FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Over half a million Americans live with Crohn’s disease. This chronic illness makes the immune system attack healthy cells in the gut. It leads to pain and many tough symptoms. Even though there’s no cure, treatments can help manage the disease.
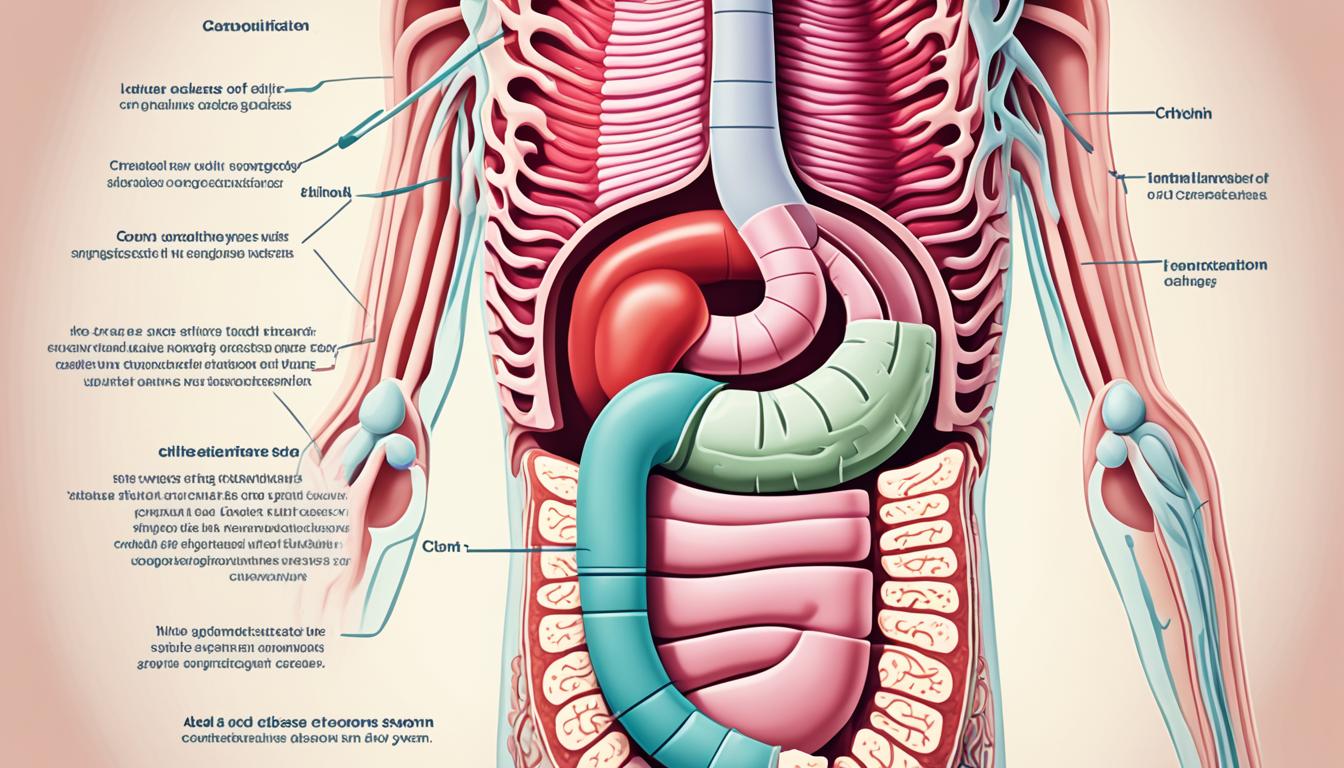
Crohn’s disease is part of inflammatory bowel disease (IBD). It can hit any part of the digestive system, but often affects the small intestine and colon. The exact cause is still a mystery, but it seems to be linked to genes, the environment, and the immune system.
Key Takeaways
- Crohn’s disease is a chronic, inflammatory bowel disease that affects the digestive tract.
- Symptoms can include abdominal pain, diarrhea, fatigue, weight loss, and malnutrition.
- There is no cure, but treatments can help manage symptoms and reduce inflammation.
- Risk factors include genetics, immune system dysfunction, and environmental factors like smoking.
- Diagnosis involves tests like blood work, endoscopies, and imaging scans.
What is Crohn’s Disease?
Crohn’s disease is a type of inflammatory bowel disease (IBD). It makes the digestive tract swell and get irritated. IBDs are long-term conditions that cause inflammation in the digestive tract. Crohn’s disease can hit any part of the digestive system, from mouth to anus, but often hits the large and small intestines. It can also spread deeper into the bowel layers.
Understanding Inflammatory Bowel Diseases
Inflammatory bowel diseases (IBDs) are chronic conditions that cause inflammation and irritation in the digestive tract. There are two main types: Crohn’s disease and ulcerative colitis. They are similar but different in where they affect and how they progress.
Where Crohn’s Disease Can Affect the Digestive System
Crohn’s disease can affect any part of the digestive tract, from mouth to anus. But it often hits the end of the small intestine and the start of the colon. This inflammation can go deep into the bowel wall. It can cause scarring, blockages, and fistulas (wrong connections between intestines and other organs).
Crohn’s disease is a chronic condition that causes a lot of discomfort and health problems. It’s important to understand this disease and its effects on the digestive system for good management and treatment.
Crohn’s Disease Symptoms
Crohn’s disease is a chronic condition that can cause many symptoms. These symptoms can be different for each person. Common symptoms include diarrhea, rectal bleeding, and feeling the need to have a bowel movement urgently.
Other symptoms are abdominal cramps, feeling like you haven’t fully emptied your bowels, and constipation that can lead to a bowel blockage.
Common Crohn’s Disease Symptoms
Symptoms of Crohn’s disease can vary and include diarrhea, fever, and feeling very tired. You might also have abdominal pain, see blood in your stool, have mouth sores, eat less, and lose weight.
These symptoms can also cause inflammation in different parts of the body. This includes the eyes, skin, joints, liver, or bile ducts, and can even cause kidney stones and anemia. In children, it can also slow down growth and development.
Severe Crohn’s Disease Symptoms
In severe cases, Crohn’s disease can cause more serious problems. These include fissures, fistulizing Crohn’s disease, and strictures in the intestine. These problems can make you lose your appetite, lose weight, feel very tired, and have less energy.
Crohn’s disease can also affect other parts of your body. This can lead to red eyes, mouth sores, swollen and painful joints, skin problems, fever, night sweats, and issues with your menstrual cycle. It can also cause osteoporosis, kidney stones, and liver problems like primary sclerosing cholangitis and cirrhosis.
Common Crohn’s Disease Symptoms | Severe Crohn’s Disease Symptoms |
|---|---|
|
|
The severity and types of symptoms can vary a lot from one person to another. It’s important to see a doctor and work with them to manage the disease.
Who Gets Crohn’s Disease?
Crohn’s disease can happen to anyone, but it often starts in teens and young adults. In the U.S., over 3 million people have it, with many getting symptoms before they turn 15. There might be more cases around age 60 too.
Some groups are more likely to get Crohn’s disease. Whites, especially Ashkenazi Jews, face the biggest risk. But, Black people in North America and the UK are seeing more cases too. If someone in your family has it, you’re more likely to get it, since genes play a big part.
What you do can affect your risk of getting Crohn’s disease. Smoking makes it more likely. But eating lots of fruits, veggies, and less red meat might help lower your risk.
In short, Crohn’s disease can hit anyone, but it’s most common in young people. Whites, Ashkenazi Jews, and those with family history are at higher risk. What you do, like smoking and eating, can also affect your chances of getting it.
Causes of Crohn’s Disease
The exact causes of Crohn’s disease are not fully known. But, it seems that both genes and environment can play a part. Immune system issues and genetic factors are key in starting and making the disease worse.
Immune System Dysfunction
Crohn’s disease might happen when the immune system attacks the digestive tract. This leads to inflammation. This immune system problem is a main cause of the disease. It causes ongoing inflammation and damage to the tissues.
Genetics and Family History
Genetics could be linked to Crohn’s disease, as about 20% of those with it have a family member with it. Some genes affect how the body handles certain microbes, making Crohn’s more likely. Also, some groups, like Jewish people, get Crohn’s more often than others.
Researchers are still looking into the genes that make someone more likely to get Crohn’s. They think things like diet and lifestyle might trigger the disease in those at risk.

Crohn’s disease is complex, with many factors at play. We don’t fully understand how genes, environment, and the immune system interact. Research is ongoing to learn more about this chronic illness.
Risk Factors for Developing Crohn’s Disease
Crohn’s disease is a complex condition with many risk factors. These factors can make someone more likely to get this chronic bowel disease. Researchers have found several key factors that might increase a person’s chance of getting it.
Age as a Risk Factor
Crohn’s disease can start at any age, but most people get it before they are 30, or between 40 and 60. It often hits during important life stages, affecting quality of life and wellbeing.
Ethnicity and Race
Some ethnic and racial groups face a higher risk of getting Crohn’s disease. People from Northern Europe, Anglo-Saxon, or Ashkenazi Jewish backgrounds are more at risk. Ashkenazi Jewish people are two to four times more likely to get an inflammatory bowel disease. But, it’s less common in people from central and southern Europe, South America, Asia, and Africa.
The risk of getting Crohn’s disease is rising among Black people in North America and the UK. Black and Hispanic people with the disease might not get surgery as often and may visit the ER more than white people. This shows we need better healthcare and special help for these groups.
Smoking and NSAIDs
Smoking is a big risk factor for Crohn’s disease, making it worse and possibly needing surgery. Non-steroidal anti-inflammatory drugs (NSAIDs) don’t cause the disease but can make symptoms worse.
Other things can increase the risk of Crohn’s or make symptoms worse. These include having had your appendix removed, certain diets, mental health issues, and being less active. Changing these things and getting medical help can help manage and prevent Crohn’s disease.
In summary, Crohn’s disease can happen at any age, but mostly in young adults. Some groups, like those of Northern European, Anglo-Saxon, or Ashkenazi Jewish descent, face a higher risk. Smoking and NSAIDs can also make the disease worse.
Diagnosing Crohn’s Disease
Diagnosing Crohn’s disease is a detailed process. It uses blood tests, stool tests, and imaging to see the digestive tract. These methods help find any issues.
Blood Tests for Crohn’s Disease
Blood tests help spot Crohn’s disease by looking for anemia and infection signs. They also rule out other health problems.
Stool Tests for Crohn’s Disease
Stool tests aid in diagnosing Crohn’s disease. They check for blood in stool or certain pathogens causing digestive issues.
Imaging Tests for Crohn’s Disease
Imaging tests are key in diagnosing Crohn’s disease. Tests like colonoscopy and CT scans show the digestive tract. They help confirm the disease and its severity.
Imaging Test | Description |
|---|---|
Colonoscopy | Views the colon and terminal ileum, includes biopsies, and shows signs of Crohn’s disease. |
CT Enterography | Shows the small bowel in detail, often used instead of barium X-rays. |
MRI | Helps see fistulas in the anal area or small intestine, good for young patients because it uses less radiation. |
Capsule Endoscopy | Uses a camera capsule swallowed to see the digestive tract and diagnose Crohn’s without anesthesia. |
Upper GI Series | Makes x-rays with barium to view the upper GI tract and spot Crohn’s disease. |
CT Scan | Makes images of the digestive tract with x-rays and contrast, aiding in Crohn’s diagnosis and its complications. |
Healthcare providers use these tests to make a full diagnosis of Crohn’s disease. They then create a treatment plan.

Treatment Options for Crohn’s Disease
Crohn’s disease is a complex condition that needs a detailed treatment plan. The main goals are to lessen inflammation, control symptoms, and stop complications. Since every case is different, there’s no single treatment for Crohn’s disease. Medications are key in managing the disease, aiming to calm down the immune system’s overactive response and help heal the gut.
Anti-Inflammatory Medications
Anti-inflammatory drugs like corticosteroids and 5-aminosalicylates are often the first choice to fight inflammation in Crohn’s disease. These drugs help ease symptoms and help heal the gut. But, using corticosteroids for a long time can cause problems like acne, bone loss, high blood sugar, and gaining weight.
Immune System Suppressors
Drugs that calm down the immune system, such as azathioprine, mercaptopurine, and methotrexate, can lessen inflammation in Crohn’s disease. They work by slowing down the immune system’s overactive response that causes inflammation. These drugs can have side effects like low white blood cell count, feeling tired, and pancreatitis.
Biologic Therapies
Newer biologic drugs target specific immune proteins, like vedolizumab, infliximab, adalimumab, certolizumab pegol, ustekinumab, and risankizumab, to treat Crohn’s disease. These biologics, or anti-tumor necrosis factor-alpha therapies, can reduce inflammation and help heal the gut. But, they might raise the chance of getting infections, including tuberculosis.
Using a mix of medications can make treatment work better but might increase the risk of side effects. Clinical trials are important for finding new and better treatments for Crohn’s disease as treatment options evolve.
Managing diet and nutrition is also crucial in treating Crohn’s disease by easing symptoms, providing important nutrients, and helping with healing. Even with the right medication and diet, many Crohn’s patients may need surgery at some point.
The best treatment plan for someone with Crohn’s depends on how severe their condition is, how they react to treatments, and if they have any complications.
Surgical Treatment for Crohn’s Disease
For people with Crohn’s disease, surgery might be part of their treatment plan. Up to three-quarters of those with the disease will need surgery at some point. This is to deal with complications and issues from the chronic, inflammatory bowel condition.
Common surgeries for Crohn’s include strictureplasty, fistula removal, and more. These operations can help with symptoms and improve life quality. But, surgery doesn’t cure Crohn’s disease. About 30% of those who have surgery may see symptoms return within 3 years, and 60% within 10 years.
Surgery can lead to infections and other issues, but it also has benefits. These benefits include less pain, fewer symptoms, and better diet. After surgery, patients might need new medicines and could stay in the hospital for a week.
It’s wise for those with Crohn’s to see surgeons who specialize in general or colon and rectal surgery. Surgery might be an option if medical treatments don’t help much or if medicines cause bad side effects.
Surgery doesn’t cure Crohn’s, but it helps manage the condition and improve health. Regular colonoscopies are also advised to check for colorectal cancer risk.

Surgical Procedure | Description |
|---|---|
Strictureplasty | Widening of a narrowed section of the intestine to improve the flow of digested food |
Fistula Removal | Removal of abnormal connections between the intestines and other organs or the skin |
Colectomy | Partial or complete removal of the colon |
Proctocolectomy | Removal of the entire colon and rectum |
End Ileostomy | Creation of an opening in the abdomen to allow waste to exit the body |
Bowel Resection | Removal of a damaged or diseased portion of the intestine |
Abscess Drainage | Drainage of a localized collection of pus in the abdomen or pelvis |
Ileostomy | Creation of an opening in the abdomen to allow waste to exit the body |
“Surgery for Crohn’s disease does not guarantee the absence of future symptoms, but it can provide significant benefits in terms of reduced pain, fewer symptoms, fewer medications, improved diet, and weight gain.”
Nutrition Therapy for Crohn’s Disease
Eating differently can help improve nutrition and let the bowel rest. This can lessen inflammation. A low-residue or low-fiber diet may be suggested to avoid intestinal blockage. It’s key for people with Crohn’s disease to eat right because they might not absorb nutrients well.
When Crohn’s disease gets worse, eating less fiber can help. This means avoiding foods like fresh fruits, veggies, prunes, and caffeinated drinks. Eating smaller meals more often can also be easier and help you get more nutrients.
After things get better, eating a variety of foods is good. This includes fruits, veggies, whole grains, lean meats, and low-fat dairy. Adding foods high in fiber can also help your gut health.
Some medicines for Crohn’s disease can make it hard for your body to absorb nutrients. This includes things like prednisone and cholestyramine. It’s important to watch for and fix these issues with diet or supplements to stay healthy.
Also, think about how surgery for Crohn’s disease affects nutrient absorption. Less surface area in the intestines can make it harder to get vitamins and minerals.
Getting a diet plan that fits your needs and the stage of your disease is key. This helps manage Crohn’s disease and keeps you feeling good.
Working with a healthcare team, including a dietitian, can help. They can make a plan that meets your nutritional needs and supports your health over time.
Lifestyle and Home Remedies for Crohn’s Disease
Managing stress, exercising, and avoiding trigger foods can help with Crohn’s disease symptoms. Keeping a food diary can spot what foods trigger your symptoms.
Probiotics can fix the balance of gut bacteria in people with Crohn’s. Omega-3 fatty acids from fish or supplements might help with inflammation, but their effect on Crohn’s is still unsure.
A liquid diet can help heal the gut during a flare-up, lasting from days to weeks with a doctor’s advice. Traditional Chinese medicine like acupuncture might also help, but more studies are needed.
Yoga is good for reducing stress, which can help prevent Crohn’s flare-ups. But, getting too little sunlight can increase Crohn’s risk, so sunbathing is not advised.
Turmeric’s curcumin might fight inflammation in Crohn’s, but more research is needed. Early studies suggest cannabis could ease symptoms like pain and nausea, but more research is needed.
Pineapple stem’s bromelain could fight Crohn’s inflammation. Camel milk is full of nutrients and antioxidants, and might improve Crohn’s symptoms by providing essential vitamins and minerals.
Biofeedback therapy lets people control their body’s reactions with their thoughts, helping with stress and symptoms of Crohn’s.
A 2022 review found curcumin could be a safe and effective treatment for IBD. Probiotics have strong evidence of helping ulcerative colitis and might help Crohn’s disease too, according to a 2023 review.
Bromelain showed promise in reducing inflammation in rat studies in 2017, but more human research is needed. Wormwood might help people with Crohn’s get into remission, but more studies are needed.
Thunder god vine might help with chronic inflammation, but its effect on Crohn’s is still unknown, says the National Center for Complementary and Integrative Health. Patchouli oil could reduce colitis symptoms in rats, suggesting it might help with inflammatory bowel conditions.
Fish oil, including cod liver oil and omega-3 supplements, might ease Crohn’s symptoms, says the Crohn’s & Colitis Foundation and a 2022 study. Medical cannabis could improve IBD symptoms and quality of life, especially for those who used it before, a 2022 study found.
Acupuncture with moxibustion helped people with Crohn’s disease, a 2023 review found, but more research is needed to understand how it works.
Many people with Crohn’s use traditional medicine and natural treatments together. Probiotics are in foods like yogurt and sauerkraut, while prebiotics are in artichokes and bananas.
Omega-3 fatty acids in fish oil can reduce Crohn’s symptoms, making it more likely to stay in remission. Acupuncture can release endorphins, helping manage Crohn’s symptoms.
Biofeedback therapy helps manage bodily responses, including those with Crohn’s disease. Herbal treatments like aloe vera juice and turmeric might ease symptoms, but talk to a doctor first because they can interact with other medicines.
Living with Crohn’s Disease
Crohn’s disease is a chronic condition with ups and downs. It’s important to manage symptoms and keep a good quality of life. Knowing how to handle flare-ups is key for those with the disease.
Managing Crohn’s Disease Flare-Ups
Flare-ups of Crohn’s disease can be tough, causing diarrhea, pain, weight loss, and tiredness. It’s vital to work with doctors to find and fix the causes, like food or stress. A tailored treatment plan, anti-inflammatory drugs, and lifestyle changes can help lessen flare-ups.
Emotional Impact of Crohn’s Disease
Crohn’s disease can really affect your feelings, leading to anxiety, frustration, and sadness. The constant ups and downs, along with physical issues, can hurt your mental health. Talking to a therapist or joining a support group can help. Sharing stories and tips with others who get it can make you feel supported and help you cope better.
Support Groups and Resources
Being part of a support group can make you feel connected and not alone. There are many online and in-person groups, resources, and networks for Crohn’s disease patients. Crohn’s & Colitis Foundation, NHS, and WebMD offer lots of helpful info and support.
“Living with Crohn’s disease requires patience, resilience, and a willingness to adapt. But with the right support and management strategies, individuals can find ways to thrive and maintain a fulfilling life.” – Dr. Sarah Almond, Gastroenterologist
Understanding how to manage flare-ups, dealing with the emotional side, and using support can help people with Crohn’s disease take charge of their health and live better.
Conclusion
There is no cure for Crohn’s disease, but treatments can ease symptoms and improve life quality. In the U.S., 319 people per 100,000 have Crohn’s disease. Each year, 20.2 new cases are found per 100,000 people. With the right care, diet, and support, people with Crohn’s can manage their condition well.
Research has found that immune system issues and genetics play a big part in Crohn’s disease. This has led to new treatments that help control the disease and prevent serious problems.
About half of Crohn’s patients face bowel problems within 20 years of being diagnosed. But, surgery rates have dropped by 8.4% each year from 1996 to 2013.
Working with doctors, eating well, staying active, and getting support helps manage Crohn’s disease. This approach can improve health and well-being. Thanks to ongoing research, the outlook for people with Crohn’s disease is getting better.
FAQ
What is Crohn’s disease?
Crohn’s disease is a condition that causes ongoing inflammation in the gut. It can affect any part of the digestive system, from the mouth to the anus. It’s a long-term illness that can be very painful and stressful, sometimes leading to serious problems.
What are the symptoms of Crohn’s disease?
Symptoms can vary but often include diarrhea, fever, and feeling very tired. You might also have belly pain, see blood in your stool, have mouth sores, eat less, and lose weight. In severe cases, it can affect other parts of the body like the eyes, skin, and liver.
What causes Crohn’s disease?
We don’t fully understand what causes Crohn’s disease. But it’s thought to be a mix of an overactive immune system and genetics. Sometimes, the immune system attacks the gut, causing inflammation. If your family has it, you might be more likely to get it too.
Who is at risk of developing Crohn’s disease?
Most people get diagnosed with Crohn’s before they turn 30. It’s more common in whites, especially those of Ashkenazi Jewish descent. But, it’s becoming more common in Black people in North America and the UK. Smoking and using certain painkillers can also raise your risk.
How is Crohn’s disease diagnosed?
Doctors use blood tests, stool tests, and imaging like colonoscopies to diagnose Crohn’s. These tests help find inflammation, rule out other conditions, and confirm the diagnosis.
What are the treatment options for Crohn’s disease?
Treatment often includes anti-inflammatory and immune system drugs. These can reduce inflammation and help manage symptoms. Newer treatments target specific immune proteins and can be very effective.
When is surgery required for Crohn’s disease?
Surgery is needed by about half of those with Crohn’s to remove damaged gut parts. But it doesn’t cure the disease, and it often comes back.
How can diet and lifestyle affect Crohn’s disease?
Eating differently can help manage symptoms and reduce inflammation. A low-fiber diet might be suggested to prevent blockages. Staying active, managing stress, and avoiding certain foods can also help.
What is the emotional impact of living with Crohn’s disease?
Crohn’s disease can really affect your mood, causing anxiety and depression. Talking to a therapist or joining a support group can help. Sharing stories with others who understand can make you feel less alone.