FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Did you know CML is rare, affecting 1 in 100,000 people yearly? It’s a bone marrow cancer that makes too many white blood cells. Thanks to new treatments, most people can live long after being diagnosed.
CML starts in the bone marrow, where blood cells are made. It’s called “chronic” because it grows slowly. This article will cover CML’s causes, symptoms, diagnosis, and treatments.
Key Takeaways
- Chronic myelogenous leukemia (CML) is an uncommon type of blood cancer that affects the bone marrow.
- CML is characterized by an abnormal increase in white blood cell production, leading to a buildup in the blood and bone marrow.
- CML typically affects older adults, although it can occur at any age.
- The presence of the Philadelphia chromosome is a hallmark of CML, found in 90% of cases.
- Advances in targeted therapies have greatly improved the prognosis for CML patients, allowing most to achieve remission and live for many years.
What is Chronic Myelogenous Leukemia?
Chronic myelogenous leukemia (CML) is a cancer that starts in the bone marrow’s blood-forming cells. It happens when a genetic change creates an abnormal gene called BCR-ABL. This gene turns the cell into a CML cell.
These leukemia cells grow and divide, filling the bone marrow and blood. CML grows slowly but can quickly turn into a fast-growing leukemia that’s harder to treat.
Overview
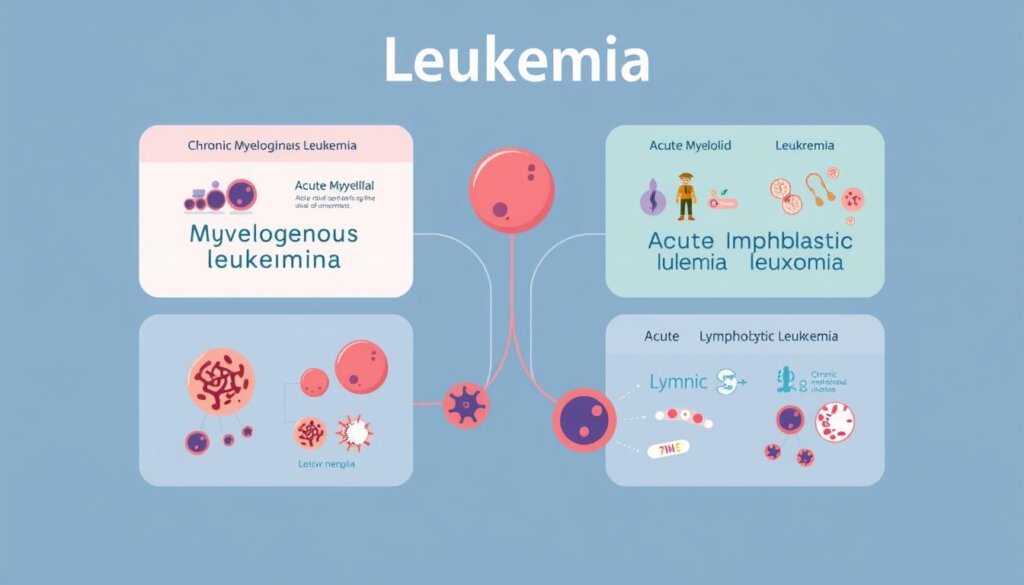
Leukemia is either acute or chronic, and myeloid or lymphocytic, based on the blood cells affected and how fast it grows. Chronic leukemias like CML have cells that mature partly but not completely. Acute leukemias have immature cells that grow quickly.
Types of Leukemia
There are 4 main types of leukemia: Acute Myeloid Leukemia (AML), Chronic Myeloid Leukemia (CML), Acute Lymphocytic Leukemia (ALL), and Chronic Lymphocytic Leukemia (CLL). Chronic myelomonocytic leukemia (CMML) is another chronic leukemia that starts in myeloid cells.
Lymphocytic leukemias differ from lymphomas in where the cancer cells are found. Leukemia cells are mainly in the bone marrow and blood. Lymphoma cells are in lymph nodes and other tissues.
Type of Leukemia | Description |
|---|---|
Acute Myeloid Leukemia (AML) | Rapidly progressing leukemia that affects myeloid cells |
Chronic Myeloid Leukemia (CML) | Slower-growing leukemia that affects myeloid cells |
Acute Lymphocytic Leukemia (ALL) | Rapidly progressing leukemia that affects lymphocytes |
Chronic Lymphocytic Leukemia (CLL) | Slower-growing leukemia that affects lymphocytes |
Chronic Myelomonocytic Leukemia (CMML) | Chronic leukemia that originates in myeloid cells |
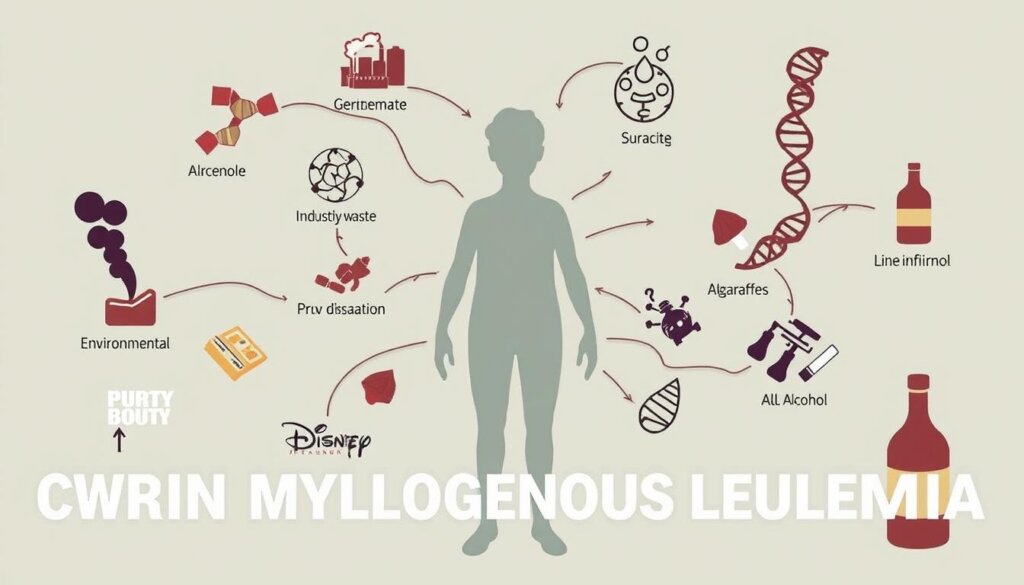
Causes and Risk Factors
Chronic myelogenous leukemia (CML) is a blood cancer that starts in the bone marrow. We don’t know the exact cause, but some factors can raise your risk.
The Philadelphia Chromosome
Most CML patients have a special chromosome called the Philadelphia chromosome in their blood cells. This happens when chromosomes 9 and 22 swap parts. This creates a new gene, BCR-ABL, that makes blood cells grow too much.
Risk Factors for CML
CML is linked to radiation and age. It mostly affects adults, especially after middle age, and is rare in kids. Men are slightly more likely to get it than women.
Being exposed to radiation, like from an atomic bomb, raises your risk. High doses of radiation also increase your risk.
Smoking, diet, chemicals, and infections don’t seem to affect your risk. The Philadelphia chromosome isn’t passed down from parents. CML isn’t inherited.
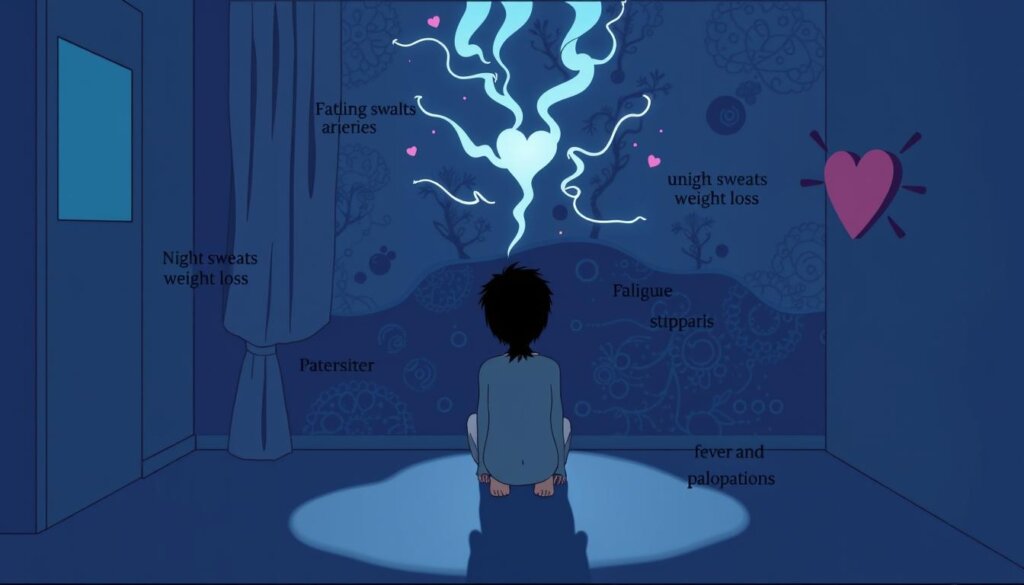
Symptoms of Chronic Myelogenous Leukemia
Many people with chronic myelogenous leukemia (CML) don’t show symptoms early on. But as it gets worse, symptoms like bone pain and easy bleeding start. You might also feel full after eating a little, tired, or have a fever.
Other symptoms include weight loss, loss of appetite, and pain in the left upper abdomen. This pain is often from an enlarged spleen (splenomegaly).
CML can also affect blood cells. Anemia makes you weak and tired. Leukopenia raises your risk of getting sick.
Neutropenia can cause serious infections. Thrombocytopenia leads to easy bruising and bleeding. This includes frequent or severe nosebleeds and bleeding gums.
An abnormal white blood cell count is a key sign of CML. It’s worth noting that CML is rare in kids, making up only 1 percent of childhood leukemias. Kids with CML might have anemia, bleeding, bone pain, and more.
If you notice these symptoms, see a doctor right away. Early treatment can make a big difference in managing CML.
Diagnosis and Testing
Diagnosing chronic myelogenous leukemia (CML) needs several tests and scans. First, tests look for the Philadelphia chromosome or BCR-ABL gene. These tests are done through cytogenetic testing, FISH, and PCR.
Laboratory Tests
Other tests include a blood count and a chemistry panel. A hepatitis panel and BCR-ABL PCR are also done. These tests are repeated every 3 months after starting treatment.
More tests like flow cytometry and mutational analysis might be needed.
Bone Marrow Aspiration and Biopsy
A bone marrow test is key for diagnosis. Pathologists check blood and bone marrow cells. They look for different white blood cells and blast cells.
In CML, white blood cells are often high. Platelets can be too high or too low. Most people with CML have the BCR-ABL mutation.
Fluorescence in situ hybridization finds the Philadelphia chromosome. The PCR test looks for the chromosome if FISH doesn’t find it.
Quantitative PCR measures BCR-ABL in the blood. About 95% of people with CML have the Ph chromosome in bone marrow. In some cases, the BCR::ABL1 gene is found even without the Ph chromosome.

Quantitative Polymerase Chain Reaction (qPCR) finds and measures the BCR::ABL1 gene. It can spot small amounts of the gene. Fluorescence In Situ Hybridization (FISH) is more sensitive than standard tests.
Chronic Myelogenous Leukemia Phases
Chronic myelogenous leukemia (CML) is a complex blood cancer. It goes through different phases. Knowing these phases is key for treating and managing the disease.
Chronic Phase
The chronic phase is the first stage of CML. It’s a slow-moving disease. In this phase, the blood has more granulocytes and other cells, but less than 2% are blast cells.
Patients in this phase often do well with standard treatments.
Accelerated Phase
The disease can move to the accelerated phase next. This stage has more blast cells and other changes. Symptoms like fever and weight loss can appear.
Blast Phase
The final stage is the blast phase or blast crisis. Here, the disease becomes very aggressive. Blast cells are over 20% in the blood or bone marrow.
Symptoms can be severe. It’s like acute leukemia.
Going to the accelerated or blast phase means a worse outlook for CML patients. Doctors use scores like the Sokal system to guess survival chances. These scores look at age, spleen size, and blood cell counts.
“Understanding the different phases of chronic myelogenous leukemia is crucial for providing the best possible care and support to patients.”
Treatment Options
Chronic myelogenous leukemia (CML) is mainly treated with targeted therapy. This uses tyrosine kinase inhibitors (TKIs). These drugs target the BCR-ABL fusion protein that makes CML cells grow.
Several FDA-approved TKIs are used as first-line treatments for chronic phase CML. These include imatinib (Gleevec®), dasatinib (Sprycel®), nilotinib (Tasigna®), and bosutinib (Bosulif®).
Tyrosine Kinase Inhibitors for CML
Imatinib is a first-generation TKI. Dasatinib, nilotinib, and bosutinib are second-generation TKIs. For those with intermediate- or high-risk chronic phase CML, second-generation TKIs may offer more benefits than imatinib.
Ponatinib, a third-generation TKI, is a third-line option for patients who have failed multiple TKIs or have the T315I mutation.
TKIs stop CML cells from growing and surviving. This leads to better outcomes for patients. Side effects can include swelling, nausea, muscle cramps, fatigue, diarrhea, and skin rashes.
Tyrosine Kinase Inhibitor | FDA Approval for CML |
|---|---|
Imatinib (Gleevec®) | First-line treatment for chronic phase CML |
Dasatinib (Sprycel®) | First-line treatment for chronic phase CML |
Nilotinib (Tasigna®) | First-line treatment for chronic phase CML |
Bosutinib (Bosulif®) | First-line treatment for chronic phase CML |
Ponatinib | Third-line treatment for CML patients who have failed multiple TKIs or have the T315I mutation |
Other treatment options for CML include stem cell transplantation, chemotherapy, and clinical trials. It’s important to talk about your treatment plan with your healthcare provider. Consider the CML phase, test results, prognostic factors, and other health issues.
Remember, talking openly with your healthcare team is key to managing CML. This helps achieve the best possible outcomes.
Stem Cell Transplantation
Stem cell transplantation is a treatment for some CML patients. It’s for those who have reached advanced stages or didn’t do well with other treatments. The process kills the bad bone marrow with strong chemo and then adds healthy stem cells from a donor.
This method can cure CML but is risky. It’s mainly for those who have tried other treatments without success.
Allogeneic stem cell transplant uses donor stem cells. It’s the main way to treat CML. It might cure CML but isn’t good for older patients or those with health problems.
Stem cell transplant is now less common for CML. This is because of tyrosine kinase inhibitors (TKIs), which are the usual treatment.
Younger patients, especially kids and those with a matching donor, might get this transplant. It’s also for those not doing well with TKIs or in advanced stages. High doses of chemo are often avoided because of bad side effects.
For a transplant, chemo kills leukemia cells, then healthy stem cells are added to fix the bone marrow. These stem cells can come from blood or bone marrow, with blood being more common.
There are two main types of stem cell transplants: autologous and allogeneic. Allogeneic is used more for CML because of the risk of getting leukemia cells with the stem cells. This type can lead to serious or life-threatening problems.
Thanks to new treatments, CML patients are living longer. Tyrosine kinase inhibitors have helped lower death rates in CML patients in Japan and the U.S.. But, stem cell transplantation is still key in managing CML, with results depending on risk assessments and early detection.
Key Transplant Statistics for CML | Value |
|---|---|
Allogeneic stem cell transplant – Proven chance to cure CML | Yes |
Stem cell transplant use for CML – Decreased due to TKIs | Yes |
Patients recommended for allogeneic transplant | Younger patients, those with matched donors, those not responding to TKIs, those in the accelerated/blast phase |
Chemotherapy intensity – Typically avoided due to side effects | Yes |
Stem cell source – Peripheral blood more common than bone marrow | Yes |
Allogeneic transplant – Risk of severe/life-threatening complications | Yes |
In summary, stem cell transplantation, especially allogeneic, is still a big deal for CML patients. It’s risky but can cure CML in some cases. Research keeps working to make this treatment better for more patients.
Living with Chronic Myelogenous Leukemia
Living with chronic myelogenous leukemia (CML) can be tough. It affects your body, mind, and daily life. CML makes up almost 15% of all adult leukemia. It’s a rare leukemia.
Dealing with treatment side effects and fatigue is hard. Navigating the healthcare system can also be stressful. But, many people with CML live well with the right support.
Coping and Support
Support groups and counseling help a lot. Talking to others with CML can be very helpful. Exercise, healthy eating, and therapies like acupuncture can also help manage side effects.
There are ways to get help with treatment costs. Social workers, care teams, and groups like the American Cancer Society can offer financial aid. Talking to your employer about work arrangements can also help.
Coping Strategies for CML Patients | Supportive Resources |
|---|---|
|
|
With the right care, people with CML can live for many years. New treatments have improved survival rates. Regular check-ups with your doctor are key.
“The key to living well with CML is to be proactive in your care, maintain open communication with your healthcare team, and seek out the support and resources that can help you navigate this journey.”
By using a full approach to coping and support, people with chronic myelogenous leukemia can improve their life quality. They can find hope in managing their disease for the long term.
Monitoring and Follow-up Care
Ongoing CML monitoring and follow-up care are key for managing chronic myelogenous leukemia (CML). Regular blood tests check BCR-ABL levels, showing how well treatment works. Patients see their oncologist often to talk about test results and treatment changes.
Bone marrow tests may be done to check for changes. The main test is a PCR test to see how well TKI treatment is working. Other tests, like CBC and imaging, are also used.
It’s important to stay in touch with your healthcare team and follow your care plan. Most people with CML stay on TKI treatment forever.
Molecular Response (MR) Levels | Percentage of Cells with BCR-ABL1 Gene |
|---|---|
MR1 | 10% or less |
MR2 | 1% or less |
MR3 (Major Molecular Response) | 0.1% or less |
MR4 (Deep Molecular Response) | 0.01% or less |
MR5 (Deep Molecular Response) | 0.001% or less |
Levels of cytogenetic response are also watched in bone marrow cells.
- Complete cytogenetic response: None or less than 1% of cells contain Philadelphia chromosome.
- Partial cytogenetic response: Between 1 and 35% of cells contain Philadelphia chromosome.
- Minor cytogenetic response: Between 36 and 65% of cells contain Philadelphia chromosome.
- Minimal cytogenetic response: Between 66 and 95% of cells contain Philadelphia chromosome.
- No cytogenetic response: More than 95% of cells contain Philadelphia chromosome.
Those who had a stem cell transplant will have many checkups and tests. Getting emotional support from friends, family, or groups is very helpful.
“Studies have shown that missing doses or not taking the right dose of TKI drugs can lead to worse overall outcomes.”
Living a healthy lifestyle, like not smoking and eating well, can help your health.
In summary, regular CML monitoring and follow-up care are key for managing CML.
Conclusion
Chronic myelogenous leukemia (CML) has seen big changes in recent years. New treatments like tyrosine kinase inhibitors have made a big difference. These treatments have greatly improved life for many CML patients.
With the right treatment and care, most people with CML can live longer and feel better. This is a big step forward.
But CML is still a serious disease that needs careful watching. More research and understanding of CML could lead to even better treatments. As CML cases are expected to grow in the U.S., teamwork between patients and doctors is key.
Even though survival rates for CML patients have gotten better, the fight against CML is ongoing. By staying informed and working with doctors, people with CML can face their disease with hope. They can keep living well despite the challenges.
FAQ
What is chronic myelogenous leukemia (CML)?
CML is a rare cancer that affects the bone marrow. It’s where blood cells are made. It causes more white blood cells in the blood.
What causes CML?
A genetic change causes CML. It creates an abnormal gene called BCR-ABL. This turns blood cells into CML cells.
What are the symptoms of CML?
Early symptoms of CML are rare. But, they can include bone pain and bleeding easily. Feeling full after eating a little and fatigue are also symptoms.
Other symptoms are fever, weight loss, and loss of appetite. An enlarged spleen and blurry vision can also happen.
How is CML diagnosed?
Blood tests diagnose CML. They look for the Philadelphia chromosome or BCR-ABL gene. A bone marrow test is also key for diagnosis.
What are the phases of CML?
CML has three phases: chronic, accelerated, and blast. The chronic phase is the most treatable. The other phases are less treatable.
What are the treatment options for CML?
First-line treatments are TKI medications like imatinib. Dasatinib, nilotinib, and bosutinib are also options. For some, stem cell transplantation is a choice.
How is CML monitored and managed long-term?
Long-term care for CML is crucial. Regular blood tests and bone marrow tests are needed. Patients work with their team to manage treatment and side effects.