FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Imagine a young child, full of life and laughter, facing liver cancer. Sadly, about 250 kids in the U.S. each year get this diagnosis. Hepatoblastoma is the most common liver cancer in kids.
This rare cancer, making up 37% of all liver tumors in kids, mostly hits infants and toddlers. It often strikes between 6 months and 3 years old. These tumors start from early liver cells and come in two types: epithelial and mixed.
Key Takeaways
- Hepatoblastoma is the most common primary malignant liver tumor in children, affecting mostly those under the age of 3.
- It is a rare cancer, comprising about 1% of all childhood tumors.
- Hepatoblastomas are classified into two main types: epithelial and mixed epithelial-mesenchymal.
- Treatment has advanced significantly, with a current cure rate of around 70% through a combination of chemotherapy and surgical resection.
- Early detection and appropriate management are crucial for improving outcomes in children with hepatoblastoma.
What is Hepatoblastoma?
Overview and Prevalence
Hepatoblastoma is a rare liver cancer that mainly hits young kids. Most cases happen before they turn 3. It’s the top liver cancer in kids.
It’s getting more common in North America and Europe. Boys are slightly more likely to get it.
This cancer is rare, affecting only 2 to 3 million people. It mostly shows up in the first 18 months. Kids from infancy to 5 years old are mostly affected.
Boys are more likely to get it until they’re about 5.
About one-fifth of cases might need a liver transplant. It’s now 7.5 percent of all liver transplants in kids. But, up to 80 percent of kids can live over 20 years after a transplant.
Recurrences can happen in 16 percent of kids after a transplant. Most happen in the first two years.
Hepatoblastoma often spreads to the lungs. Surgery or chemotherapy can cure up to half of kids, even if it’s outside the liver. A study of 35 kids showed no difference in recurrences after a transplant.
In short, hepatoblastoma is a rare but serious cancer in young kids. It’s more common in boys. Thanks to better medical care, many kids can now survive and thrive after treatment.
Causes and Risk Factors
Though we don’t know the exact cause of hepatoblastoma, some genetic syndromes increase the risk. These include Beckwith-Wiedemann syndrome, familial adenomatous polyposis (FAP), trisomy 18, and Down syndrome. Other risk factors are prematurity, low birth weight, preeclampsia, and parental tobacco use before and during pregnancy.
Genetic mutations in the Wnt signaling pathway are common in hepatoblastoma. Very low birth weight is also a risk factor. Other factors include congenital abnormalities, paternal Hispanic ethnicity, maternal birthplace outside the US, and maternal Asian race.
Risk Factor | Adjusted Hazard Ratio (95% CI) |
|---|---|
Birth weight | 25.6 (7.70–85.0) |
Birth weight 1000–1999 g | 9.15 (3.09–27.1) |
Congenital abnormalities | 5.87 (1.88–18.3) |
Paternal Hispanic ethnicity | 4.18 (1.22–14.3) |
Maternal birthplace outside the US | 3.55 (1.51–8.32) |
Maternal Asian race | 3.86 (1.30–11.52) |
Preterm birth is linked to hepatoblastoma. Congenital abnormalities, especially omphalocele, raise the risk. The study found more congenital issues in hepatoblastoma cases.
“Hepatoblastoma is a very rare cancer that usually affects children less than 3 to 4 years of age.“
In summary, hepatoblastoma causes are not fully known. But, genetic syndromes, congenital issues, and perinatal factors are risk factors. Knowing these helps in early detection and treatment of hepatoblastoma.
Symptoms and Diagnosis
Signs and Tests
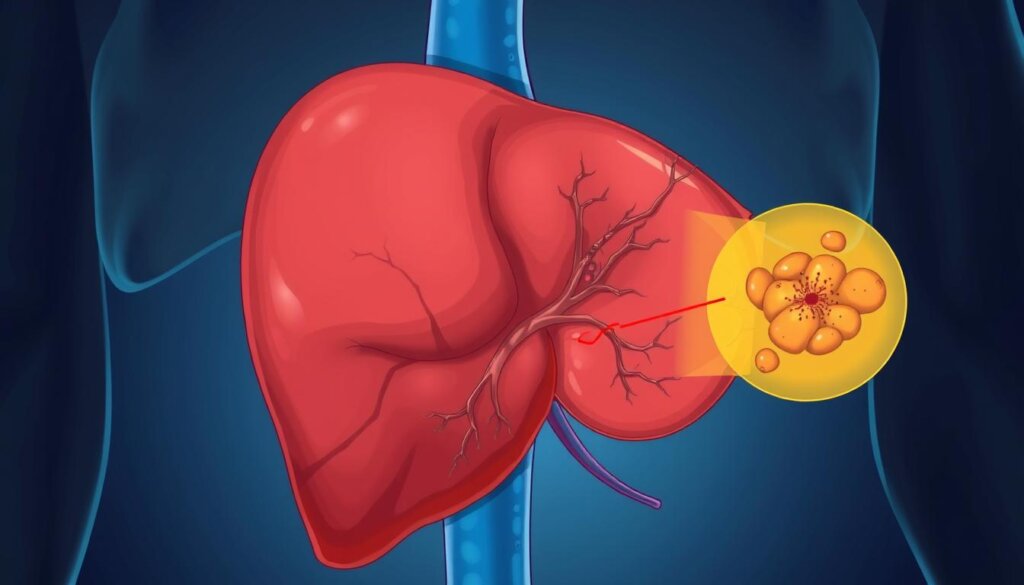
Hepatoblastoma is a rare liver cancer in kids. It shows up as a big, painless lump in the belly. Kids might also lose weight, not want to eat, or grow slowly.
About 90% of kids with this cancer have very high levels of alpha-fetoprotein (AFP) in their blood.
Doctors use ultrasound, CT scans, and MRI to see how big the tumor is and if it has spread. They might also take a biopsy to confirm the cancer and find out what type it is.
Diagnostic Test | Purpose |
|---|---|
Ultrasound | Evaluate the size and location of the tumor within the liver |
CT Scan | Assess the extent of the tumor and detect any metastases |
MRI | Provide detailed images of the tumor and surrounding structures |
Tumor Biopsy | Confirm the diagnosis and determine the histological subtype |
Finding and diagnosing hepatoblastoma early is key to treating it well. Doctors can make a good treatment plan by knowing the signs and doing the right tests.

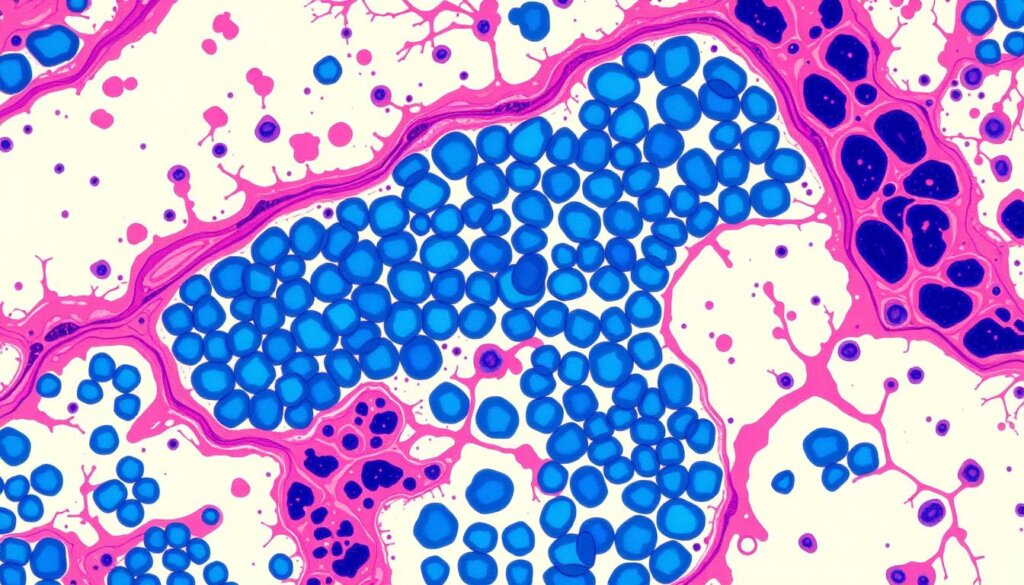
Histopathology and Subtypes
Hepatoblastoma is the most common liver cancer in kids. It happens mostly in the first 3 years of life. It makes up 90% of liver cancers in kids under 5.
The number of hepatoblastomas has gone up a lot in the last 30 years. This is because of early births, low birth weight, better survival rates, and better imaging.
Hepatoblastomas are mainly two types: epithelial and mixed. The epithelial type has subtypes like fetal, embryonal, macrotrabecular, and small cell undifferentiated. The mixed type has both epithelial and mesenchymal parts, like osteoid and spindle cells.
Testing for beta-catenin helps tell the subtypes apart. The fetal type shows beta-catenin on the cell membrane. The less differentiated types show it in the nucleus.
The fetal subtype has small cells and low cell division. The crowded fetal subtype has cells packed together and more cell division. A pleomorphic fetus has big, irregular nuclei and coarse chromatin. The embryonal subtype looks like solid nests or glands with dark cytoplasm.
The small-cell undifferentiated subtype has low AFP levels and is very aggressive. It looks like rhabdoid tumors with big nuclei and lots of filaments.
Hepatoblastoma Subtype | Histological Features |
|---|---|
Fetal (Well-differentiated) | Small, polygonal cells, low mitotic activity, clear to vacuolated cytoplasm |
Fetal (Crowded) | Closely packed cells, higher nucleus-to-cytoplasm ratio, increased mitotic activity |
Pleomorphic Fetal | Irregularly shaped nuclei, conspicuous nucleoli, coarse chromatin |
Embryonal | Solid nests or glandular structures, dark granular cytoplasm, enlarged nuclei |
Small-cell Undifferentiated | Discohesive, irregular nuclei, prominent nucleoli, abundant cytoplasmic filaments |
The International Pediatric Liver Tumors Consensus Classification helps standardize hepatoblastoma diagnosis.
“Immunohistochemical studies have been conducted to understand the clinicopathologic implication of hepatic progenitor cell marker expression in hepatoblastoma cases.”
Staging and Risk Stratification
Hepatoblastoma is a rare liver cancer in kids. It’s important to know its stage and risk to choose the right treatment. The Children’s Hepatic Tumors International Collaboration (CHIC) has a system for this.
The CHIC system looks at many things. It checks alpha-fetoprotein (AFP) levels, age, PRETEXT group if there are metastases and PRETEXT annotation factors. This helps doctors understand the disease better and plan treatments.
The PRETEXT group is key in treating hepatoblastoma. It shows how big the tumor is in the liver. The CHIC system has four risk groups: very low, low, intermediate, and high.
Risk Group | Characteristics |
|---|---|
Very Low | PRETEXT I/II, no metastases, AFP ≥100 ng/mL |
Low | PRETEXT III, no metastases, AFP ≥100 ng/mL |
Intermediate | PRETEXT IV, no metastases, AFP ≥100 ng/mL |
High | Metastatic disease, AFP |
The CHIC system helps doctors worldwide manage hepatoblastoma better. It lets them plan treatments based on each child’s risk. This way, they can help kids with this tough cancer more effectively.
Treatment and Management
Surgical Resection and Chemotherapy
The main treatment for hepatoblastoma, a rare liver cancer in kids, is surgery. About 60% of these cancers can’t be removed right away. So, neoadjuvant chemotherapy is used to make the tumor smaller.
If the tumor still can’t be removed, a liver transplant might be needed. This has been shown to help kids live longer. After surgery, more chemotherapy is given to kill any leftover cancer cells.
It’s very important to watch alpha-fetoprotein levels closely. This helps see if the treatment is working and if the cancer comes back. Some kids have special gene changes, like APC mutations, that doctors study.
Some families might have a condition called familial adenomatous polyposis. But most kids with hepatoblastoma don’t have this.
Doctors are looking into new ways to treat this cancer. They’re even using special viruses to fight it. They’re also looking at ways to stop the cancer from growing by blocking the hedgehog pathway.
They’re also studying how neoadjuvant chemotherapy helps in treating more advanced cases.
Research is ongoing to find better treatments for this rare cancer. The goal is to help kids live better lives.
“Surgical resection, either upfront or following neoadjuvant chemotherapy, is the mainstay of treatment for hepatoblastoma.”
Hepatoblastoma
Hepatoblastoma is a rare cancer in kids, mostly under 3 years old. This rare pediatric cancer starts from liver stem cells. It’s divided into two main types: epithelial and mixed.
Thanks to new treatments, more kids are being cured. Doctors use chemotherapy first, then surgery. This method works for about 70% of cases.
How well a child does depends on several things. These include how much tumor is left after surgery and the child’s age. Most cases are not caused by genetics, but some are.
Key Facts About Hepatoblastoma | Data |
|---|---|
Incidence in the U.S. | The incidence of hepatoblastoma has been increasing in the U.S. based on trends from 1992 to 2004. |
Prognosis for Fetal Histology | Surgical resection is reported as curative for children with hepatoblastoma with pure fetal histology. |
Risk-Adapted Treatment | Differentiated treatment protocols for high- and standard-risk hepatoblastoma have shown promising results. |
Chemotherapy and Surgery for High-Risk | A study on dose-dense cisplatin-based chemotherapy and surgery for high-risk hepatoblastoma demonstrated feasibility and success in children. |
Role of Liver Transplantation | The role of liver transplantation in managing unresectable hepatoblastoma in children has been highlighted in the literature. |
International Society of Paediatric Oncology Study | Risk-adapted treatment for childhood hepatoblastoma is addressed with final reports from the second study of the International Society of Paediatric Oncology. |
Chemotherapy Regimen Comparison | A comparison between different chemotherapy regimens for standard-risk hepatoblastoma has been conducted. |
Diagnostic Tool for Hepatic Tumors | INI1 immunohistochemistry is emphasized as an essential diagnostic tool for children with hepatic tumors and low alpha-fetoprotein levels. |
Hepatoblastoma is rare, affecting less than 1 in 1 million kids. But, if caught early, the cure rate is over 80%. For more advanced cases, survival rates are between 20% and 70% at 3-5 years.
Research is ongoing to improve treatment for this rare cancer. St. Jude Children’s Research Hospital is leading the way with clinical trials for liver cancer in kids and teens.
“The survival rate for hepatoblastoma is over 80% if the tumor is only in the liver and removable by surgery post-chemotherapy.”
As we learn more about hepatoblastoma, doctors and researchers keep working. They aim to give the best care to kids with pediatric liver cancer and their families.
Prognosis and Outcomes
The outlook for kids with hepatoblastoma, a rare liver cancer, has gotten much better. Now, about 70% of kids can be cured. This is thanks to a mix of chemotherapy and surgery.
Several things affect how well a child will do. These include how big the tumor is, how well the surgery went, the type of tumor, and the child’s age. Kids with smaller tumors and complete surgery do best. But, kids with big tumors or certain types of tumors face tougher challenges.
Prognostic Factor | Impact on Prognosis |
|---|---|
PRETEXT Group | Lower PRETEXT groups (I-II) have a better prognosis than higher groups (III-IV) |
Surgical Resection | Complete surgical resection is associated with improved survival rates |
Histological Subtype | Favorable subtypes (e.g., epithelial) have better prognosis than unfavorable subtypes (e.g., small cell undifferentiated) |
Age at Diagnosis | Younger children (under 3 years) generally have a better prognosis |
Even though more kids are surviving hepatoblastoma, scientists keep working. They want to make treatments even better for this tough cancer.
“The progress in managing hepatoblastoma has been remarkable, but there is still room for improvement, especially for patients with advanced or high-risk disease.”
Differential Diagnosis
When it comes to pediatric liver tumors, the differential diagnosis for hepatoblastoma includes several other conditions. Hepatocellular carcinoma (HCC) can look like the macrotrabecular subtype of hepatoblastoma. However, it usually affects older patients with risk factors like metabolic disorders or liver cirrhosis. Focal nodular hyperplasia and hepatic adenoma can also look like certain hepatoblastoma subtypes. But they are less common in young children.
Lymphoma and metastatic disease can also look like liver tumors in children. This makes it hard to tell them apart from hepatoblastoma. Knowing the unique features of these tumors is key for the right diagnosis and treatment.
Differential Diagnosis | Key Distinguishing Features |
|---|---|
Hepatocellular Carcinoma (HCC) | Typically affects the older patient population, associated with risk factors like metabolic disorders or liver cirrhosis. |
Focal Nodular Hyperplasia | Less common in young children, it can resemble certain hepatoblastoma subtypes. |
Hepatic Adenoma | Less common in young children, it can resemble certain hepatoblastoma subtypes. |
Lymphoma | It presents as a liver tumor in children and requires differentiation from hepatoblastoma. |
Metastatic Disease | It presents as a liver tumor in children and requires differentiation from hepatoblastoma. |
It’s very important to tell hepatoblastoma apart from other pediatric liver tumors for the right treatment. A careful look at the patient’s symptoms, imaging, and tissue samples is needed for the right diagnosis.
Research and Future Directions
Ongoing hepatoblastoma research is looking into new ways to treat this rare liver cancer in kids. Scientists are testing targeted therapies and improving chemotherapy to make treatments better. They also want to make staging and risk plans more personal for each child.
Genetics and the molecular causes of hepatoblastoma, like the Wnt/beta-catenin pathway, are being studied. This research aims to find new ways to fight cancer by targeting its causes.
Ongoing Studies and Advancements
New studies are using cool tech to manage hepatoblastoma. For example, 3D printing helps doctors plan surgeries and teach patients. Also, 3D software is helping with complex liver surgeries. The ALPPS procedure is also showing promise for treating liver tumors in kids.
Liver transplants are proving to be very effective for kids with big tumors that can’t be removed. Studies on liver transplants for these tumors have shown good results. Robotic surgery is also being used more for kids’ tumors, with many successes. A case report showed how ex vivo liver resection and autotransplantation with cardiopulmonary bypass worked for a child with hepatoblastoma.
As we learn more about hepatoblastoma, researchers are working hard to find new treatments. Their work is key to improving care and outcomes for kids with this rare cancer.
Statistical Data | Reference |
|---|---|
A systematic review highlighted the utility of three-dimensional printing for preoperative assessment of children with extra‐cranial solid tumors. | |
A study focused on using three‐dimensional printed liver models for patient education showed impact in patient understanding. | |
A research article discussed the usefulness of three‐dimensional (3D) simulation software in hepatectomy for pediatric hepatoblastoma. | |
Research on ALPPS (Associating Liver Partition with Portal Vein Ligation for Staged Hepatectomy) indicated its effectiveness in the treatment of liver tumors in children. | |
Liver transplantation has shown to be highly effective in children with irresectable hepatoblastoma. | |
Long-term outcomes following liver transplantation for primary hepatic tumors have been studied over a period of 40 years. | |
Robotic-assisted surgery for pediatric tumors has become an emerging trend, with numerous successful cases reported in pediatric oncology. | |
A case report detailed the successful use of ex vivo liver resection and autotransplantation with cardiopulmonary bypass for hepatoblastoma in children. |
Hepatoblastoma is the most common liver cancer in kids. Most cases happen before a child is four years old. Thanks to better treatments and surgery, survival rates have improved a lot.
Removing the tumor completely is key to curing hepatoblastoma. In the U.S., removing tumors early is standard for some cases. For others, chemotherapy comes first. Doctors use a system called PRETEXT to plan surgeries, from small cuts to removing the whole liver.
For the best results, following a treatment plan is important. Trying to reduce side effects from treatments and surgeries is also crucial. Kids with big tumors might do better at centers that specialize in complex surgeries. But, deciding where to get care can be tough because of limited data.
“The ongoing research and advancements in the field of pediatric hepatoblastoma are essential in improving the care and outcomes for these young patients. By exploring innovative treatment approaches and refining our understanding of the disease, we can strive to provide more effective and personalized care, ultimately giving these children the best chance at a brighter future.”
Conclusion
Hepatoblastoma is a common liver tumor in kids. It makes up just over 1% of all childhood cancers. Even though it’s rare, with about 100 cases a year, we’ve made big steps in treating it. Now, a mix of chemotherapy and surgery can cure about 70% of cases.
Researchers are working hard to make treatments even better. They want to understand the disease better and help more kids. Finding genes like CTNNB1 and TERT helps doctors create better treatments. This means kids with hepatoblastoma can get better care and have a brighter future.
Even though hepatoblastoma is rare and tough, we’re making progress. Advances in hepatoblastoma overview and pediatric liver cancer management give hope to kids and their families. By supporting research, we can beat this disease and help more kids live happy, healthy lives.
FAQ
What is hepatoblastoma?
Hepatoblastoma is a rare liver cancer in kids. It mostly hits children under 3. It’s a big deal, making up about 1% of all childhood cancers.
What are the causes and risk factors for hepatoblastoma?
We don’t always know why it happens. However, some genetic issues raise the risk. These include Beckwith-Wiedemann syndrome and Down syndrome.
Other risks are being born too early, being underweight, and having parents who smoke.
What are the symptoms and diagnostic tests for hepatoblastoma?
Kids with it often have a big, painless belly bump. Their blood tests show high levels of alpha-fetoprotein (AFP). Doctors use ultrasound and MRI to see how big the tumor is.
How are hepatoblastomas classified and staged?
Doctors sort them into two types: epithelial and mixed. The Children’s Hepatic Tumors International Collaboration (CHIC) has a system to rate them. It looks at AFP levels, age, and how big the tumor is.
What are the treatment options for hepatoblastoma?
Surgery is key, but sometimes they need chemotherapy first. About 60% of cases start too big to remove right away. Chemotherapy tries to make it smaller.
If that doesn’t work, a liver transplant might be an option.
What is the prognosis for children with hepatoblastoma?
Thanks to better treatments, more kids are getting better. Now, about 70% can be cured. The chance of getting better depends on the tumor size and how well it’s removed.
What is the differential diagnosis for hepatoblastoma?
Other liver cancers in kids can look like hepatoblastoma. These include HCC and lymphoma. Doctors have to check carefully to tell them apart.
What are the recent advancements and future directions in hepatoblastoma research?
Scientists are looking at new ways to treat it. They’re testing targeted therapies and improving chemotherapy. They also want to understand the cancer better to find new treatments.