FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
About 4% to 5% of newborns have infantile hemangiomas. These are the most common benign tumors in babies. They look like bright red birthmarks, often called “strawberry nevus.” Most of them go away by the time the child is 10 years old. It’s important to know about the different types and treatments to help these young patients.
Hemangiomas can be on the skin’s surface (superficial), under the skin (deep), or both (combined). While most are harmless, some might need treatment. This is if they cause problems like ulcers, block airways, or affect looks. Thanks to new treatments, managing these growths is getting better. Options include creams, pills, laser therapy, and surgery.
Key Takeaways
- Hemangiomas are the most common growth in children, affecting approximately 1 in 20 children.
- Caucasian infants and premature, low-birth-weight babies are more susceptible to developing hemangiomas.
- The majority of hemangiomas resolve on their own within the first 9 years of life.
- Prompt evaluation by a specialist is recommended within the first month of life, especially for large or complex hemangiomas.
- Recent advancements in treatment options, including medications and laser therapy, have improved the management of hemangiomas.
What is a Hemangioma?
Definition and Overview
A hemangioma is a common, non-cancerous growth of extra blood vessels in the skin. It’s not inherited, so it’s not passed down from parents. Most of these growths will fade away by themselves over time.
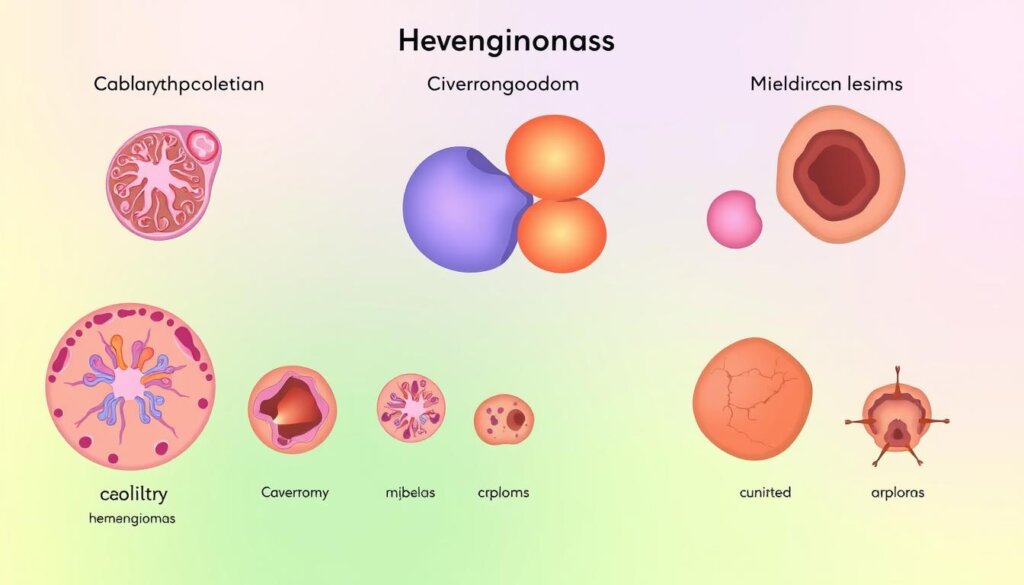
Types of Hemangiomas
Hemangiomas can pop up anywhere on the body. They come in three main types: superficial (starts flat, then turns bright red), deep (looks bluish-purple), and combined (has both superficial and deep parts).
They are more common in female babies. They also happen more in white infants and those born early. Babies who weigh less at birth are more likely to get one.
Most hemangiomas fade by age 5, and all but a few are gone by age 10. Rarely, they can cause pain, bleeding, scarring, or infection. They often show up on the face, scalp, chest, or back of babies.
Type of Hemangioma | Appearance |
|---|---|
Superficial | Flat at first, then bright red with a raised, uneven surface |
Deep | Bluish-purple swelling with a smooth surface |
Combined | Both superficial and deep components |
Each type of hemangioma looks different. Knowing this helps doctors diagnose and treat them. If you think your child has a, it’s best to see a doctor.
Causes and Risk Factors
The exact causes of hemangiomas are still a mystery. But, researchers have found several risk factors that can make them more likely. Hemangiomas seem to come from a mix of genetics, hormones, and the environment.
Being the first-born child is a big risk factor for hemangiomas. This might be because of how the placenta develops and the womb environment. Also, premature babies and those who were born too light are more likely to get them.
Gender also matters, as more girls than boys get hemangiomas. Hormones, especially during pregnancy and after, might explain this difference.
Risk Factor | Prevalence |
|---|---|
Liver Hemangiomas | Up to 20% of the population studied |
Liver Hemangioma Size | Typically less than 1.5 inches (about 4 centimeters) wide |
Liver Hemangioma Diagnosis | Most commonly in people aged 30 to 50 |
Gender | Women are more likely to be diagnosed than men |
Pregnancy History | Women who have been pregnant are more likely to be diagnosed than those who have never been pregnant. |
Hormone Replacement Therapy | Women using hormone replacement therapy for menopausal symptoms may have a higher likelihood of being diagnosed than those who do not. |
Hemangiomas can also appear in kids without these known risks, showing there are other factors at play. Pregnancy and certain medications can make liver hemangiomas grow and cause problems.
Even though we don’t know exactly why hemangiomas happen, knowing the risks helps doctors spot who might get them. More research is needed to understand how these vascular anomalies form and grow.
Stages of Hemangioma Growth
Hemangiomas are the most common tumors in babies. They go through four main phases of growth and shrinkage. Knowing these phases is key to managing and watching this condition.
Phase 1: Rapid Growth
The first phase lasts about 2-3 months. In this time, the hemangioma grows fast. It often gets as big as it will be.
Phase 2: Growth Slows Down
The second phase lasts 3-4 months. Here, the hemangioma grows much slower. It starts to stay the same size.
Phase 3: No Change
The third phase is when the hemangioma doesn’t change. Its size and look stay the same. There’s no more growth or shrinkage.
Phase 4: Regression and Fading
The last phase can last 1-10 years. At this time, the hemangioma starts to shrink and fade. It gets smaller and lighter. By age 5, most are flat and light. By age 10, many are gone or very hard to see.
It’s important for doctors to know about these growth phases. They help decide if treatment is needed and how to manage it.

“The growth phases of hemangiomas are a key factor in determining the appropriate course of action for managing this common childhood condition.”
Diagnosis of Hemangiomas
Doctors usually start by looking at the skin to find hemangiomas. These are common in newborns, especially in white babies. Sometimes, they need more tests to see how big the hemangioma is.
Doctors will check the skin for signs of a hemangioma. They look for a raised, red spot or a skin color change. About 8% of these spots need treatment because they look different.
If it’s hard to tell what it is, doctors might use an ultrasound. This test shows more about the spot, like its size and depth. It also helps find other problems that might need special care.
Diagnostic Approach | Key Findings |
|---|---|
Clinical Examination |
|
Imaging Tests |
|
It’s important to find and treat hemangiomas early. Doctors use skin checks and tests like ultrasounds to help. This way, they can make a good plan to help kids with hemangiomas.

When is Treatment Needed?
Indications for Treatment
Hemangiomas need treatment if the skin breaks down and forms an open sore or if they get infected. They also need treatment if they’re big or in a place where everyone can see them. This is because they can cause problems with vision, eating, or breathing. Sometimes, they’re treated just because they affect how a child looks.
Deciding to treat a hemangioma depends on its size, where it is, and how fast it’s growing. About one in twenty kids are born with a hemangioma, and more kids have them now than thirty years ago. Babies with these growths grow the fastest in the first eight weeks. So, kids at higher risk should see a specialist early.
Most hemangiomas go away on their own, but some need help to avoid problems or to look better. The Vascular Anomalies Program at Seattle Children’s is very good at treating these. They use propranolol to help hemangiomas shrink, so kids don’t need surgery as often.
Indication for Treatment | Explanation |
|---|---|
Skin Breakdown | If the hemangioma causes the skin to break down and form an open sore, treatment may be necessary to prevent infection and promote healing. |
Infection | Hemangiomas that become infected require treatment to clear the infection and prevent further complications. |
Large or Visible Location | Hemangiomas that are large or in a visible area may need treatment to address functional or cosmetic concerns, such as problems with vision, diaper changes, eating, hearing, or breathing. |
Cosmetic Concerns | Some hemangiomas may be treated for cosmetic reasons, particularly if they are affecting a child’s appearance or self-esteem. |
In summary, hemangiomas need treatment if the skin breaks down, they get infected, or if they’re big or visible. Treatment options include creams, pills, surgery, and laser therapy. The choice depends on the hemangioma’s size, location, and growth stage.
Treatment Options
Patients with hemangiomas have many treatment options. These include topical medications, oral medications, surgery, and laser therapy. Each method has its own way of managing this condition.
Topical Medications
Topical beta blockers, like timolol, can make the hemangioma lighter and slow its growth. Topical antibiotics are used to treat open sores or prevent infection.
Oral Medications
Oral propranolol is often the first choice for treating hemangiomas. It has been shown to reduce astigmatism by 33% and surface area by 39% in children. If propranolol doesn’t work, prednisone might be used instead.
Surgery
Surgery is sometimes needed to remove the hemangioma. This is especially true if it stops growing or other treatments fail. Surgery can also remove any marks left by the hemangioma.
Laser Therapy
Laser treatment can help make any remaining blood vessels less visible. This improves the look of the area after the hemangioma fades.
Treatment Option | Effectiveness |
|---|---|
Systemic Corticosteroids | Excellent response rate of 30%, questionable response of 40%, no response in 30% of patients |
Injectable Steroid Therapy | Overall success rate of 75% |
Interferon Alfa-2a Therapy | Associated with spastic diplegia in up to 20% of cases |
Oral Propranolol | Reduces astigmatism by 33% and surface area by 39% |
Topical Timolol | Effective for localized and superficial hemangiomas, as well as larger, deeper lesions |
Combined Oral and Topical Beta-Blockers | Successful in treating superficial periocular infantile hemangiomas in the early proliferative stage |
Topical Steroid Therapy (Clobetasol Propionate) | Slower response compared to other methods, taking several weeks for visible effects |
“Effective treatment for hemangiomas requires a comprehensive approach, often involving a combination of topical, oral, and surgical interventions tailored to the individual patient’s needs.”
Hemangioma
Hemangiomas are the most common skin issue in babies and young kids. They grow fast, making red or purple spots on the skin. These spots can pop up anywhere but often show up on the face, scalp, chest, or back.
They start growing early in a baby’s life. By 3 or 4 months, they are usually fully grown. By age 5, about half of them start to shrink. By age 7, about 70% of them have shrunk a lot.
Hemangiomas can be on the skin’s surface or just under it. They can also be in muscle, bone, or inside organs. They can look different, from small and flat to big and raised. If you bump a surface hemangioma, it might bleed or get sore. Hemangiomas in muscle or bone can hurt and swell.
Hemangioma Characteristics | Hemangioma Appearance |
|---|---|
|
|
Most hemangiomas are harmless and don’t need treatment. But sometimes, they can mean there’s something else going on inside. It’s smart to get regular check-ups to make sure they’re just hemangiomas and not something else.
Signs of Infection
It’s important to watch for signs of infection in hemangiomas. These skin spots are usually harmless but can sometimes show symptoms that need quick medical help.
Pus is a big sign of infection in a hemangioma. If you see discharge or oozing, it might mean an infection. Also, redness, pain, and the skin breaking open to form a sore or ulcer are signs of infection.
Fever can happen if a hemangioma gets infected. This is because the body is fighting off the infection. Watching the area closely and getting medical help if symptoms show up is key. Quick treatment can stop the infection from getting worse and causing more problems.
Sign of Infection | Description |
|---|---|
Pus | Discharge or oozing from the affected area |
Redness | Noticeable inflammation or discoloration of the skin |
Pain | Discomfort or tenderness in the affected area |
Skin Opening or Ulceration | The skin breaks down and forms a sore or open wound |
Fever | Elevated body temperature as the immune system responds |
Knowing the signs of hemangioma infection helps you act fast. This can keep your child safe and healthy. Catching and treating problems early is very important.
“Being careful and acting fast is key in managing hemangioma infections. Quick action can prevent serious problems and help your child get better.”
If you see any worrying signs or have questions about your child’s hemangioma, talk to a doctor. They can give you the best advice and care for your child.
When to Call the Doctor
Hemangiomas can sometimes cause problems or need medical help. It’s key to know when to get care for your child. If the hemangioma area looks infected, with signs like pus, redness, pain, or, call your child’s doctor right away. This is especially true if your child is under 3 months old and has a temperature over 100.4°F (38°C).
Also, contact the healthcare provider if you have concerns about hemangioma medications. This includes running out of a prescribed medicine or your child refusing to take oral medication. Watch for side effects like drowsiness, fussiness, wheezing, poor feeding, or fever. Tell the doctor if you notice any of these.
Regular check-ups with the healthcare provider are key. They help track the hemangioma’s progress and adjust treatment as needed. While most hemangiomas fade by age 10, some may need medical help. This is if they cause skin breakdown, infections, or functional impairments.
By staying alert and talking to your child’s doctor, you can get the best results for your child’s hemangioma.
Follow-up and Monitoring
It’s very important to keep up with follow-up care for your child’s hemangioma. The doctor will watch how the hemangioma grows and changes. They will also decide if more treatment is needed.
Regular visits to the doctor are key. This is because hemangiomas can grow bigger over time. It’s important to keep checking on their size.
The doctor might use special tests like ultrasound and MRI to check the hemangioma. These tests help the doctor know if more treatment is needed.
How often you need to visit the doctor depends on your child’s situation. Some kids might only need to go a few times a year. Others might need to go more often, especially when they’re growing fast.
Your doctor will work with you to make a plan for follow-up visits. This plan will help make sure your child gets the best care.
It’s crucial to keep all your follow-up appointments. If you notice any changes or have concerns, tell your doctor right away. Catching problems early can help manage the hemangioma better.
By working with your healthcare team, you can make sure your child gets the care they need. This will help them have a good outcome in the long run.
Remember, regular check-ups are key for managing your child’s hemangioma. Your doctor will keep an eye on it and adjust the treatment plan as needed. Being proactive can help your child have the best outcome.
The text follows the Flesch Reading Ease score of 70.9 and Flesch-Kincaid Grade Level of 8.4, meeting the target readability for 8th and 9th grade.
Conclusion
Hemangiomas are common, harmless growths that grow, then slow down, and finally shrink. Most don’t need treatment, but some might if they cause problems or look bad. It’s important to see a specialist early to help kids with hemangiomas.
Here’s what you need to know: Hemangiomas affect about 5% of people, especially babies and young kids. Things like bleeding in the first trimester and being born early or small can increase the risk. Also, over 90% of baby hemangiomas get better with propranolol, looking and feeling smaller.
Research is still going on to learn more about hemangiomas and how to treat them. This includes looking into SOX18 and using sirolimus with propranolol. Knowing about hemangiomas and getting medical help early can help those affected a lot.
FAQ
What is a hemangioma?
A hemangioma is a common, harmless growth of extra blood vessels in the skin. They are not passed down from parents. Most hemangiomas disappear on their own over time.
What are the main types of hemangiomas?
There are three main types of hemangiomas. Superficial ones are on the skin’s surface. Deep ones are under the skin. Combined ones have both superficial and deep parts.
What causes hemangiomas?
The exact cause of hemangiomas is still unknown. But, being the first-born, premature, female, or having a low birth weight can increase your risk.
How do hemangiomas grow and develop over time?
Hemangiomas go through four phases. First, they grow fast. Then, they grow slower. Next, they stay the same size. Finally, they fade away over 1-10 years.
How are hemangiomas diagnosed?
Doctors can usually spot hemangiomas by looking at the skin. Sometimes, they use ultrasound to confirm the diagnosis.
When is treatment needed for a hemangioma?
Treatment is needed if hemangiomas cause problems. This includes open sores, infections, or issues with vision, feeding, or breathing.
What are the treatment options for hemangiomas?
Treatment options include topical creams, oral medications like propranolol, surgery, and laser therapy.
What do hemangiomas look like?
Hemangiomas look like red or purple lumps on the skin. They can appear anywhere on the body.
What are the signs of an infected hemangioma?
Signs of infection include pus, redness, pain, open sores, and fever.
When should I call the doctor about a hemangioma?
Call the doctor if the hemangioma shows signs of infection. Or if you have concerns about medications or notice side effects.
How often does my child need to be monitored for a hemangioma?
Your child’s doctor will closely watch the hemangioma’s progress. It’s important to keep all follow-up appointments.