Overview
Renal cell carcinoma (RCC) is the most common kidney cancer. It makes up over 90 percent of all kidney cancers. This cancer comes from the kidney’s cells and has many types.
RCC is mostly not caused by family history (~96%). It often happens between 50 to 70 years old. Men are more likely to get it than women, by a 2:1 ratio.
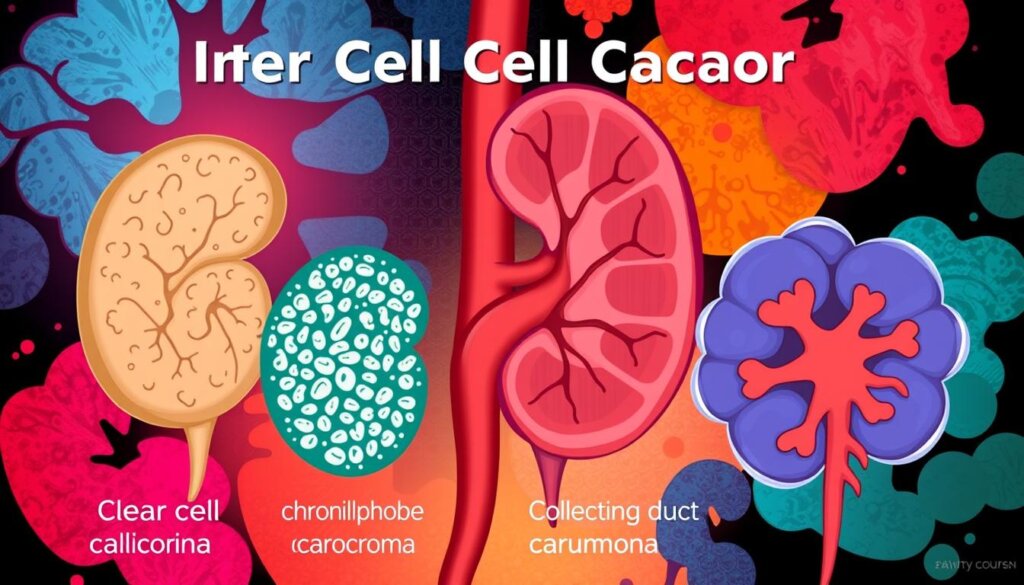
Types of Renal Cell Carcinoma
The main types of RCC are clear cell, papillary, and chromophobe. Each type has its own genetic changes. RCC cases have been rising since 1975.
More than half of RCC cases are found by accident. In 2020, 73,750 new cases were expected. RCC is most common in people aged 60 to 70.
Renal Cell Carcinoma Subtypes | Percentage of Cases |
|---|---|
Clear cell RCC | 70-80% |
Papillary RCC | 10-15% |
Chromophobe RCC | Around 5% |
For early-stage RCC, the 5-year survival rate is 93%. Early-stage patients make up about two-thirds of all cases. The survival rate for kidney and renal pelvis cancers is 75%.
Etiology: Risk Factors and Causes
Kidney cancer, also known as renal cell carcinoma (RCC), is a complex disease. It has many risk factors and causes. Knowing these is key to spotting who’s at higher risk and taking steps to prevent it.
Some main risk factors include environmental and lifestyle choices, as well as genetic and hereditary conditions.
Environmental and Lifestyle Factors
Smoking greatly increases the risk of kidney cancer. Being overweight and having high blood pressure also raise the risk. These can lead to hormonal changes that might cause the disease.
Working with certain chemicals, like trichloroethylene or cadmium, can also up the risk of RCC.
Genetic and Hereditary Conditions
About 4% of RCC cases are linked to rare hereditary conditions. If a family has a history of RCC, especially if a sibling has it, the risk goes up.
Conditions like von Hippel-Lindau (VHL) syndrome, hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome, and Birt-Hogg-Dubé (BHD) syndrome are genetic. They increase the risk of RCC.
Understanding RCC’s causes and risk factors helps people take action. They can lower their risk and catch the disease early. Regular health checks, lifestyle changes, and genetic counseling for those with a family history are all important.
Epidemiology: Incidence and Survival Rates
Renal cell carcinoma (RCC), the most common kidney cancer, has seen an increase since 1975. This is mainly because of better imaging that finds cancer early. In the U.S., there will be 81,610 new cases of kidney cancer in 2024. Sadly, 14,390 people will die from it.
The 5-year survival rate for kidney cancer is 75%. Early detection greatly improves these chances. The SEER database shows that survival rates are high for early-stage kidney cancer. They are 93% for localized, 74% for regional, and 17% for distant metastatic cancer.
Demographics play a big role in kidney cancer. Blacks face a higher risk and lower survival rates than others. On the other hand, Asian/Pacific Islanders have a lower risk and better survival rates. Men are more likely to get kidney cancer and have lower survival rates than women.
Demographic Factor | Incidence Rate | Survival Rate |
|---|---|---|
Blacks | Significantly higher | Lower than other races |
Asian/Pacific Islanders (A/PI) | Lower compared to other races | Higher |
Males | About twice the rate of females | Lower than females |
Kidney cancer incidence has gone up, but survival rates have improved. This is due to better detection and treatment. Yet, there are big disparities in who gets kidney cancer and who survives. We need more research and targeted help to fix these issues.
“The ability to identify high-risk individuals and detect kidney cancer at an early, localized stage is crucial for improving survival rates and reducing the burden of this disease.”
Pathophysiology of Hypernephroma
Genetic Alterations and Molecular Signatures
Renal cell carcinomas (RCCs) start from the nephron’s epithelial cells. Clear cell RCC (CCRCC) comes from the proximal tubule. Papillary RCC (PRCC) comes from the distal tubule. Chromophobe RCC (ChRCC) comes from the collecting duct’s intercalated cells.
The genetic changes and molecular signs in RCC types help us understand and classify them.
CCRCC often loses part of chromosome 3, where the VHL gene is. PRCC has MET gene mutations and extra chromosomes. ChRCC loses many chromosomes, including 1, 2, 6, 10, 13, 17, and 21.
These changes help us classify RCC types and understand their causes. They also show us where to find new treatments.

“The genetic alterations and molecular signatures observed in different RCC subtypes are crucial for their classification and understanding.”
RCC Subtype | Genetic Alterations |
|---|---|
Clear Cell RCC (CCRCC) | Loss of short arm of chromosome 3 (3p), where VHL gene is located |
Papillary RCC (PRCC) | MET gene mutations, chromosomal trisomies |
Chromophobe RCC (ChRCC) | Loss of multiple chromosomes (1, 2, 6, 10, 13, 17, 21) |
Studying renal cell carcinoma, or hypernephroma, is complex. It involves many areas of research. Knowing the genetic and molecular signs of RCC types is key to better understanding and treating the disease.
Histopathology of Renal Cell Carcinoma
Renal cell carcinoma (RCC) is a complex disease with many types. The World Health Organization (WHO) lists over 14 types of RCCs. Each type has its own genetic, molecular, and clinical features.
The main types are clear cell RCC (CCRCC), papillary RCC (PRCC), and chromophobe RCC (ChRCC). These types make up most of the cases.
Clear Cell Carcinoma
CCRCC is the most common type, making up 70-80% of RCCs. It has clear or pink granular cytoplasm and lots of blood vessels. This makes it look different under a microscope.
CCRCC is linked to the VHL gene being turned off. This leads to more blood vessels forming.
Papillary Carcinoma
PRCC makes up 10-15% of RCCs. It has two types based on how it looks. Type 1 has thin blood vessels and small cells. Type 2 has big cells and lots of nucleoli.
The different looks of RCC types show their genetic and molecular changes. These changes affect how well the cancer will do and how it should be treated. Knowing about RCC’s histopathology is key for making the right diagnosis and treatment plan.
Symptoms and Diagnosis of Kidney Cancer
Kidney cancer, also known as renal cell carcinoma, often lacks clear symptoms in its early stages, making it challenging to diagnose. As the cancer progresses, patients may experience symptoms such as blood in the urine, pain in the back or side, loss of appetite, unexplained weight loss, persistent fatigue, and fever or night sweats.
To diagnose kidney cancer, healthcare providers may order a variety of tests, including blood and urine tests. These tests can detect anemia, which is very common in people with kidney cancer, as well as polycythemia (having too many red blood cells), which is less common. High levels of blood platelets, neutrophils, calcium, lactate dehydrogenase (LDH), or liver enzymes may also be observed in individuals with kidney cancer.
In addition to blood and urine tests, healthcare providers often utilize imaging studies, such as ultrasound, X-ray, CT scan, and MRI, to detect and evaluate kidney tumors. In some cases, a biopsy may be performed to confirm the diagnosis and determine the specific subtype of renal cell carcinoma.
The grade of the renal cell cancer, ranging from 1 to 4, is an important factor in determining the prognosis. Grade 1 renal cell cancers have cells that closely resemble normal kidney cells and tend to have a good prognosis, while Grade 4 renal cell cancers have cells that look significantly different from normal kidney cells and often have a worse prognosis.
Early detection and accurate diagnosis are crucial for effective treatment of kidney cancer. By understanding the symptoms and undergoing appropriate diagnostic tests, individuals can take proactive steps towards managing this challenging form of cancer.
“Kidney cancer is often caught incidentally, when a patient is being evaluated for an unrelated condition. This makes early diagnosis challenging, but also highlights the importance of regular check-ups and screening for high-risk individuals.”
Staging and Prognosis of Hypernephroma
The TNM Staging System
Kidney cancer, or renal cell carcinoma (RCC), is staged using the TNM system. The stages range from I to IV. Stage I means a small tumor in the kidney. Stage IV means the cancer has spread far away.
Lower stage numbers mean less cancer spread. Higher numbers mean more spread.
The TNM system looks at the tumor’s size, spread, and if it’s in lymph nodes or distant organs. This helps decide the best treatment and gives a good idea of the patient’s chances.
Stage | Description |
|---|---|
Stage I | The main tumor is no more than 7 centimeters across and is limited to the kidney. |
Stage II | The main tumor is larger than 7 cm across but still confined to the kidney. |
Stage III | The tumor may have grown into a major vein or surrounding tissue, with or without lymph node involvement, but there is no spread to distant organs. |
Stage IV | The tumor has grown beyond the kidney’s boundaries, potentially involving nearby lymph nodes or distant metastasis. |
There are also prognostic models like the MSKCC model and the IMDC criteria. They group advanced kidney cancer into low-, intermediate-, and high-risk groups. These groups are based on factors like blood LDH level and time from diagnosis to treatment.
These models help guide treatment and give insights into the patient’s prognosis.
The prognosis for kidney cancer depends a lot on the stage at diagnosis. If caught early, kidney cancer can often be cured. But, it’s harder to treat when it spreads.
The 5-year survival rates in the US are 93.2% for localized, 76.1% for regional, and 17.8% for distant disease.
Knowing about kidney cancer staging and prognosis is important for both doctors and patients. It helps make treatment plans and sets realistic hopes for the disease’s course. Regular monitoring and early detection are key to better outcomes for those with this cancer.
Treatment Options for Renal Cell Carcinoma
Kidney cancer, also known as renal cell carcinoma (RCC), is the most common type of kidney cancer. It makes up about 9 out of 10 cases. The overall 5-year survival rate for kidney and renal pelvis cancer in the United States is 76.5%.
Treatment options for RCC depend on the stage of the cancer. If caught early, before it spreads outside the kidney, there’s a better chance of a cure.
Surgical Management
Surgery is the most effective treatment for RCC. Options include partial nephrectomy, simple nephrectomy, and radical nephrectomy. After surgery, adjuvant therapy like sunitinib and pembrolizumab may be recommended to lower the risk of cancer coming back.
Non-surgical Treatments
For RCC that can’t be removed by surgery or has spread, other treatments include immunotherapy and targeted therapy. Cryotherapy, thermal ablation, SBRT, and arterial embolization are also options. These treatments can slow the disease’s progression and manage symptoms, even if a complete cure is not possible.
Early detection of kidney cancer is key to improving cure chances. Symptoms include fatigue, weight loss, blood in the urine, and back pain. If the cancer hasn’t spread outside the kidney, a complete cure is possible. But if it has metastasized, treatment can slow its progression and manage symptoms.
People who have a nephrectomy can live with one kidney. They might not need a special diet. But if the remaining kidney gets injured or fails, dialysis or a kidney transplant might be needed.
“The best treatment approach depends on various factors, including the stage and subtype of RCC, the patient’s overall health, and their individual preferences.”
Treatment Option | Description | Effectiveness |
|---|---|---|
Partial Nephrectomy | Removal of the tumor while preserving the kidney | Effective for early-stage RCC, 5-year survival rate of 93% |
Radical Nephrectomy | Removal of the entire kidney, adrenal gland, and surrounding lymph nodes | Effective for more advanced RCC, 5-year survival rate drops to 72.3% if cancer has spread to lymph nodes |
Immunotherapy | Drugs that boost the body’s immune system to fight cancer, such as nivolumab and pembrolizumab | Effective for advanced or metastatic RCC, can help slow disease progression |
Targeted Therapy | Drugs that target specific molecules involved in cancer growth and progression, such as lenvatinib and cabozantinib | Effective for advanced or metastatic RCC, can help slow disease progression |
In summary, the treatment options for renal cell carcinoma (RCC) vary based on the stage and severity of the disease. Early detection is crucial, as kidney cancer caught in its early stages has a higher chance of being.,
Conclusion
Kidney cancer, also known as hypernephroma or renal cell carcinoma, is common in adults. It’s important to know about its risks, symptoms, and treatments. This knowledge helps manage the disease better and improves chances of recovery.
Early detection is hard, but new medical tools and treatments help. They work best for those with cancer that hasn’t spread far.
Working with a team of doctors helps create a treatment plan for each person. This plan aims to meet their specific needs and increase their recovery chances. Understanding how kidney cancer affects the immune system is key. This knowledge helps doctors treat the disease more effectively.
Research and new discoveries in kidney cancer treatment are ongoing. This means doctors can offer better care and improve patient outcomes. This is good news for those facing this tough disease.
Early detection and quick treatment are key for a good outcome. Regular health checks and talking to your doctor are important. They help catch kidney cancer early and manage it well. By being proactive in your health, you can do a lot to stay well and get the best results.
FAQ
What is hypernephroma, and how is it related to kidney cancer?
Hypernephroma is another name for renal cell carcinoma (RCC). It’s the most common kidney cancer in adults. It makes up over 90% of all kidney cancers.
What are the major histological subtypes of renal cell carcinoma?
RCC has three main types: clear cell RCC, which accounts for 70-80% of cases; papillary RCC, which accounts for 10-15%; and chromophobe RCC, which accounts for about 5% of cases. Each type has its own genetic changes.
What are the risk factors for developing renal cell carcinoma?
Smoking, obesity, and high blood pressure are big risks. Chemicals like trichloroethylene also raise the risk. Rare genetic conditions like VHL syndrome cause about 4% of RCC cases.
What is the incidence and survival rate for kidney and renal pelvis cancers?
RCC cases have gone up since 1975. In 2024, there will be 81,610 new cases in the U.S. The 5-year survival rate is 75%. Early diagnosis helps a lot.
What are the key genetic alterations and molecular signatures associated with different RCC subtypes?
CCRCC often loses part of chromosome 3, where VHL is. PRCC has MET gene mutations. ChRCC loses many chromosomes, including 1, 2, 6, 10, 13, 17, and 21.
What are the common symptoms of kidney cancer, and how is it typically diagnosed?
Early kidney cancer often has no symptoms. Later, symptoms like blood in urine and pain may appear. Doctors use tests like ultrasound and CT scans to find it.
How is renal cell carcinoma staged, and how does the stage affect prognosis?
RCC is staged using the TNM system. It looks at the tumor size, lymph node involvement, and metastases. Stage I is a small tumor, and stage IV is advanced. Early stages have better survival rates.
What are the main treatment options for renal cell carcinoma?
Surgery is the main treatment for RCC. This can be removing the whole kidney or just the tumor. For advanced cases, treatments like targeted therapy and immunotherapy are used.