FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
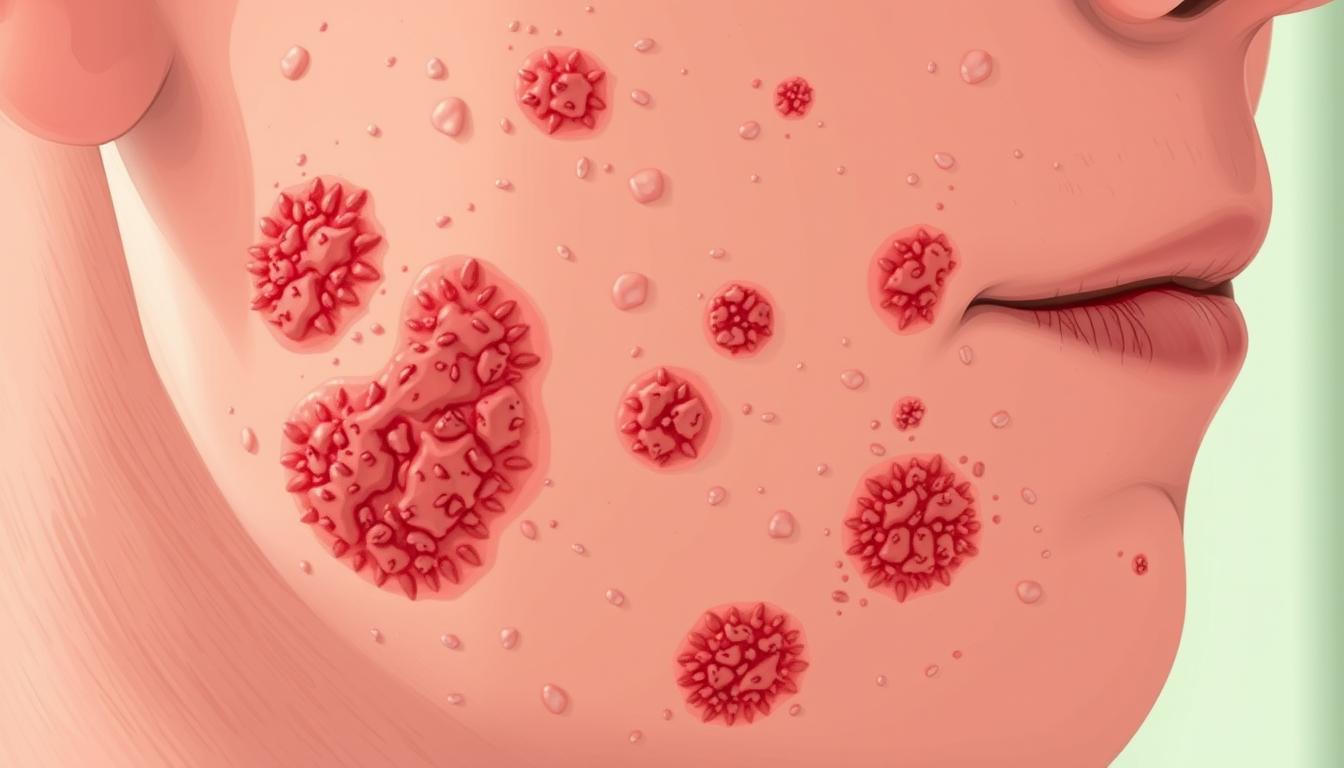
Actinic keratosis is a serious condition found in nearly 60% of Australians and 20% of Americans. This is because they live near the equator and get a lot of UV radiation. These rough, scaly patches on the skin can turn into skin cancer if not treated. It’s very important to know what causes it, its symptoms, and how to treat it.
UV rays from the sun and tanning beds cause actinic keratosis. People with fair skin, blonde or red hair, and light eyes are more at risk. They have less melanin to protect their skin from UV damage. Older adults and those with weak immune systems are also more likely to get it. This is because they have been exposed to more UV rays and their immune system is not strong.
It’s key to know the causes and risks of actinic keratosis to prevent and manage it. By doing regular skin checks, protecting your skin from the sun, and treating it early, you can lower the risk of it turning into skin cancer.
Key Takeaways
- Actinic keratosis is a precancerous skin condition caused by prolonged UV exposure from the sun and tanning beds.
- Individuals with fair skin, light hair, eye color, and weakened immune systems are at higher risk for developing actinic keratosis.
- Actinic keratosis lesions commonly appear on sun-exposed areas of the body and can vary in appearance from flat patches to rough, scaly bumps.
- Early detection and treatment are crucial to prevent the progression of actinic keratosis to squamous cell carcinoma, a type of skin cancer.
- Proactive measures, such as regular skin exams and consistent sun protection, can help reduce the risk of developing actinic keratosis.
What is Actinic Keratosis?
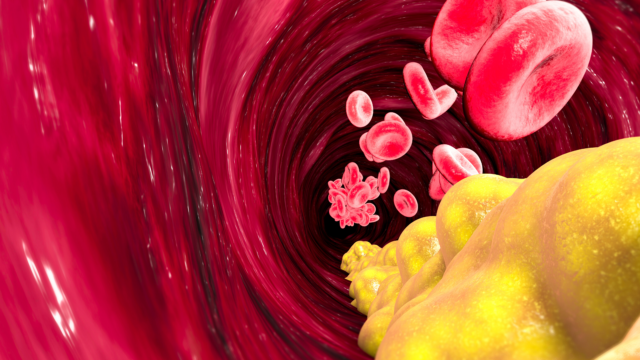
Actinic keratosis, also known as solar keratosis, are precancerous skin lesions caused by long-term exposure to UV radiation from the sun. These lesions appear as rough, scaly patches or bumps on the skin, often on sun-exposed areas like the face, lips, scalp, arms, and hands. While actinic keratoses are not life-threatening, they can develop into squamous cell carcinoma, a type of skin cancer, if left untreated.
Precancerous Skin Lesions
Actinic keratoses are considered precancerous lesions because they have the potential to progress into a type of skin cancer called squamous cell carcinoma. In fact, the majority of squamous cell carcinomas start off as actinic keratosis. Regular monitoring and early treatment of actinic keratoses are crucial to prevent this progression.
Rough, Scaly Patches
The distinctive appearance of actinic keratoses is characterized by rough, scaly patches or bumps on the skin. These lesions often develop on sun-exposed areas of the body, such as the face, lips, scalp, arms, and hands. The skin affected by actinic keratosis may feel like sandpaper or appear discolored, ranging from red to brown or gray.
Actinic keratoses are a common condition, with an estimated 58 million Americans having one or more of these lesions. While not all actinic keratoses will progress to skin cancer, it is important to monitor them and seek prompt treatment, as 5-10% of these lesions can turn into squamous cell carcinoma.
Key Facts about Actinic Keratosis | Data |
|---|---|
Prevalence in the US | 58 million Americans have one or more Actinic Keratosis (AKs) |
Progression to Skin Cancer | 5-10% of AKs turn into skin cancer, predominantly squamous cell carcinomas |
Relationship to Squamous Cell Carcinoma | The majority of squamous cell carcinomas start off as Actinic Keratosis |
Common Affected Areas | Actinic Keratosis often appears on sun-exposed areas such as the face, lips, ears, scalp, shoulders, neck, and hands |
Potential Complications | An untreated squamous cell carcinoma can become invasive and life-threatening |
Importance of Early Detection | Early detection of Actinic Keratosis allows for effective treatment before progressing to skin cancer |
Risk Factors for Actinic Keratosis
Actinic keratosis is a skin condition that can turn into cancer. It’s caused by UV radiation from the sun or tanning beds. People with fair skin, light hair, and light eyes are more likely to get it. Older adults also face a higher risk.
Those with weak immune systems, like organ transplant recipients or people with HIV/AIDS, are more at risk.
Sun Exposure and UV Radiation
Long-term exposure to UV radiation causes actinic keratosis. People near the equator, where UV rays are stronger, are more likely to get it. Not using sunscreen or protective clothes when in the sun raises the risk over time.
Fair Skin and Older Age
Those with fair skin, especially red or blonde hair, and light eyes are more likely to get actinic keratosis. The risk goes up with age as more sun damage builds up.
Immunosuppression
Weakened immune systems increase the risk of actinic keratosis. This includes organ transplant recipients and people with HIV/AIDS.
It’s important to know and deal with these risk factors. This helps manage and prevent actinic keratosis and lower the chance of skin cancer.
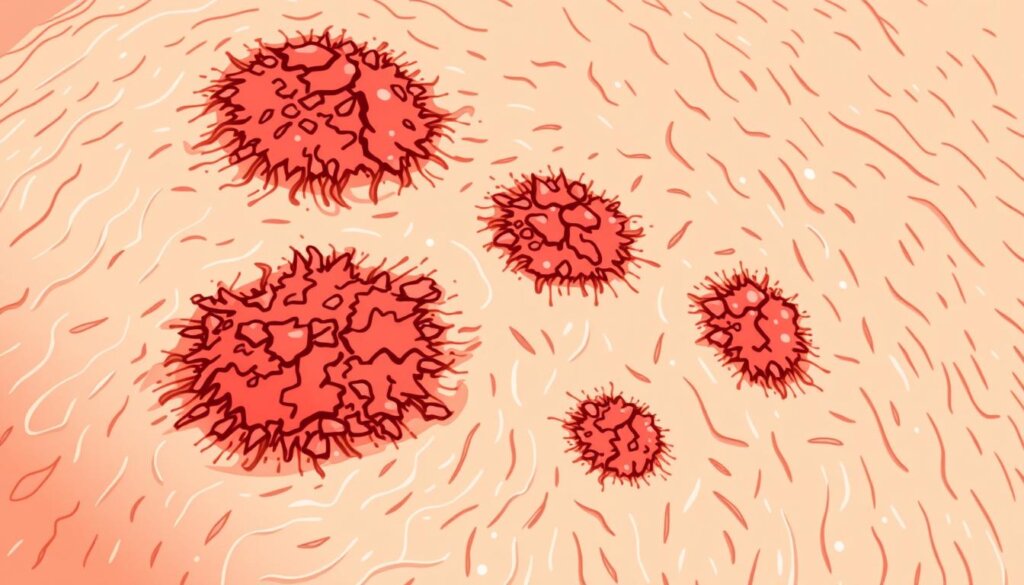
Symptoms of Actinic Keratosis
Actinic keratosis lesions show up as rough, scaly patches or bumps on sun-exposed skin. They can be light or dark, tan, pink, or red. Some may itch, hurt, or feel prickly. People often have more than one of these lesions, and those on the lips are called actinic cheilitis.
The most common symptoms of actinic keratosis include:
- Rough, scaly patches on the skin
- Itching or a prickly sensation
- Soreness or tenderness
- Varied coloration, ranging from light to dark, tan, pink, or red
Actinic keratosis lesions often appear on sun-exposed areas. This includes the face, ears, scalp, hands, legs, and arms. Also, having many of these lesions can increase the risk of skin cancer, like squamous cell carcinoma.
“About 90% of actinic keratoses do not turn into skin cancers, but almost all squamous cell carcinomas of the skin originate from actinic keratoses.”
Regular skin checks and quick treatment of actinic keratosis are key. This helps prevent more serious skin problems.

Diagnosis of Actinic Keratosis
Identifying actinic keratosis starts with a clinical examination by your doctor. They look at your skin and feel the texture of the lesions. Sometimes, a skin biopsy is needed to confirm it, especially if it looks like skin cancer.
Dermoscopy is also used to help diagnose actinic keratosis. It uses a special device to look closely at your skin. This helps your doctor see signs of actinic keratosis. Dermoscopy is great for telling actinic keratosis apart from other skin issues, like lentigo maligna.
Clinical Examination
Your doctor will look at your skin and feel the texture of the lesions during an exam. They might also ask about your health history and symptoms.
Dermoscopy and Biopsy
If the exam isn’t clear or if your doctor thinks it might be cancer, they might suggest more tests. This could be a skin biopsy or a dermoscopic check. A biopsy takes a small skin sample for analysis, while dermoscopy shows detailed info about the lesion’s structure and look.
It’s important to see your dermatologist regularly, especially if you’ve had a lot of sun damage or have many actinic keratosis spots. Catching actinic keratosis early and treating it can stop skin cancer from happening.
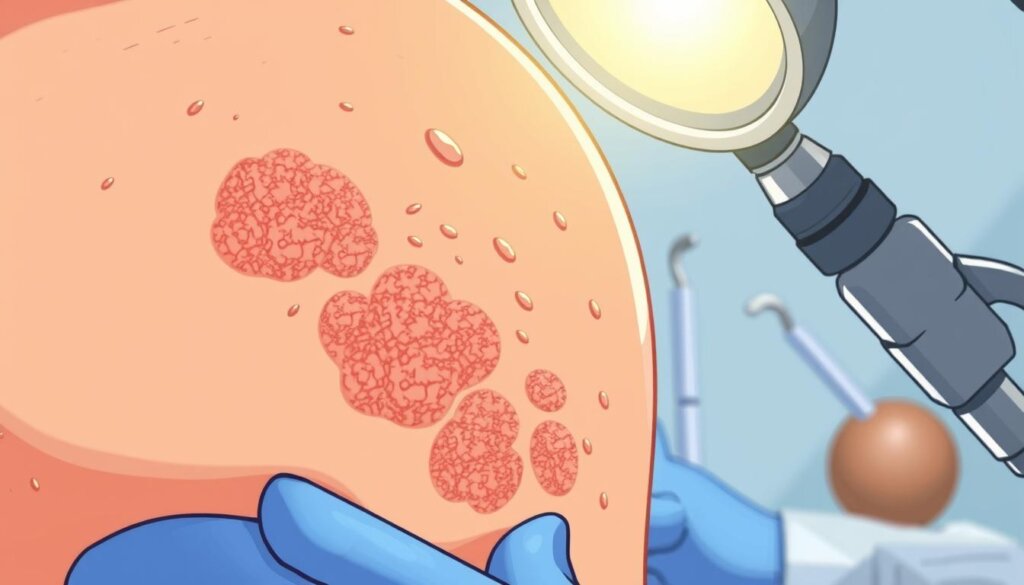
Treatment Options for Actinic Keratosis
Actinic keratosis, those precancerous skin lesions, can be treated in many ways. Each treatment is chosen based on what the patient needs. There are destructive therapies, topical medications, and field ablation treatments to choose from.
Lesion-Directed Therapies
For single or small groups of actinic keratosis, doctors might suggest specific treatments. These include freezing, scraping, and surgery. Cryosurgery and laser surgery are often used to treat single spots, leaving little to no scar.
Field-Directed Therapies
For many or widespread actinic keratosis, doctors prefer field-directed treatments. These treatments cover the whole sun-damaged area. Topical creams like fluorouracil and imiquimod are applied to the area. Photodynamic therapy (PDT) is also effective, especially for the face and scalp.
Choosing a treatment depends on several factors. These include how many lesions there are, where they are, the patient’s age, and health. It’s important to avoid the sun after treatment to prevent burns and improve results. Regular self-checks and visits to the dermatologist are key to catching any new or growing lesions and to watch for skin cancer.
“Majority of cutaneous squamous cell carcinomas (cSCCs) arise from pre-existing actinic keratoses (AKs), and AKs that progress to squamous cell carcinoma cannot be distinguished from AKs that will resolve or persist.”
Treatment Modality | Efficacy |
|---|---|
Cryotherapy | 38% response rate |
Topical 5-Fluorouracil | 44% response rate |
Imiquimod 5% Cream | 50% clearance rate, 58% clearance rate on the head |
Preventive Strategies
Keeping your skin safe from UV rays is key to avoiding actinic keratosis. Stay away from tanning beds and sun because they harm your skin and can cause cancer. Kids need extra care because they spend more time outside and can get sunburned easily. Parents and caregivers should protect them.
Seeing a doctor for skin checks is important. It helps find actinic keratosis and other skin issues early. This way, you can treat them quickly and lower the chance of skin cancer. Many visits to doctors are for actinic, showing how vital these check-ups are. Also, some chemicals like arsenic can increase skin cancer risk. Knowing and avoiding these chemicals is important.
Sun Protection
Protecting your skin from the sun is a top way to prevent actinic keratosis. Use sunscreen with at least SPF 30, wear clothes that cover you, and don’t stay in the sun too long. Also, UV from tanning beds can hurt your skin as much as the sun. So, it’s best to avoid them too.
Regular Skin Examinations
Getting regular skin checks can catch new growths or odd spots early. This can stop them from turning into skin cancer. Finding problems early is key for quick treatment and less chance of skin cancer getting worse. Smoking also raises the risk of squamous cell skin cancer. Quitting can help lower this risk.
People with weak immune systems are more at risk for skin cancer and may face treatment challenges. It’s important to avoid things that weaken your immune system to prevent skin cancer. Some people at higher risk might benefit from special drugs to lower skin cancer risk. But, more research is needed to find good medicines.
By knowing and using these prevention tips, you can help lower your risk of actinic keratosis and skin cancers. Most skin cancers start from actinic keratoses. This shows how critical early prevention and action are.
Preventive Measure | Effectiveness |
|---|---|
Sun protection (sunscreen, protective clothing, avoiding UV exposure) | Highly effective in reducing the risk of actinic keratosis and skin cancer |
Regular skin examinations | Crucial for early detection and prevention of skin cancer progression |
Smoking cessation | Lowers the risk of squamous cell skin cancer and other cancers |
Immune system support | Important for individuals at higher risk of skin cancer |
Chemoprevention drugs | Ongoing research to identify effective medications for reducing skin cancer risk |
“Understanding skin cancer prevention strategies and implementing protective measures to limit exposure to UV rays can help lower the risk of basal and squamous cell skin cancers.”
Actinic Keratosis
Actinic keratosis is a common skin problem caused by UV radiation from the sun. It shows up as rough, scaly patches or bumps. These can turn into squamous cell carcinoma if not treated. It’s important to catch it early and treat it right to stop it from getting worse.
Internists say actinic keratoses are a big deal, with 1396 cases per 100,000 people every year. Studies show a small chance of these spots turning into cancer, from 0.025% to 16%. In places like Queensland, Australia, 31% of people over 40 have them.
These spots are usually under 2 cm and hit people over 50 hard. They show up on sun-exposed areas like the face and arms. People with light skin and eyes are more at risk.
It’s key to catch and treat actinic keratosis early to stop it from becoming cancer. There are many ways to treat it, like creams, freezing, and lasers. Early action can lower the risk of serious skin cancer.
Actinic Keratosis | Seborrheic Keratosis |
|---|---|
Precancerous skin lesions caused by UV radiation exposure | Noncancerous skin growths that are not related to sun damage |
Usually smaller than 2 cm in size | May reach about 1 inch in diameter |
More common in individuals over age 50 | Uncommon in people under age 20, often develops in 30s or 40s |
More likely to occur in individuals with light skin and eyes | Tends to affect individuals with lighter skin more commonly |
Treatment options: Topical therapies, cryosurgery, laser treatments | Treatment options: Cryosurgery, electrosurgery, curettage, ablation, topical solutions |
Knowing about actinic keratosis and how to treat it can help people fight it. This can lower the chance of getting skin cancer.
Potential Progression to Skin Cancer
Actinic keratosis lesions can turn into squamous cell carcinoma if not treated. The risk of this happening is about 8% on average. But, this risk can change based on many factors. It’s important to catch and treat actinic keratosis early to lower the risk of it becoming skin cancer.
Actinic Keratosis with Atypical Basal Cells (AK I) is often linked to skin cancer. Also, hyperkeratotic actinic keratoses have a high chance of turning into cancer. Studies on treating actinic keratoses with 0.5% 5-Fluorouracil and salicylic acid show the need for effective treatment.
Most squamous cell carcinomas start as actinic keratoses. The more UV radiation you get, the higher your risk of actinic keratosis and skin cancer. But, it’s hard to tell which actinic keratoses will turn into cancer.
A study found signs that can predict squamous cell carcinoma in certain groups. This shows why regular skin checks are key for those at risk, like those with actinic keratosis.
In short, actinic keratosis can turn into squamous cell carcinoma if not treated. Quick action and the right treatment are key to stopping this from happening and preventing skin cancer.
Importance of Early Detection
Actinic keratosis needs quick diagnosis and treatment to stop skin cancer. Early treatment can manage actinic keratosis well. This lowers the chance of it turning into squamous cell carcinoma. Getting regular skin checks from a doctor is key for catching actinic keratosis and other skin issues early.
Actinic keratoses often show up in sun-exposed areas, especially in older people. People with lighter skin (Fitzpatrick Skin Phototypes I and II) are more at risk because they have less melanin. Men are more likely to get actinic keratosis than women.
In the U.S., about 20% of people have actinic keratosis. The risk of it turning into cancer is 8% for most people, but it can vary. Finding and treating actinic keratosis early can greatly lower the risk of it becoming skin cancer.
Skin Cancer Statistic | Value |
|---|---|
One in six Americans develops skin cancer at some point in their lives | |
Skin cancer accounts for one-third of all cancers in the United States. | |
Melanoma is the eighth most common malignancy in the United States. | |
Incidence of melanoma is rapidly increasing, with one in 1,500 Americans born in 1935 likely to develop melanoma compared to one in 105 persons born in 1993 | |
Mortality rates from skin cancer are higher in men than in women, with men having a higher risk due to lesions often developing in less observable areas. | |
Mortality rates are also increased in blacks due to the tendency to develop aggressive tumors and to be diagnosed at later stages. |
The rise in skin cancer is due to more sun exposure and less ozone. Nonmelanoma skin cancer mostly affects older people, while melanoma often hits between 20 and 45. People who work outside a lot are at higher risk.
Having had skin cancer before makes you more likely to get it again in five years. Sun exposure early in life is a big risk factor for skin cancer. Getting badly sunburned as a kid or teen also raises your risk.
“Early detection is key to successfully treating skin cancer. Regular skin exams can identify abnormal growths and lesions before they become problematic.”
Understanding the importance of early detection and being proactive can greatly improve your chances of beating skin cancer. Regular skin checks and quick action on any unusual changes can make a big difference in managing actinic keratosis and other skin issues.
Role of the Healthcare Team
Managing actinic keratosis needs a team effort. This team includes primary care providers and dermatologists.
Primary care providers start by checking for actinic keratosis. They then send patients to dermatologists for more help. Dermatologists are the experts in treating actinic keratosis.
The healthcare team teaches patients about sun protection and regular skin checks. This helps stop actinic keratosis from getting worse.
Together, the healthcare team makes sure actinic keratosis is caught and treated right. This lowers the chance of it turning into skin cancer.
“Early detection and management of actinic keratosis are essential to preventing the development of skin cancer.” – Dr. Jane Doe, Dermatologist
Conclusion
Actinic keratosis is a common skin problem that needs careful watching and quick action. Lots of research has been done on it. This shows it can turn into cancer and what increases this risk.
Even though some studies say it might go away on its own, most agree early treatment is key. This helps stop skin cancer from happening.
The numbers on actinic keratosis are really high. It costs over $1 billion a year in the USA and affects almost 40 million people. This makes it a big health issue.
Also, up to 60% of squamous cell carcinomas come from actinic keratosis. This shows we need to catch it early and stop it before it’s too late.
By using sun protection and checking your skin often, you can lower your risk. People with actinic keratosis are 5.1 times more likely to get skin cancer. This is why watching your skin and acting fast is so important.
Working with doctors can help you deal with actinic keratosis. This way, you can lower the chance of it turning into skin cancer.
FAQ
What is actinic keratosis?
Actinic keratosis is a rough, scaly patch or bump on the skin. It’s caused by UV damage. These lesions can turn into squamous cell skin cancer if not treated.
What are the risk factors for developing actinic keratosis?
Risk factors include UV radiation from the sun or tanning beds. Fair skin, light hair and eyes, older age, and weakened immune systems also increase risk.
What are the symptoms of actinic keratosis?
Symptoms include rough, scaly patches or bumps on sun-exposed skin. They can be light or dark, tan, pink, or red. Some may itch, sore, or feel prickly.
How is actinic keratosis diagnosed?
Doctors can usually spot actinic keratosis by looking and feeling the skin. Sometimes, a skin biopsy or dermoscopy is needed to confirm it.
What are the treatment options for actinic keratosis?
Treatments include cryotherapy, curettage, and surgical excision. Field-directed therapies like topical medications, photodynamic therapy, and laser resurfacing are also options.
How can actinic keratosis be prevented?
Protect your skin from UV radiation with sunscreen and protective clothing. Avoid too much sun. Regular skin checks can also help catch actinic keratosis early.
What is the risk of actinic keratosis progressing to skin cancer?
Actinic keratosis can turn into squamous cell carcinoma, a skin cancer. The risk is about 8%, but it can vary based on individual factors.
Why is early detection and treatment of actinic keratosis important?
Early detection and treatment are key to preventing skin cancer. Catching it early means it can be managed, reducing the risk of turning into squamous cell carcinoma.
How does the healthcare team manage actinic keratosis?
The healthcare team, including primary care providers and dermatologists, work together. They provide expert care, treatment, and follow-up. They also teach patients about sun protection and regular skin checks.