FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
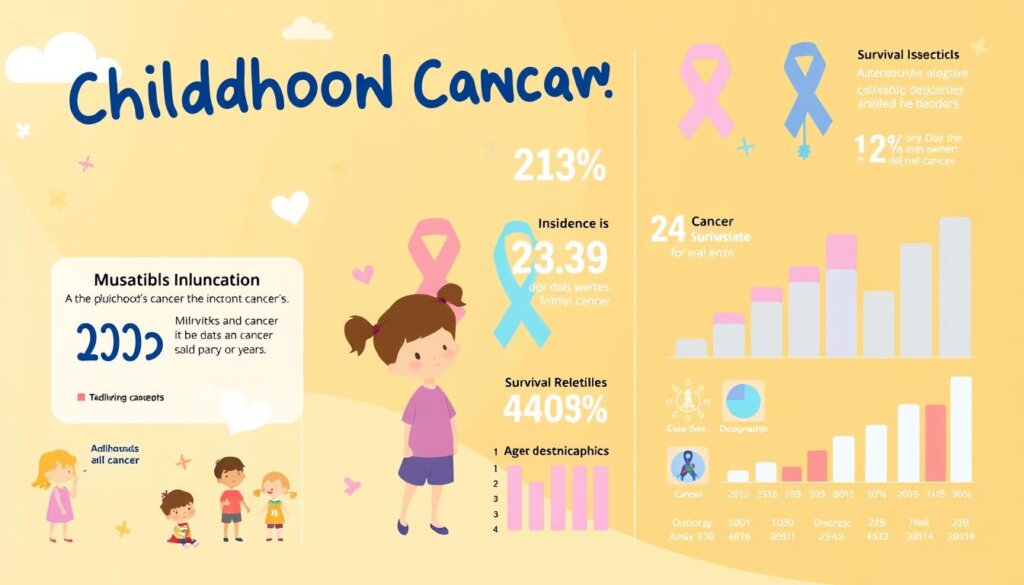
Did you know that over 80% of children with cancer in the United States survive for 5 years or more? This fact gives hope, but the journey is tough. Parents feel shocked and overwhelmed when their child gets cancer. It’s key to understand childhood cancer and support families well.
Children with cancer may see others who have lost their hair or are very sick during treatment, which can be difficult to witness. But, with age-appropriate info and open talks, parents can help their kids cope. Honest and calm talks build trust as you talk with your child and their siblings.
Key Takeaways
- Childhood cancer is a complex and challenging experience for families.
- Parents often feel shocked and overwhelmed after their child’s diagnosis.
- Open and honest communication with children is crucial for building trust and understanding.
- Children’s reactions to cancer can vary, and parents play a vital role in supporting them.
- Seeking support from healthcare professionals and the community is essential for families dealing with childhood cancer.
What is Childhood Cancer?
Causes and Types of Childhood Cancer
Cancer occurs when cells grow abnormally. It happens when cells become damaged or old and healthy cells can’t replace them.
Childhood cancers come from random gene changes, not from lifestyle or environment like adult cancers. There are over 100 kinds of childhood cancers. The exact type depends on how cells look and their genetic features.
The most common childhood cancers are leukemias, brain tumors, and lymphomas. Other types like neuroblastoma, Wilms tumor, and bone cancers also affect kids.
Type of Childhood Cancer | Description |
|---|---|
Leukemias | The most common childhood cancers include acute lymphocytic leukemia (ALL) and acute myeloid leukemia (AML). |
Brain and CNS Tumors | The second most common childhood cancers, with various types presenting different treatment approaches and outcomes. |
Lymphomas | Cancers start in lymphocytes, affecting the immune system and causing symptoms like weight loss, fever, fatigue, and swollen lymph nodes. |
Neuroblastoma | A cancer that primarily affects infants and young children, typically starting in the abdomen. |
Wilms Tumor | Also known as nephroblastoma, this cancer is more common in children aged 3 to 4 years and usually manifests as a swelling in the abdomen. |
Rhabdomyosarcoma | The most common type of soft tissue sarcoma in children, accounting for about 3% of childhood cancers. |
Retinoblastoma | A cancer of the eye, typically diagnosed in children around 2 years of age, is often identified by a white or pink appearance of the pupil. |
Primary Bone Cancers | Such as osteosarcoma and Ewing sarcoma are more prevalent in older children and teens, with distinct patterns of development and symptoms. |
Pediatric oncology is a special field for kids with cancer. Treatments include surgery, chemotherapy, and more. Clinical trials help find better treatments.
Hospitals for kids with cancer are part of the NCI-supported Children’s Oncology Group (COG). About 8 to 10 percent of childhood cancers are inherited. The National Cancer Institute (NCI) funds research on childhood cancers.

Symptoms and Diagnosis
Childhood cancer is rare but can show symptoms like common illnesses or injuries. The symptoms that need a specialist can differ by region. Some kids might get a cancer diagnosis during tests for other issues or after a sudden symptom.
Signs of childhood cancer include unexplained weight loss, fatigue, and paleness. Easy bruising or persistent pain in bones or joints are also signs. But these symptoms often mean something else, like an injury or infection.
Doctors will do a full check-up and tests like scans and biopsies if they suspect cancer. This helps find out what kind and how far along the cancer is.
In the UK, about 1,900 new cases of childhood cancer are diagnosed each year. The most common cancers in kids are leukemia, brain tumors, and lymphomas. Almost half of these cases happen in kids under 4.
General practitioners might see only one case every 20 years, and some might never see a case in their careers.

It’s important to spot early signs of childhood cancer and get medical help fast. Knowing the symptoms and how doctors diagnose helps parents and doctors work together. This ensures the best care for kids with this tough disease.
Cancer in Children
Statistics and Risk Factors
Childhood cancer is rare but a big killer in kids in the U.S. About 400,000 kids and teens get it every year. We don’t know what causes most cases, but some things might raise the risk. These include radiation, certain medicines, and genes passed down from family.
The top cancers in kids are leukemias, brain tumors, and lymphomas. About 10% of kids with cancer have a genetic reason for it. We should teach kids how to avoid cancer later in life.
In rich countries, over 80% of kids with cancer get better. But in poor countries, less than 30% do. Many kids in poor countries die because they can’t get the right care.
Palliative care helps kids with cancer feel better and live better lives. The World Health Organization wants 60% of kids with cancer to survive by 2030.
Statistic | Data |
|---|---|
Estimated number of children and adolescents aged 0-19 years who develop cancer each year | 400,000 |
Survival rate in high-income countries | More than 80% |
Survival rate in low- and middle-income countries | Less than 30% |
Percentage of low-income countries reporting cancer medicines generally available | 29% |
Percentage of high-income countries reporting cancer medicines generally available | 96% |
Percentage of children with cancer having a genetic predisposition | 10% |
“The World Health Organization strives to achieve at least 60% survival for all children with cancer by 2030, aiming to save an additional one million lives over the next decade.”
Treatment Options
Many treatment options are available for childhood cancer. Children’s cancers often respond well to chemotherapy because they grow fast. Their bodies can also handle more chemotherapy than adults.
But, radiation therapy can cause more harm in young children than in adults. Most kids get treated at special cancer centers. These centers are part of the Children’s Oncology Group (COG).
At these centers, kids often participate in clinical trials. These trials test new treatments and aim to improve cancer care for kids. Older kids must agree to join, with their parents’ help.
These centers have a team of experts, including doctors, nurses, and others. They all work together to help kids.
Childhood Cancer Treatment | Percentage |
|---|---|
Leukemia | Significant percentage |
Lymphoma | Prevalent type |
Brain and Spinal Cord Tumors | Second most common form |
Other Childhood Cancers | Neuroblastoma, osteosarcoma, Ewing sarcoma, rhabdomyosarcoma, retinoblastoma, Wilms tumor |
At UCLA Health, kids might get chemotherapy or other treatments. The Simms/Mann-UCLA Center also helps families.
In the U.S., over 10,000 kids get cancer each year. Leukemias and brain cancers are common. New treatments like CAR T cells are being tested.
However, treatments can have long-term effects. Children might face learning problems or heart issues, so it’s key to have plans for their long-term health.

Coping and Support
When a child gets cancer, it’s very hard for families. But, places that help kids with cancer offer many support services. These help kids and their families deal with the tough times.
Emotional and Practical Support for Families
These services help families find ways to cope. Childhood cancer prognosis shows continuous improvement with increasing chances of cure. But it still affects families deeply.
Grieving is a common response that affects children with cancer, parents, siblings, and family members. Parents need to learn about the disease and treatment. This helps them manage their feelings.
Support groups and resources available in hospitals are beneficial for coping with childhood cancer.
Children cope differently based on their age, and support services try to meet these needs. Practical coping strategies include keeping a journal, taking care of relationships, maintaining daily activities, and seeking help from support groups.
For school-aged children, parents need to offer repeated reassurance that the child is not responsible for the cancer and encourage communication. It’s also key to keep regular routines for siblings and offer comfort.
Teenagers with cancer need to know about emotional reactions and feel encouraged to share their feelings. They also need to know they’re not to blame for their illness.
About 80% of parents of children with cancer feel very emotionally distressed. But, 60% find it hard to ask for or accept help, even though they would benefit from emotional, practical, and financial assistance.
To help families, approximately 50% of parents of children with cancer engage in support groups, counseling services, or online communities to help manage the emotional challenges associated with their child’s diagnosis. Around 75% of parents of children with cancer rely on recreational activities and spending quality time together as a family to alleviate stress and create a sense of normalcy during treatment. And 45% seek spiritual or religious support to find comfort and strength during their child’s illness.
Pediatric cancer centers offer many emotional and practical support services. They aim to empower families and help them cope with the challenges of their child’s cancer journey.
Talking to Children about Cancer
When your child gets a cancer diagnosis, talking openly is key. Talking to kids about cancer can be tough, but it’s vital for their understanding and coping.
Begin by explaining cancer in simple terms that fit their age. Let them know they didn’t cause it and doctors are working hard to help. Tell them it’s okay to feel scared, sad, or angry.
- Give honest, simple info about cancer and treatment.
- Let them ask questions and share their feelings.
- Involve them in talks about the illness for better understanding and family bonding.
Talking about cancer doesn’t have to be done all at once. It’s a conversation that can grow as the situation changes. If you need help, talk to healthcare pros, therapists, or social workers.
“When parents include children in discussions about the illness, it can lead to a better understanding and emotional connection within the family.”
Make the conversation natural and safe for your child to open up. Being honest helps them feel informed, supported, and strong during their cancer fight.
For more help and tips, see the Cancer.org guide on talking to kids about cancer. It offers advice on talking to kids at every stage of cancer, from diagnosis to treatment.
Every family talks about cancer differently, but being open and supportive is key. Together, you can help your child face this tough time with kindness and strength.
Survivorship and Long-Term Care
Thanks to new cancer treatments, over 80% of kids with cancer in the U.S. live 5 years or more. But, many survivors face long-term physical, emotional, and brain effects from their treatment. It’s key to keep up with follow-up care to manage these effects and improve their life quality.
Follow-up care for kids with cancer starts about two years after treatment ends. Most survivors need yearly check-ups, but the schedule can change. The Children’s Oncology Group has rules for checking on survivors, starting two or more years after treatment.
Survivorship care can come from the original treatment team, a Long-Term Follow-Up Program, a local doctor, or a nurse practitioner. It’s important to keep up with care to handle late effects. Survivors need a treatment summary with all their health info.
Survivorship care helps patients stay healthy and do well at school and work. Teens and young adults with cancer had survival rates for the most deadly cancer types from 1975 to 2016. A study in the Netherlands looked at cancer trends in teens and young adults from 1990-2016.
A study in the Childhood Cancer Survivor Study found late deaths and health issues in long-term survivors. A study in Scandinavia found hospital visits for endocrine disorders in adults who had cancer as kids. The St Jude Lifetime Cohort Study looked at the health burden of surviving childhood cancer.
The Childhood Cancer Survivor Study found patterns in health issues in survivors of childhood cancer from 1970-1999. Survivors faced psychological issues, health quality, and brain function, showing life quality problems.
Studies showed survivors had psychological symptoms, social issues, and health behaviors, affecting their well-being. Adult survivors of childhood cancer had anxiety, showing the emotional toll.
Interventions were tested to help adolescent and young adult cancer survivors, like online therapy for depression. A review stressed the need for assessments and interventions to help with aftercare, health, and relationships.
Cancer Research and Advancements
Childhood cancer research has made big steps forward. We now know more about the genetic causes of cancer. Scientists are working on new treatments that are better and have fewer side effects for kids.
The Children’s Oncology Group (COG) is key in this effort. COG runs about 100 clinical trials at a time, studying new treatments and ways to improve current ones for childhood cancers.
About 20% of kids with cancer get their first treatment in a COG study. Around 57% of kids with Acute Lymphoblastic Leukemia (ALL) get their first care in a COG study.
However, some childhood cancers, like diffuse intrinsic pontine glioma (DIPG), have not seen better survival rates in 50 years. COG works with over 230 institutions worldwide. They provide specialized care for kids with cancer.
The Childhood Cancer Data Initiative (CCDI) is also important. CCDI works to gather data on childhood cancer. This helps research and leads to new discoveries.
CCDI’s Molecular Characterization Initiative analyzes genetic data. This helps tailor treatments to each child’s genetic profile.
Researchers have studied the genetics of childhood cancers extensively. In 2020, a global project examined them on a large scale. In 2018, they analyzed 1,699 pediatric cancers to better understand them.
Research and teamwork are key in fighting childhood cancer. By learning more about cancer and trying new treatments, we can help kids and their families.
Conclusion
Childhood cancer is tough, but we’re getting better at treating it. Thanks to new treatments and support for families, kids with cancer have a good chance of beating it. Over the years, more kids are surviving cancer and living long, healthy lives.
More than 85% of kids with cancer live for over 5 years after being diagnosed. We can keep making progress by spreading awareness and supporting research. This way, we help kids with cancer and their families.
Childhood cancer is a big problem for kids aged 1 to 4 and 5 to 14. We must keep working to understand and treat pediatric oncology. We aim to provide these brave kids and their families with the best care.
The fight against cancer in children is tough, but we’re making progress. Thanks to research and better cancer support, we can help more kids. Together, we can make sure every child with cancer gets to live a happy, fulfilling life.
FAQ
What is childhood cancer?
Cancer is when cells grow in a bad way. It happens when cells don’t follow the right signals. This makes cancer cells grow too much.
These cells can push out healthy ones. This makes it hard for the body to work right.
What are the common types of childhood cancers?
There are over 100 kinds of cancers in kids. The exact type depends on how cells look and their genetic features. The most common are leukemias, brain tumors, and lymphomas.
What are the causes of childhood cancer?
Childhood cancers come from random gene mutations. Lifestyle and environment don’t cause them like they do in adults.
What are the symptoms of childhood cancer?
Symptoms include losing weight without trying, feeling very tired, and looking pale. You might also bruise easily or have pain in bones or joints.
How is childhood cancer diagnosed?
Doctors use tests like blood tests, scans, and biopsies. These help find out the type and stage of cancer.
What are the statistics on childhood cancer?
Childhood cancer is rare but deadly. About 15,000 kids under 19 get cancer each year in the U.S.
What are the common treatments for childhood cancer?
Treatments include surgery, chemotherapy, and radiation. There’s also immunotherapy and targeted therapy to fight cancer.
How can families cope with a child’s cancer diagnosis?
Families need support when a child gets cancer. Parents might feel shocked and overwhelmed. It’s key to talk honestly and calmly with your child and siblings.
Take care of yourself, too. It’s not selfish. If you need help, reach out to your child’s team and family.
How should parents talk to their child about cancer?
Be honest and use simple words when talking about cancer. Answer your child’s questions and reassure them. Tell them the doctors are working to help.
Let your child express their feelings. Support them through this tough time.
What are the long-term effects of childhood cancer?
Survivors might experience physical, emotional, and cognitive effects. Ongoing care is key to managing these effects and improving their quality of life.
How is research advancing the treatment of childhood cancer?
Research is studying cancer’s genetic causes and cell features. This has improved diagnosis and treatment. New therapies, like targeted drugs and immunotherapies, are being explored.
Clinical trials offer new treatments and help advance pediatric oncology.