FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Gestational trophoblastic disease (GTD) affects about one in every 1,000 pregnant women in the U.S. This rare group of tumors may sound scary, but most are not cancerous. Knowing about GTD’s types, causes, symptoms, and treatments can help clear up confusion and offer hope.
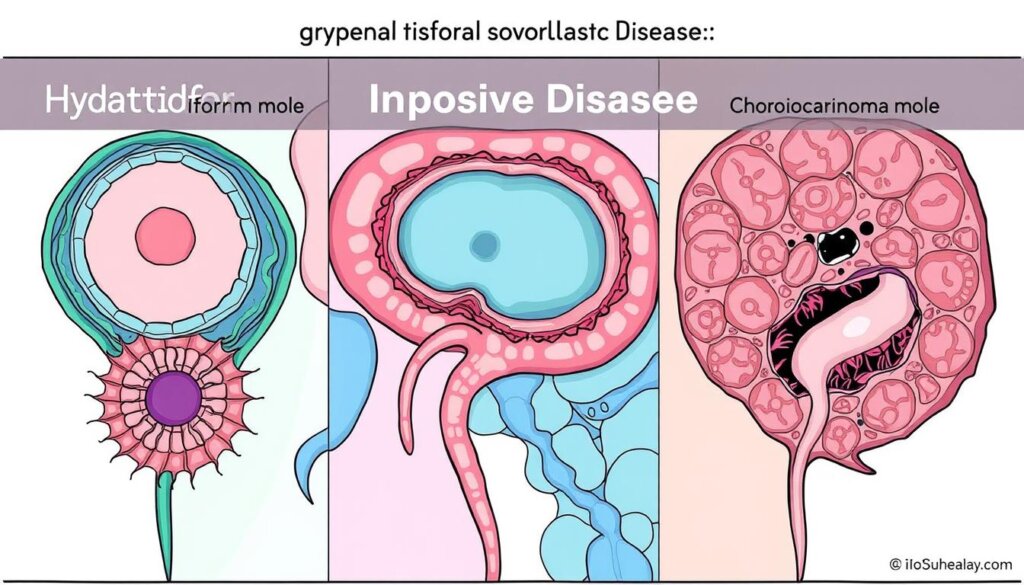
GTD comes from too much growth of trophoblast cells, which make the placenta. These cells can grow too much, leading to either non-cancerous or cancerous tumors. The main types of GTD are hydatidiform moles (molar pregnancies) and gestational trophoblastic neoplasia (GTN). GTN includes serious forms like choriocarcinoma and others.
Key Takeaways
- Gestational trophoblastic disease (GTD) is a rare group of tumors that develop during early pregnancy.
- GTD can be either benign (non-cancerous) or malignant (cancerous).
- The two main types of GTD are hydatidiform moles (molar pregnancies) and gestational trophoblastic neoplasia (GTN).
- Risk factors for GTD include maternal age, previous molar pregnancy, and history of miscarriage.
- Common symptoms of GTD include abnormal vaginal bleeding, larger-than-usual uterus, and severe nausea/vomiting.
What is Gestational Trophoblastic Disease?
Gestational trophoblastic disease (GTD) is a rare group of tumors that grow in early pregnancy. They come from trophoblast cells, which are meant to form the placenta. GTD can be either benign (non-cancerous) or malignant (cancerous). It’s divided into two main types: hydatidiform moles and gestational trophoblastic neoplasia (GTN).
Benign and Malignant GTD
Hydatidiform moles are the most common type of GTD and are usually benign. But, about one in five complete hydatidiform moles can turn cancerous. On the other hand, choriocarcinomas, placental-site trophoblastic tumors (PSTTs), and epithelioid trophoblastic tumors (ETTs) are malignant forms of GTD. These cancerous GTD tumors can spread and need aggressive treatment.
Type of GTD | Characteristics |
|---|---|
Hydatidiform Moles (Molar Pregnancies) |
|
Gestational Trophoblastic Neoplasia (GTN) |
|
In summary, GTD is a rare group of tumors that grow in early pregnancy. They come from trophoblast cells. GTD can be benign or malignant. Hydatidiform moles are the most common, and GTN is the more serious, cancerous form.
Types of Gestational Trophoblastic Disease
Gestational trophoblastic disease (GTD) is a rare condition. It happens when cells in the placenta grow abnormally during pregnancy. There are two main types: Hydatidiform Moles (Molar Pregnancies) and Gestational Trophoblastic Neoplasia (GTN).
Hydatidiform Moles (Molar Pregnancies)
Hydatidiform moles (HMs) are the most common GTD. They happen in about 2 in 1,000 pregnancies in Southeast Asia and Japan. In the United States, the rate is about 1 in 600 abortions and 1 in 1,500 pregnancies.
HMs can be complete or partial and are usually not cancerous. But, 15-20% of HMs can turn into cancer, needing chemotherapy after surgery.
Older women and those younger than 21 are at higher risk for molar pregnancies. Having had a molar pregnancy before increases the risk of getting another one by about 1%. Also, a history of miscarriage can double or triple the risk of molar pregnancy. The chance of a third mole after two previous ones is 15-20%.
Gestational Trophoblastic Neoplasia (GTN)
Gestational trophoblastic neoplasia (GTN) includes cancers like invasive moles, choriocarcinomas, and others. Invasive moles can grow and spread more than hydatidiform moles. Choriocarcinomas can spread to different parts of the body, especially in women with a history of molar pregnancies or miscarriages.
PSTT and ETT are rarer types of GTN. Age and having had a molar pregnancy before are risk factors for GTD.
Knowing about the different types of gestational trophoblastic disease is key. It helps in diagnosing, treating, and managing this rare condition. Healthcare providers can then give the best care by understanding the risks and complications of HMs and GTN.
Causes and Risk Factors
Though we don’t know all about GTD, we know some things that raise the risk. These include certain factors that can make a woman more likely to get this rare condition.
Maternal Age
Being very young or very old can increase the risk of GTD. Women under 20 or over 40 face a higher risk. This might be because of changes in the body during early or late pregnancy.
Previous Molar Pregnancy
Having had a molar pregnancy before raises the risk of getting it again. Women who’ve had a mole before might have a 20% chance of getting another one. This shows why it’s crucial to watch closely if you’ve had a molar pregnancy before.
Miscarriage History
Women who have had miscarriages might also be at higher risk for GTD. The exact link isn’t clear, but changes in hormones and cells from early pregnancy loss might play a part.
Risk Factor | Explanation |
|---|---|
Maternal Age | Women under 20 and over 40 have a higher risk of developing GTD. |
Previous Molar Pregnancy | Women with a history of molar pregnancy have up to a 20% chance of developing another mole in a subsequent pregnancy. |
Miscarriage History | Women with a history of miscarriage may have an increased risk of GTD, though the relationship is not fully understood. |
Knowing these risk factors helps doctors keep a close eye on women at higher risk. This way, they can catch GTD early and treat it quickly if needed.
Gestational Trophoblastic Disease Symptoms
Women with gestational trophoblastic disease (GTD) may feel many symptoms. These symptoms can change based on the type of GTD. Some common symptoms include:
- Abnormal vaginal bleeding
- A larger-than-usual uterus during pregnancy
- Pelvic pain or mass
- Severe nausea and vomiting
- High blood pressure, headache, and swelling
- Shortness of breath, dizziness, fast and irregular heartbeat, and signs of thyroid irregularities
Hydatidiform moles are the most common type of GTD. They are found in the uterus and do not spread. On the other hand, Gestational Trophoblastic Neoplasia (GTN) is cancerous and can spread to other parts of the body. GTN can spread, and its staging includes Stage I (limited within the uterus), Stage II (spread to the ovary, fallopian tube, and vagina), Stage III (spread to the lung), and Stage IV (spread beyond the lungs to other areas).

To accurately diagnose GTD, a complete physical exam and pelvic exam are needed. An ultrasound exam of the pelvis, blood tests checking for levels of b-hCG, urine studies, and curetting of the inside of the uterus are also required.
Key GTD Symptoms | Prevalence |
|---|---|
Abnormal vaginal bleeding | Common in 1 out of 1000 pregnancies |
Larger-than-usual uterus | Frequent during pregnancy |
Pelvic pain or mass | Commonly reported |
Severe nausea and vomiting | Significant in many cases |
“Accurate diagnosis of GTD is crucial for effective treatment and management of this rare but serious condition.”
Diagnosis of Gestational Trophoblastic Disease
Diagnosing gestational trophoblastic disease (GTD) starts with a detailed medical check. This includes looking at your medical history, a physical exam, and several tests. This method helps doctors find out what kind of disease you have and how far it has spread. They can then plan the best treatment for you.
Medical History and Physical Exam
Your doctor will first ask about your past health, pregnancies, and symptoms. Then, they will do a physical exam. This might include a pelvic exam to check your uterus, ovaries, and other organs.
Diagnostic Tests
To confirm GTD, your doctor may use several tests:
- Pap Test: A Pap test looks for abnormal cells in the cervix that could be linked to GTD.
- Transvaginal Ultrasound: An ultrasound gives clear images of the uterus. It helps spot molar pregnancies or other GTD issues.
- Blood Tests: Blood tests, especially those for human chorionic gonadotropin (hCG), help diagnose and track GTD.
- Urinalysis: A urinalysis checks for hCG in your urine, which can indicate GTD.
At times, doctors might also use chest X-rays, CT scans, or MRIs. These help see if GTD has spread to other areas.
Doctors use your medical history, physical exam, and test results to accurately diagnose GTD. This lets them plan the right treatment for you.
Treatment Options
If you have been diagnosed with gestational trophoblastic disease (GTD), your treatment plan will depend on the specific type and stage of your condition. Treatment methods may include surgery, chemotherapy, hysterectomy, and radiation therapy.
Surgery
For hydatidiform moles, which are the most common type of GTD, surgery is often the primary treatment. This may involve a dilation and curettage (D&C) procedure to remove the molar tissue from the uterus. In some cases, a hysterectomy (removal of the uterus) may be recommended, especially if the patient does not plan to have any more children.
Chemotherapy
Chemotherapy is the main treatment for gestational trophoblastic neoplasia (GTN), which includes invasive moles and choriocarcinoma. Common chemotherapy drugs used to treat GTN include methotrexate, dactinomycin, etoposide, vincristine, cisplatin, and bleomycin. These drugs can be used alone or in combination, depending on the specific case.
Chemotherapy is a systemic treatment that travels through the bloodstream to destroy cancer cells throughout the body, including those that may have spread from the primary uterine tumor. Even in advanced cases, most GTDs can be cured with chemotherapy.
Hysterectomy and Radiation Therapy
In some high-risk cases of GTN, a hysterectomy may be performed for women who do not wish to have more children. Radiation therapy may also be used, particularly to treat GTD that has spread to the brain or other areas of the body and is unresponsive to chemotherapy.
The treatment for recurrent or resistant GTD may involve a combination of approaches, such as altering chemotherapy drug regimens, undergoing additional surgery, and potentially using radiation therapy.
Regular follow-up and monitoring are essential after treatment for GTD to ensure that the condition does not return. Your healthcare team will work with you to develop the most appropriate treatment plan based on your specific case.
Gestational Trophoblastic Disease and Future Pregnancies
Most women treated for gestational trophoblastic disease (GTD) can have healthy pregnancies later. But, it’s key to know how GTD and its treatments might affect fertility and future pregnancies.
Chemotherapy for GTD might make women start menopause 3 years early. Women over 45 might not get their periods back after treatment. The chance of another molar pregnancy is low, about 1%.
Doctors often suggest using birth control after GTD treatment. This includes pills, patches, implants, and more. It helps prevent more molar pregnancies and ensures a safe pregnancy later.
Fertility and Pregnancy Outcomes
GTD and its treatments can affect fertility and future pregnancies differently. Some moles can turn into cancer, which can be caught with tests. Women who get pregnant soon after chemotherapy face a higher risk of miscarriage.
Chemotherapy can make menopause come sooner, but it might not always stop fertility in young women. High-dose chemotherapy can cause permanent infertility.
Immunotherapy might offer better results than some chemotherapy for GTD. Women with high-risk GTD can still have successful pregnancies and fertility, especially with low-risk cases.
The placental site and epithelioid trophoblastic tumors are different and might not respond as well to chemotherapy.
Women with GTD history might worry about future pregnancies. They might fear relapse and have emotional challenges. It’s vital to have accurate data for counseling them.
“Most women treated for GTD can go on to have normal, healthy pregnancies in the future, but it’s important to understand the potential implications and work closely with healthcare providers to ensure the best possible outcomes.”
Prevention Strategies
There’s no known way to completely stop GTD. The only sure way is to not get pregnant.
Most women can have healthy babies after GTD treatment. But, it’s key to follow doctor’s advice. They say wait at least 6 months or more after a hydatidiform mole. And wait at least 1 year after gestational trophoblastic neoplasia.
Also, get an ultrasound early in pregnancy. Do it at 6 and 10 weeks to check for GTD signs. Getting pregnant too soon after GTD treatment can risk miscarriage or birth defects.
Remember, the only sure way to prevent GTD is to avoid becoming pregnant. If you have a history of GTD, it’s crucial to follow your healthcare provider’s recommendations carefully to ensure a healthy future pregnancy.
Gestational Trophoblastic Disease Prognosis
The outlook for gestational trophoblastic disease (GTD) is very good, especially if caught and treated early. Invasive mole and choriocarcinoma, two aggressive forms, have a survival rate close to 100%. This success is thanks to modern treatments, especially chemotherapy, which works well for most women.
People with GTD are put into different risk groups based on how serious their case is. Those in the low-risk group have a 100% success rate with treatment. Even those in the high-risk group can be cured with the right care. Though ultra high-risk cases are tougher, the overall outlook for GTD is still very good, especially if caught early.
The good results for GTD come from a lot of research and special care at dedicated centers. Studies have followed patients for 1 to 16 years after diagnosis. These studies show GTD can be cured, with findings in respected journals like the British Journal of Cancer.
Treatable and Curable, but Caution for Advanced Cases
While GTD’s overall outlook is bright, advanced cases are more challenging. Rare and aggressive types like choriocarcinoma need quick and special treatment for the best results. It’s key for patients and doctors to catch it early and act fast for the best chance of survival.
In short, GTD’s outlook is mostly excellent, with most cases being treatable and curable, especially if caught early. But, more serious or unusual cases need careful watching and special care for the best results.
Conclusion
Gestational trophoblastic disease (GTD) is a rare condition that happens during pregnancy. It comes from abnormal growth of trophoblast cells. GTD can be either benign or malignant, with hydatidiform moles being the most common.
About 50% of gestational trophoblastic neoplasia (GTN) cases start after a molar pregnancy. Also, 25% may come after miscarriage, termination, or ectopic. GTN after a complete molar pregnancy can lead to 15% of patients having persistent local disease and 5% may develop metastatic disease.
The risk of GTN is low, but it increases after a molar pregnancy. The risk goes up to 1-2% after one molar pregnancy. It jumps to 15-20% after two molar gestations. Also, the risk of GTN in a coexisting molar and normal pregnancy is 27-46%. For singleton molar pregnancies, the risk is 15-20%.
Early diagnosis and treatment are key. Most GTD cases, especially when caught early, can be treated and cured.
Understanding GTD is vital for healthcare providers and patients. By knowing about GTD, its causes, symptoms, diagnosis, and treatment, we can manage it better. This knowledge helps in taking proactive steps for reproductive health. Ongoing research and advancements offer hope for better outcomes and quality of life for those with GTD.
FAQ
What is gestational trophoblastic disease (GTD)?
GTD is a rare group of tumors that happen early in pregnancy. They come from abnormal growth of trophoblast cells. These cells usually make up the placenta but grow wrong in GTD. They can be either non-cancerous or cancerous.
What are the main types of gestational trophoblastic disease?
GTD has two main types. The first is hydatidiform moles, or molar pregnancies. The second is gestational trophoblastic neoplasia (GTN). GTN includes serious forms like choriocarcinoma and invasive moles.
What are the risk factors for gestational trophoblastic disease?
Risk factors for GTD include being older, having had a molar pregnancy before, and having a history of miscarriage.
What are the common symptoms of gestational trophoblastic disease?
Symptoms of GTD include abnormal bleeding, a big uterus, pelvic pain, and severe nausea and vomiting.
How is gestational trophoblastic disease diagnosed?
Diagnosing GTD involves a detailed medical check-up. This includes looking at your medical history, a physical exam, and tests like ultrasound and blood tests.
What are the treatment options for gestational trophoblastic disease?
Treatment for GTD depends on the type and stage of the disease. It also depends on your health and if you want to have more kids. Options include surgery, chemotherapy, and radiation therapy.
Can women with gestational trophoblastic disease have healthy pregnancies in the future?
Yes, most women treated for GTD can have healthy pregnancies later. This is a very positive thing about GTD.
Can gestational trophoblastic disease be prevented?
No, there’s no way to prevent GTD. The only way to avoid it is to not get pregnant.
What is the prognosis for gestational trophoblastic disease?
The outlook for GTD is good, especially if caught early. Most GTD cases, like hydatidiform moles, are treatable and curable.