FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Did you know brachytherapy has been treating cancer since 1901? It’s a special kind of radiation therapy. Radioactive sources are placed right in or near the tumor, allowing more radiation to be given while keeping healthy tissues safe.
Brachytherapy is changing the game in cancer fights. It helps with prostate, breast, cervical, and more cancers.
Key Takeaways
- Brachytherapy is a targeted radiation therapy that places radioactive sources directly into or near a tumor.
- It allows for higher doses of radiation while minimizing damage to surrounding healthy tissues.
- Brachytherapy is used to treat a variety of cancers, including prostate, breast, and cervical.
- There are different types of brachytherapy, including low-dose rate (LDR) and high-dose rate (HDR).
- Brachytherapy is as effective as external beam radiation therapy and surgery for many cancers.
What is Brachytherapy?
Definition and Overview of Brachytherapy
Brachytherapy is a special way to treat cancer. It involves putting radioactive sources right into or near the tumor. This method gives high doses of radiation to the cancer while protecting healthy tissues.
It has been used since the early 1900s. Over time, technology and techniques have improved a lot.
The name “brachytherapy” comes from the Greek word “brachy” meaning short distance. This shows how the radioactive sources are close to the tumor. It can be used alone or with other treatments like surgery or external beam radiation.
Brachytherapy is used for many cancers. These include brain, breast, cervical, lung, rectal, and skin cancer. The treatment can be temporary or permanent. The radioactive material can be placed temporarily or left in the body to give a weakening dose over time.

“Brachytherapy allows for the delivery of higher doses of radiation directly to the treatment area compared to external radiation.”
How Brachytherapy Works
Brachytherapy is a precise cancer treatment. It places radioactive sources right in or near the tumor. These sources kill cancer cells while keeping healthy tissues safe.
The sources are placed using a thin tube called a catheter or a larger device called an applicator. The treatment’s length and dose are set for each patient.
This method targets tumors well, killing cancer cells effectively. It also protects healthy tissue from harm.
Brachytherapy sessions are short and can be done near imaging tests. They are not painful and last just minutes. Patients can go home with little discomfort in between sessions.
Types of Brachytherapy Radiation Delivery
Brachytherapy has two types: LDR and HDR. LDR uses small radioactive seeds to treat prostate cancer, while HDR delivers high doses quickly, often for prostate and gynecological cancers.
Both LDR and HDR are effective for treating cancers like cervical cancer. Patients are treated under general anesthesia and need to fast for 6 hours.
Types of Brachytherapy
Brachytherapy is a targeted radiation therapy with different delivery methods. Each type has its own benefits. The main types are low-dose rate (LDR), high-dose rate (HDR), and permanent implants.
Low-Dose Rate (LDR) Brachytherapy
LDR brachytherapy uses radioactive sources like seeds or pellets. They are placed in or near the tumor. These sources stay for 1 to 7 days, and the patient must stay in the hospital.
This method is often used for prostate and brain tumors.
High-Dose Rate (HDR) Brachytherapy
HDR brachytherapy gives a high dose in short sessions, lasting 10-20 minutes. Patients visit the hospital daily or weekly for these sessions.
It’s mainly used for prostate, cervical, and head and neck cancers.
Permanent Implants
Permanent implants, like radioactive seeds, are left in the body. The radiation slowly fades over time. This method is often used for prostate cancer.
The choice of brachytherapy depends on the cancer type, stage, and patient’s health. Brachytherapy can be very effective for many cancers. It offers a targeted and convenient way to treat cancer with radiation.
Brachytherapy Procedures
Brachytherapy is a special cancer treatment. It puts radioactive sources right into or near the tumor. This method gives more radiation to the tumor and less to healthy tissues.
There are many ways to put the radioactive sources in the body.
Techniques for Placing Brachytherapy Sources
Interstitial brachytherapy implants radioactive sources into the tumor. This is often used for prostate, breast, and gynecological cancers. Thin catheters, applicators, or needles are used. CT scans or ultrasounds guide them for accurate placement.
Intracavity brachytherapy involves placing sources in body cavities or surgery-created cavities. It is used for cervical, endometrial, and rectal cancers. Specialized applicators or balloons are used.
Episcleral brachytherapy is for eye cancers. It attaches radioactive sources to the eye’s surface.
Brachytherapy Technique | Description |
|---|---|
Interstitial Brachytherapy | Implanting radioactive sources directly into the tumor or cancerous tissue, often using catheters, applicators, or needles with imaging guidance. |
Intracavity Brachytherapy | Placing radioactive sources in a body cavity or a cavity created by surgery, such as the cervix, vagina, or rectum, using specialized applicators or balloons. |
Episcleral Brachytherapy | Attaching radioactive sources to the surface of the eye (the sclera) to deliver targeted radiation for eye cancers. |
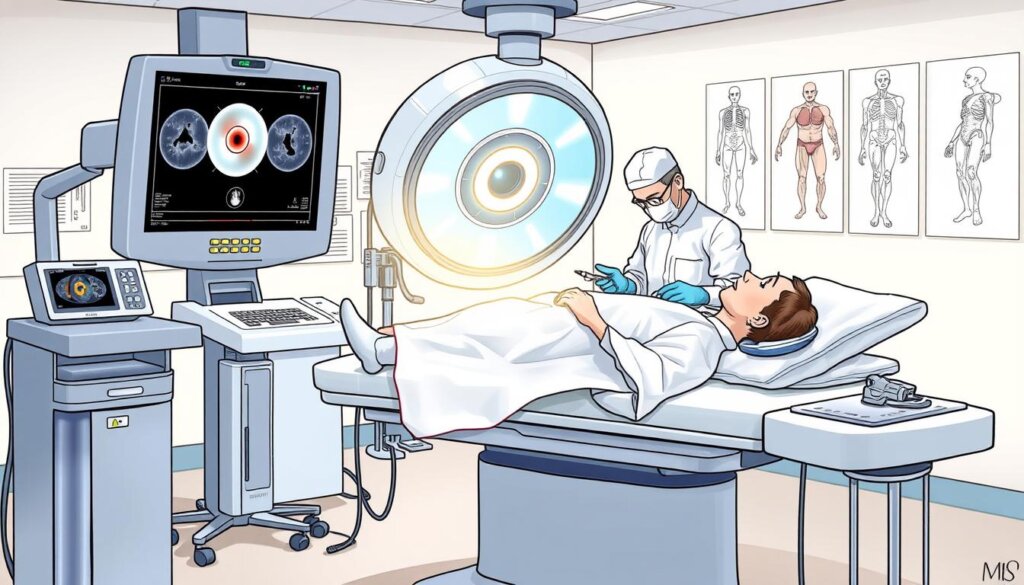
Brachytherapy procedures are carefully planned. They ensure the right placement of radioactive sources. The choice of technique depends on the cancer’s type, size, and location.
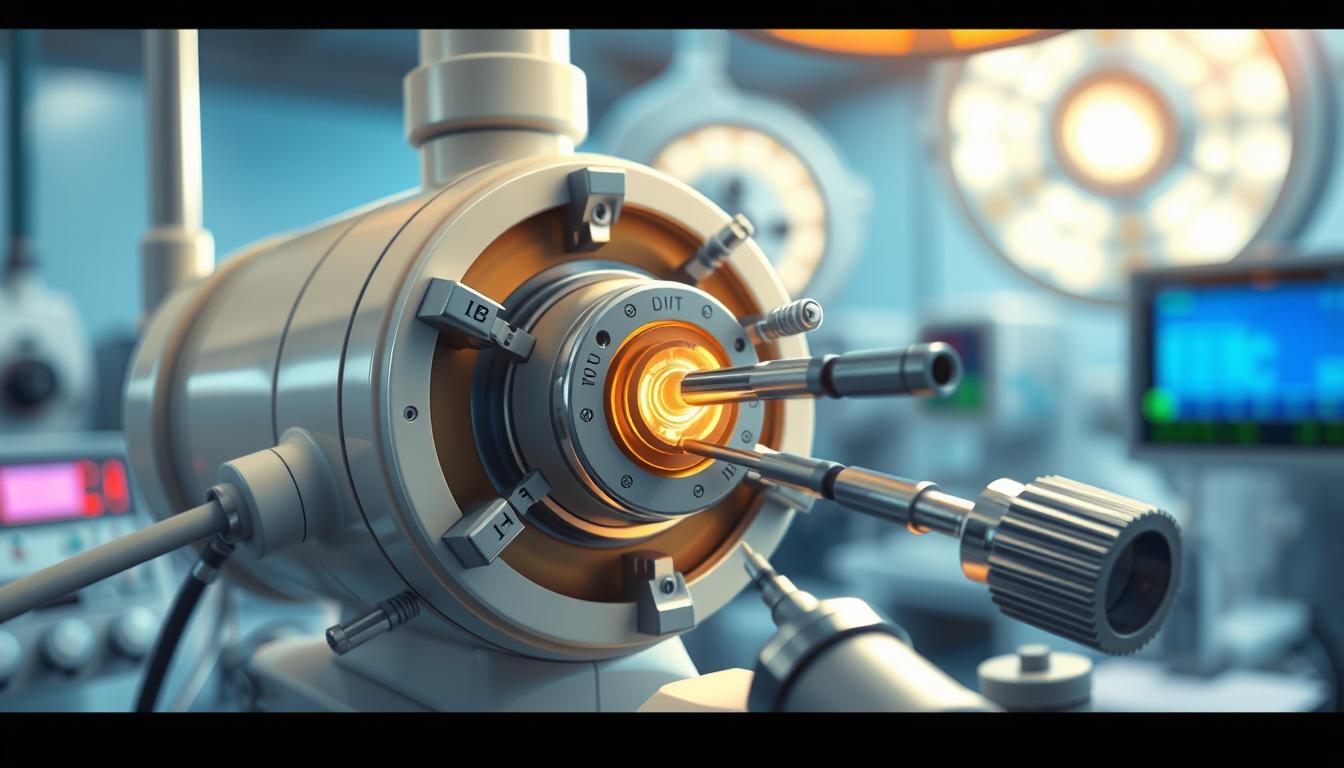
Brachytherapy Applicators and Equipment
Brachytherapy treatment requires special tools to deliver the radioactive sources to the cancer. These tools are key to safe and effective treatment.
Common Brachytherapy Applicators
Here are some common brachytherapy tools:
- Vaginal cylinders: Used for vaginal and cervical cancers.
- Tandem and ring/ovoid devices: For cervical and uterine cancers.
- “Y”-applicators: Used for rectal and anal cancers.
- Valencia applicators: Treats skin cancers, especially on the face.
- Breast brachytherapy applicators, like MammoSite and SAVI, for breast cancer.
- Plaque and sheet applicators: For ocular and superficial cancers.
- Interstitial needle templates: For precise radiation placement in tumors.
These tools help deliver brachytherapy safely and effectively. They make sure the right amount of radiation gets to the cancer, protecting healthy tissues.
Brachytherapy Applicator | Primary Use |
|---|---|
Vaginal Cylinder | Vaginal and cervical cancers |
Tandem and Ring/Ovoid | Cervical and uterine cancers |
“Y”-Applicator | Rectal and anal cancers |
Valencia Applicator | Skin cancers |
Breast Brachytherapy Applicators (e.g., MammoSite, SAVI) | Breast cancer |
Plaque and Sheet Applicators | Ocular and superficial cancers |
Interstitial Needle Templates | Precise placement of radiation sources |
These tools are made to ensure safe and effective radiation therapy. They are tailored for each patient and their cancer type. Research keeps improving brachytherapy technology, making treatments better and more effective.
Preparing for Brachytherapy
When you’re getting ready for brachytherapy, you’ll talk with a radiation oncologist. They will plan your treatment. You might get X-rays, MRI, or CT scans to figure out where to place the radioactive sources.
You’ll also have a physical exam and share your medical history. The doctor will explain the treatment, possible side effects, and what you need to do before starting.
Before brachytherapy, you might stop taking some medicines, like NSAIDs and vitamins. You should avoid certain medicines for 18 hours before. However, you should take Keflex and Flomax in the morning of the treatment.
You might need to do a bowel prep with laxatives and Miralax solution a few days before the procedure. This will ensure your bowels are empty for the procedure. The day before, you’ll only drink clear liquids and avoid solid food.
Brachytherapy patients often stop blood-thinning medicines like Advil and Aspirin before the treatment. Because of sedation, having a driver on the day of treatment is important.
After brachytherapy, you might feel tired, nauseous, or have diarrhea and pain. These symptoms usually last 1-2 weeks. You’ll have a follow-up in 4-6 weeks after the treatment ends.
If you have fever, pain, swelling, or diarrhea, call your doctor right away.
Knowing what to expect can make you feel more ready for brachytherapy.
“Proper preparation is key to ensuring a successful brachytherapy treatment and minimizing potential complications.”
What to Expect During Treatment
The experience during brachytherapy varies based on your treatment type. Temporary brachytherapy, or HDR brachytherapy, uses sources that are in and out quickly. You might get anesthesia and feel some pain, but no radiation stays in your body.
Temporary Brachytherapy Sessions
In temporary brachytherapy, a radioactive source is placed near the tumor. This method gives a strong dose of radiation to the cancer while protecting healthy tissues. Treatments are short, and you might need several over days or weeks.
Permanent Brachytherapy Implants
Permanent implants keep the radioactive sources inside you, with radiation levels dropping over time. You’ll need to avoid young kids and pregnant women until the radiation goes down. How long you stay in the hospital depends on your recovery.
Your healthcare team will give you all the details and instructions for safety and comfort.
“Brachytherapy can typically deliver a higher radiation dose than external beam radiation therapy, making it more effective at destroying cancer cells while sparing healthy tissue.”
Temporary Brachytherapy | Permanent Brachytherapy |
|---|---|
Radioactive sources inserted and removed in short sessions | Radioactive sources remain implanted in the body |
Sessions typically last a few minutes | Radiation gradually decreases over time |
May require anesthesia and cause some discomfort | May require safety precautions around others |
No radiation left in the body afterward | Length of hospital stay varies based on recovery |
Knowing what to expect in temporary brachytherapy sessions and permanent brachytherapy implants helps you prepare. This way, you can work well with your healthcare team for a good outcome.
Radiation Safety Precautions
Brachytherapy uses radioactive sources, which require safety steps to protect everyone. Patients in high-dose-rate (HDR) brachytherapy might stay in a private room. Healthcare workers may also need to wear protective gear or stand far away.
Patients with permanent implants should avoid young kids and pregnant women until the radiation goes down. The healthcare team will give clear instructions on safety for each patient.
Radiation therapy, including brachytherapy, has been around for over 100 years. It follows strict safety rules and checks. The ALARA principle helps keep radiation exposure low during cancer treatment.
External beam radiation therapy uses a beam aimed at the affected area. Internal radiation therapy (brachytherapy) uses a sealed source inside the body. Visitors need to stay in the hospital and limit contact during brachytherapy.
Brachytherapy treatments are safe. They use low-energy photons and keep radiation in the treatment area. The radioactive sources are tested, sealed, and placed carefully in the body. Patients might feel some side effects, like tenderness or swelling, but these usually go away in a few days.
Patients can receive effective cancer treatment safely by following safety precautions. This way, they can avoid risks from radiation exposure.
Brachytherapy Treatment for Different Cancers
Brachytherapy is a treatment for many cancers, like prostate, gynecological, breast, and eye cancers. The method and radiation sources used vary based on the cancer type and location. For example, prostate cancer often uses permanent seed implants. Gynecological cancers might get devices placed in the vagina or uterus.
Brachytherapy can be used alone or with other treatments, such as external beam radiation or surgery. Doctors at places like the University of Kansas Cancer Center have extensive experience with it. It can produce better results than other treatments for cancers like high-risk prostate cancer.
For prostate cancer, brachytherapy works well for low- and intermediate-risk patients. Almost all patients stay disease-free for five years, and over 92% for 10 years. In gynecologic cancers, brachytherapy is a key treatment for cervical cancer after external beam radiation. It’s also an option for uterine cancer patients who can’t have surgery.
Cancer Type | Brachytherapy Approach | Key Benefits |
|---|---|---|
Prostate Cancer | Permanent seed implants | – Highly effective for low- and intermediate-risk patients – Over 92% disease-free after 10 years |
Gynecological Cancers (Cervical, Uterine) | Intracavitary brachytherapy | – Standard treatment for cervical cancer after external beam radiation – Option for uterine cancer patients unable to undergo surgery |
Breast Cancer | Accelerated partial breast irradiation | – Targeted radiation to the tumor bed after lumpectomy – Reduces radiation exposure to healthy breast tissue |
Eye Cancer | Episcleral plaques | – Effective treatment for ocular melanoma and other eye cancers – Preserves the eye and vision in many cases |
Brachytherapy is a safe and effective cancer treatment. It delivers radiation precisely, reducing harm to nearby organs or healthy tissue. It can be done as an outpatient procedure, sometimes needing an overnight hospital stay. It uses either temporary high-dose-rate (HDR) or permanent low-dose-rate (LDR) approaches.
In summary, brachytherapy is a versatile treatment for many cancers. It offers targeted and effective therapy, and patients can greatly benefit from working with experienced brachytherapy providers.
Conclusion
Brachytherapy is a targeted cancer treatment that works well for many types of cancer. It sends radiation directly to the tumor, protecting healthy tissues nearby, which helps lower the chance of side effects.
This therapy is used for many cancers, like prostate and gynecological ones. Even though its use has changed, efforts are being made to make it more available again. This way, more patients can benefit from it.
Brachytherapy is getting better with new tools and methods. This means you and your doctor can choose the best treatment for you. Knowing about brachytherapy helps you be more involved in your care. It aims to give you the best results.
FAQ
What is brachytherapy?
Brachytherapy is a precise way to fight cancer. It uses radioactive material placed inside or near tumors. This method targets cancer from within.
How does brachytherapy work?
It uses radioactive sources, such as seeds or wires, placed in or near the tumor. These sources kill cancer cells while protecting healthy tissues.
What are the different types of brachytherapy?
There are three main types. Low-dose rate (LDR) uses sources that stay for 1 to 7 days. High-dose rate (HDR) delivers a high dose in short sessions. Permanent implants slowly decrease radiation over time.
How are the radioactive sources placed during brachytherapy?
Sources are placed using special techniques. These include putting them directly in the tumor or in body cavities and attaching them to the eye.
What kind of applicators and equipment are used for brachytherapy?
Many types of applicators are used. These include vaginal cylinders and devices for the cervix and breast. There are also special tools for the eye and skin.
How do I prepare for brachytherapy treatment?
You’ll have imaging tests like X-rays and CT scans, a physical exam, and a review of your medical history. The doctor will explain the treatment and any precautions.
What can I expect during brachytherapy treatment?
The experience varies by treatment type. Temporary treatments involve short sessions with sources inserted and removed. Permanent implants stay in the body, with radiation decreasing over time.
What safety precautions are needed for brachytherapy?
High-dose-rate treatments may require a private room. This is to protect others from radiation. Permanent implants need precautions around young children and pregnant women until radiation levels drop.
What types of cancer can be treated with brachytherapy?
Brachytherapy treats many cancers. This includes prostate, cervical, and breast cancer. The method and sources used vary by cancer type and location.