FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Dementia with Lewy Bodies (DLB) is a complex and often misdiagnosed condition that shares symptoms with both Alzheimer’s disease and Parkinson’s disease.
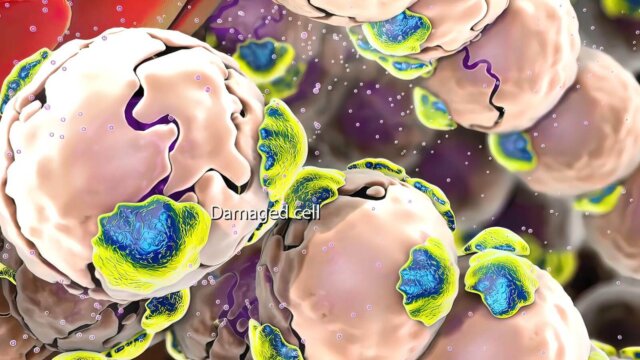
It is characterized by the presence of Lewy bodies—abnormal protein deposits in the brain that affect cognition, movement, and behavior.
Despite its significant impact, DLB is less well-known than Alzheimer’s, yet it is not uncommon. In the United States, DLB accounts for up to 10% of all dementia cases, making it essential for medical professionals and caregivers to have a clear understanding of the disorder.
This article aims to illuminate the nuances of DLB, particularly in comparison to Alzheimer’s disease. Recognizing its distinctive features is crucial for accurate diagnosis, which can inform more effective management and treatment strategies.
By delineating the differences between these two forms of dementia, we hope to provide a comprehensive guide that will support enhanced patient care and awareness of potential treatment options.
For further information on DLB, the Alzheimer’s Association provides valuable resources, while the Mayo Clinic offers insights into symptoms and causes.
Understanding Dementia with Lewy Bodies (DLB)
Dementia with Lewy Bodies (DLB) is a type of progressive dementia distinguished by the presence of abnormal protein deposits known as Lewy bodies in the brain.
These are named after the neurologist who discovered them, Frederich H. Lewy. Characterized by fluctuations in attention, visual hallucinations, sleep disturbances, and parkinsonism, DLB poses challenges distinct from other dementias.
Unlike Alzheimer’s disease, where memory loss is prominent, DLB significantly impacts cognitive functions like judgment and visual perception early on.
Comparatively, motor symptoms such as rigidity and tremors manifest earlier in DLB, leading to disability sooner than in Alzheimer’s.
Moreover, DLB patients often experience severe autonomic nervous system disruptions, a contrast to Alzheimer’s progression.
The overlap of symptoms in DLB and Parkinson’s disease dementia suggests a close relationship, yet the former presents cognitive decline within a year of movement issues, whereas the latter shows cognitive impairment much later.
Symptoms and Causes of DLB
Dementia with Lewy Bodies (DLB) presents a constellation of symptoms that can perplex both patients and healthcare providers.
Cognitive changes are prominent, with individuals experiencing attention difficulties, planning challenges, and problems with visual and spatial abilities.
As DLB progresses, behavioral changes such as depression, apathy, and anxiety become more pronounced, often exacerbated by visual hallucinations that can occur in up to 80% of cases.
Motor symptoms reminiscent of Parkinson’s disease, including tremors and muscle stiffness, are also common, contributing to the complexity of the condition.
Sleep disturbances, particularly REM sleep behavior disorder, can lead to individuals acting out their dreams, potentially causing injury. Additionally, DLB can significantly impact the autonomic nervous system, leading to blood pressure fluctuations, dizziness, and fainting.
While the exact causes of DLB remain under investigation, risk factors include age and certain genetic variants, though these do not guarantee disease development.
Ongoing research aims to unravel the disease’s pathophysiology and potential interventions. The importance of early detection and accurate diagnosis cannot be overstated, as it is critical for effective management and care planning for DLB.
Diagnosing DLB
Diagnosing Dementia with Lewy Bodies (DLB) is complex. It begins with a detailed patient and caregiver interview focusing on cognitive, movement, sleep, behavioral, and mood symptoms. Imaging tests, such as MRI or CT scans, and cognitive assessments may be employed to differentiate DLB from other dementias.
However, the early symptoms of DLB often overlap with those of Alzheimer’s disease or psychiatric illnesses, posing challenges in accurate diagnosis.
Due to the risk of adverse reactions to certain medications in DLB patients, the involvement of specialists like geriatric psychiatrists or neurologists is crucial. These professionals utilize their expertise to interpret clinical symptoms and biomarkers, aiding in earlier and more precise diagnoses.
It’s also important to recognize the connection between DLB, Parkinson’s disease Dementia, and Alzheimer’s. The “one-year rule” helps distinguish DLB from Parkinson’s disease dementia based on the timeline of cognitive symptoms in relation to movement issues.
Understanding these nuances is vital for tailoring treatment and planning for future care needs. For more detailed information, the NIA ADEAR Center provides resources to support and educate patients and families following a DLB diagnosis.
Treatment Options for DLB
Treatment for Dementia with Lewy Bodies (DLB) is multifaceted, involving a team of specialists to manage its complex symptoms. Medications such as cholinesterase inhibitors and memantine may improve cognitive issues and hallucinations, while carbidopa/levodopa is used for movement symptoms.
Non-pharmacological interventions include physical, speech, and occupational therapies, as well as lifestyle changes and psychotherapy.
Caregivers play a crucial role in the treatment plan. They provide physical support and ensure the safety of those with DLB. They also offer emotional support, which is essential for managing the psychological aspects of the disease.
- Medications can offer symptomatic relief but do not halt disease progression.
- Non-pharmacological approaches aim to maintain quality of life and independence.
- Caregiver support is vital for managing daily challenges and providing patient care.
While these treatments can be beneficial, they come with limitations. Some medications may exacerbate other DLB symptoms or have side effects, and there is currently no cure for DLB.
For managing DLB symptoms effectively, a comprehensive approach tailored to individual needs, developed in collaboration with healthcare professionals, is recommended.
Differentiating DLB from Alzheimer’s Disease
Distinguishing between Dementia with Lewy Bodies (DLB) and Alzheimer’s disease is crucial for tailoring appropriate treatment strategies. While both conditions share the umbrella of dementia, their pathologies and symptom presentations diverge in significant ways.
A comparison table serves as a valuable tool for healthcare professionals to pinpoint the specific characteristics of each disorder.
- DLB: Often presents with early symptoms such as visual hallucinations, fluctuating attention, Parkinsonian movement issues, and REM sleep behavior disorder.
- Alzheimer’s: Typically manifests through progressive memory loss, language difficulties, and spatial awareness challenges.
Given the potential overlap in symptoms like memory impairment and mood changes, accurate diagnosis is imperative.
The presence of Lewy bodies and Alzheimer’s markers, such as plaques and tangles, can coexist, making the clinical picture complex.
Cognitive tests, imaging, and symptom assessment are essential to distinguish DLB from Alzheimer’s, ensuring that patients receive the most effective management for their specific type of dementia.
The Impact of DLB on Patients and Caregivers
Dementia with Lewy Bodies (DLB) presents a multifaceted challenge, deeply affecting both those diagnosed and their caregivers. Patients grapple with neuropsychiatric symptoms like hallucinations and sleep disturbances, which can be as disorienting as they are distressing.
The emotional toll is mirrored in the physical realm, where simple tasks become herculean efforts due to impaired motor functions. Caregivers, in turn, face a relentless wave of demands, leading to significant emotional, physical, and financial strain.
The burden can be so profound that it often results in caregiver burnout, a state of physical, emotional, and mental exhaustion.
Recognizing the need for a sturdy support network, resources such as the Lewy Body Dementia Association and the National Institute on Aging offer a lifeline.
These organizations provide vital information, fostering communities where experiences and coping strategies can be shared.
Caregiver support is not a luxury but a necessity, underpinning the ability to manage the complexities of care for someone with DLB. Self-care becomes a critical component for caregivers to sustain their own well-being and, by extension, the quality of care they provide.
Conclusion
In the quest to unravel the mysteries of dementia, we’ve explored the peculiarities of Dementia with Lewy Bodies (DLB) as it stands in contrast to Alzheimer’s disease. Key characteristics of DLB, such as cognitive fluctuations, visual hallucinations, and Parkinsonian features, mark its unique clinical footprint.
This condition challenges the cognitive faculties of patients and casts a heavy burden on caregivers, necessitating a mosaic of support and understanding.
Early detection and astute management are pivotal in mitigating the progression of DLB and improving quality of life.
The emphasis on avoiding antipsychotics, unless absolutely necessary, and the potential benefits of cholinesterase inhibitors and N-methyl-D-aspartate antagonists are notable considerations in treatment.
As we conclude, it’s critical to advocate for a deeper comprehension of DLB and to champion the advancement of research in this field.
For those who may recognize symptoms of DLB in themselves or their loved ones, seeking medical evaluation is crucial. Together, through awareness and science, we can navigate the complexities of DLB with greater precision and empathy.