FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
Coronary artery disease (CAD) is a big health problem in the U.S. It affects about one in every 20 people. In 2021, it caused 375,476 deaths, with 20% of those being people under 65. It’s a top cause of death in the country. So, it’s important to know about its causes, symptoms, and treatments.
CAD happens when plaque builds up in the arteries that bring blood and oxygen to the heart. This makes the arteries narrow and hard. It can cause chest pain, shortness of breath, and even a heart attack. Knowing the risk factors and managing it is key to keeping your heart healthy and easing the load on healthcare.
Key Takeaways
- Coronary artery disease (CAD) is the most common type of heart disease, affecting an estimated 18.2 million American adults.
- CAD is caused by the buildup of plaque in the arteries that supply blood and oxygen to the heart, leading to narrowing and hardening of the arteries.
- CAD is a leading cause of death in the U.S., responsible for 375,476 deaths in 2021, with 20% occurring in individuals younger than 65.
- Certain ethnic groups, such as Black, Hispanic, and Southeast Asian individuals, are more likely to be diagnosed with CAD and have higher mortality rates.
- Proactive management of CAD through lifestyle changes, medications, and medical procedures can help reduce the risk of complications and improve outcomes.
What is Coronary Artery Disease?
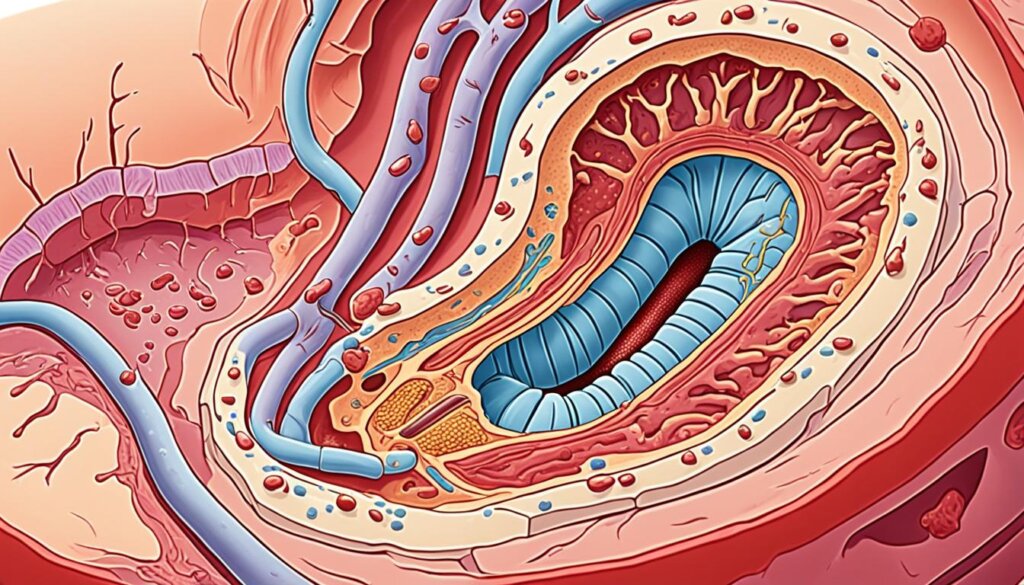
Coronary artery disease (CAD) is a serious heart condition that affects millions of Americans. It happens when the arteries that supply the heart with blood and oxygen get damaged or diseased. This is often due to a buildup of cholesterol plaques in the arteries. This process, called atherosclerosis, can make the arteries narrow and hard, reducing blood flow to the heart.
As the plaque buildup gets worse, it can make it hard for the heart to pump blood throughout the body. This increases the risk of chest pain, heart attack, and other heart problems.
Definition and Overview
CAD is the most common heart disease in the U.S., affecting over 18 million adults. It develops slowly, often without symptoms until it’s noticed. Factors that increase the risk include aging, being male, health conditions like high blood pressure and diabetes, and lifestyle choices like smoking and being overweight.
Atherosclerosis and Plaque Buildup
The main cause of CAD is atherosclerosis, where cholesterol plaques build up in arteries. These plaques can harden and narrow the arteries, reducing blood flow to the heart. This can cause symptoms like chest pain, shortness of breath, and fatigue.
To diagnose CAD, doctors use tests like an ECG, echocardiogram, and cardiac catheterization. Treatment may include lifestyle changes, medicines, and sometimes surgery like angioplasty.
“Coronary artery disease is a serious condition that can have life-threatening consequences if left untreated. However, with early detection and proper management, many individuals with CAD can lead healthy, active lives.”
Who is at Risk for Coronary Artery Disease?
Coronary artery disease (CAD) is the most common heart disease in the U.S.. It can happen to anyone, but some things make you more likely to get it. Knowing these risks helps you take steps to keep your heart healthy.
Age and Gender
Getting older increases your chance of CAD. This risk goes up after 45 for men and 55 for women. Men and those assigned male at birth face a higher risk than women and those assigned female at birth.
Existing Health Conditions
Some health issues can lead to CAD. These include high blood pressure, high cholesterol, diabetes, and atherosclerosis (artery plaque buildup). People with conditions like systemic lupus erythematosus, rheumatoid arthritis, and HIV also face a higher CAD risk.
Lifestyle Factors
Your daily choices affect your CAD risk. Being overweight, inactive, eating poorly, and smoking can up your risk. On the other hand, regular exercise and a healthy diet can lower your risk.
Family History
If a family member got heart disease young (50 or younger), your CAD risk might be higher. This points to a genetic risk that can be passed down.
Knowing the risks for CAD helps you watch your heart health and change your lifestyle. Regular doctor visits and a healthy lifestyle are key to a strong heart.
Symptoms of Coronary Artery Disease
Coronary artery disease (CAD) is the most common heart disease in the U.S. It can be silent or show signs that CAD is there.
Chest Pain (Angina)
The most common CAD symptom is chest pain, or angina. This pain feels like pressure or tightness in the chest or left side. It can spread to shoulders, arms, back, neck, or jaw. It often happens with exercise or stress and goes away with rest.
Shortness of Breath and Fatigue
Shortness of breath is another CAD symptom, especially with exercise. People may feel tired and lack energy for simple tasks.
Heart Attack Symptoms
In severe cases, CAD can cause a heart attack. Symptoms include crushing chest pain, pain in shoulders or arms, shortness of breath, and sweating. But, many heart attacks have little to no symptoms. It’s key to get medical help for any chest or heart concerns.
Women may have different heart attack symptoms than men, like anxiety, back pain, and nausea. Women’s CAD symptoms can also include back pain, jaw discomfort, and shortness of breath.
Getting medical help quickly for symptoms is very important. Early treatment can make a big difference for CAD patients.
Diagnosing Coronary Artery Disease
Your doctor starts by looking at your medical history and doing a physical check-up. They want to know about your symptoms, heart disease risks, and family heart history.
Medical History and Physical Exam
Your doctor will ask about your symptoms like chest pain or shortness of breath. They’ll check your health, including your blood pressure and heart rate. This helps them see if you might have CAD.
Diagnostic Tests
If your doctor thinks you might have CAD, they’ll order tests. These include an EKG to check your heart’s electrical activity, stress tests to see how your heart acts when you’re active, and imaging tests like CT scans or angiograms to see the coronary arteries.
Blood tests might also be done to look for signs of heart disease, like high cholesterol or inflammation. Programs for women’s heart health can help diagnose and treat CAD in women, as women’s symptoms can be different.
These tests help your doctors figure out if you have CAD and how bad it is. They use this info to make a treatment plan just for you.
Treatment Options for Coronary Artery Disease
Treating coronary artery disease (CAD) often means making changes in lifestyle and using medicine. The main goals are to ease symptoms, prevent more problems, and make the heart healthier.
Lifestyle Changes
Healthy choices are key in managing CAD. Eating foods like fruits, veggies, whole grains, and lean meats is good. Also, staying active is important. Quitting smoking is key, as it cuts down the risk of more heart attacks quickly. Stress-reducing activities like meditation or yoga can also boost heart health.
Medications
Doctors often prescribe medicines to tackle CAD. These can include aspirin to stop blood clots, drugs to lower cholesterol, beta-blockers for blood pressure, and ACE inhibitors for better blood flow. It’s vital for patients to work with their doctors to find the right medicines for them.
Procedures and Surgeries
For severe CAD, doctors might suggest procedures or surgery. Coronary angioplasty uses a balloon to open blocked arteries. Coronary artery bypass surgery uses another artery or vein to bypass the blocked part of a coronary artery. These are usually for people with serious or complex CAD.
Cardiac rehab programs are also key for CAD patients. They offer exercise, education, and counseling to help patients live healthier and manage their condition better.
“Treating coronary artery disease requires a comprehensive approach that addresses the underlying causes and risk factors. By combining lifestyle changes, medications, and, in some cases, medical procedures, patients can effectively manage their condition and improve their overall heart health.”
Dealing with coronary artery disease is a growing field, with new research and treatments. By working with their doctors, patients can get a treatment plan that fits their needs and helps them get the best results.
Coronary Artery Disease and Mental Health
Getting a diagnosis of coronary artery disease (CAD) can really affect someone’s mental health. People with CAD often feel more anxious and depressed. They worry about their symptoms, how the disease might get worse, and the risk of a heart attack. This worry can make their physical symptoms worse, creating a cycle of poor mental and physical health.
The link between CAD and mental health is complex. Studies show that mental health issues like depression and bipolar disorder can make CAD worse, especially in young people. Anxiety can also lead to high blood pressure and increase the risk of heart disease.
It’s important for people with CAD to focus on their mental health. They should talk to mental health experts, join support groups, and work with their healthcare team. Stress management, therapy, and cardiac rehab can help manage the mental side of CAD.
Healthcare providers need to pay attention to the mental health of CAD patients. This approach can lead to better health outcomes and a better quality of life for those with CAD.
“The connection between coronary artery disease and mental health is a critical area of focus for healthcare professionals. By addressing the emotional well-being of patients, we can significantly improve their overall health outcomes and quality of life.”
When to Seek Medical Attention
Regular check-ups and follow-ups are key for those with coronary artery disease. Seeing doctors regularly helps track the disease and manage it well. If you have chest pain, trouble breathing, or pain in your arms or jaw, get help fast. Calling 911 quickly can save a life in an emergency.
Regular Check-ups and Follow-ups
It’s important to keep up with regular doctor visits if you have coronary artery disease. These visits help watch the disease, change treatments, and spot problems early. By staying on top of health, patients can manage their disease better and lower the risk of more problems.
Emergency Situations
If you see signs of a heart attack, get help right away. Look out for chest pain, trouble breathing, and pain in your arms or jaw. Calling 911 fast can help save your life and lessen heart damage. Don’t wait to get emergency care, as quick action is key for treating a heart attack.
Symptom | Description |
|---|---|
Chest Pain (Angina) | A feeling of pressure, tightness, or discomfort in the chest, which may radiate to the arms, neck, or jaw. Angina is often triggered by physical activity or emotional stress. |
Shortness of Breath | Difficulty breathing, especially during physical activity or when lying down, can be a sign of coronary artery disease. |
Heart Attack Symptoms | Sudden chest pain, shortness of breath, sweating, nausea, or dizziness can indicate a heart attack and require immediate medical attention. |
“Seeking medical attention promptly is crucial for individuals with coronary artery disease, as it can mean the difference between life and death in an emergency situation.”
Questions to Ask Your Doctor
Talking about coronary artery disease with your doctor is key. You need to know about your condition, risks, and treatment options. Here are some important questions to ask:
- What are my specific risk factors for coronary artery disease?
- What lifestyle changes can I make to lower my risk of developing coronary artery disease?
- What medications would be most effective in managing my condition, and what are the potential side effects?
- Will I need any procedures or surgeries, and what does the recovery process involve?
- Are there any support groups or resources you can recommend to help me manage my coronary artery disease?
Asking these questions helps you work with your doctor to make a good treatment plan. This ensures you get the best care for your coronary artery disease.
Women might face special risk factors with coronary artery disease. These include pregnancy, birth control, and menopause effects. It’s vital to talk about these with your doctor.
Regular risk assessments and tests can spot and track coronary artery disease. This leads to early action and tailored treatments. By working with your doctor and asking the right questions, you can help manage your heart health.
“Understanding your individual risk factors and being proactive about your heart health is crucial for managing coronary artery disease.” – Dr. Sarah Johnson, Cardiologist
Risk Factors for Coronary Artery Disease
Coronary artery disease (CAD) is a big health worry that can be very serious if not handled. Knowing the risks is key to stopping it early. Recent studies have found many important factors that raise the risk of CAD.
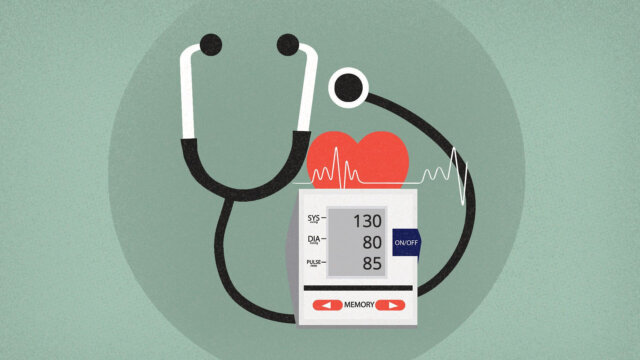
Smoking is a big risk for heart disease. High blood pressure and high cholesterol make the heart work too hard and cause fat to build up in arteries. Diabetes, being overweight, and not moving enough also make the risk higher.
- Smoking greatly increases the risk of heart disease.
- High blood pressure strains the heart and can cause heart disease.
- High cholesterol in the blood can lead to heart disease.
- High lipoprotein (a) is a risk factor for heart disease and hardening of the arteries.
- Not exercising can cause fat to build up in arteries, raising the risk of heart attack or stroke.
- Diabetes can greatly increase the risk of heart disease because of high blood sugar making blood thick.
- Thrombosis, a blood clot, can cause a heart attack if it blocks a coronary artery.
Family history and age also play a big part in CAD. If someone close has had heart disease young, you might be at higher risk. After 65, the risk of CAD goes up.
To lower CAD risk, changing your lifestyle is key. Quit smoking, eat well, exercise, and manage health conditions. Taking steps to reduce risks can greatly improve heart health and lower CAD chances.
In conclusion, knowing and dealing with CAD risks is key to a healthy heart. Regular check-ups, a healthy life, and managing health conditions are important. They help prevent and manage this serious condition.
Coronary Artery Disease in Women
Coronary artery disease (CAD) is the top cause of death for both women and men in the U.S.. Women often show different symptoms than men, like shortness of breath, extreme tiredness, nausea, and pain in the back or jaw, not just chest pain. They face a higher risk of CAD after menopause.
Pregnancy issues, hormonal birth control, and early menopause can raise a woman’s CAD risk. Women often have blockages in smaller arteries too, which supply blood to the heart. It’s key to know these differences for the correct diagnosis and treatment of CAD in women.
Studies reveal women are less likely to get aspirin and statins to prevent heart attacks than men. They’re also less likely to go to cardiac rehab and have bypass surgery. This shows healthcare providers must pay more attention to women’s CAD needs.

Having a family history of heart disease, inflammatory conditions like rheumatoid arthritis or lupus, and low estrogen after menopause can up a woman’s CAD risk. Knowing these differences helps doctors improve how they diagnose, treat, and manage CAD in women. This can lessen the impact of this serious condition.
Racial and Ethnic Disparities in Coronary Artery Disease
Coronary artery disease (CAD) affects different groups in the U.S. in big ways. Black, Hispanic, and American Indian people often get CAD more and face worse outcomes, like a higher chance of dying, than whites.
Many things cause these differences, like not having good healthcare, being poor, and having more risk factors like high blood pressure and diabetes. In 2017, black people were more than twice as likely to die from heart disease as Asian or Pacific Islander people.
Heart disease was more common in 2017 among non-Hispanic whites, blacks, Hispanics, and Asians. Non-Hispanic black adults had an 11.5% chance of having heart disease. High blood pressure was most common in 2015-2016 among non-Hispanic blacks over 20 years old at 46.9%.
Black and Hispanic adults over 20 were most likely to be obese and have diabetes. High cholesterol was found equally in 2015-2016 among Hispanic, white, black, and Asian adults over 20.
Racial/Ethnic Group | Prevalence of Cardiovascular Disease | Prevalence of Diabetes | Prevalence of Hypertension |
|---|---|---|---|
Non-Hispanic Black | 47% | 1 in 4 | 59% |
Non-Hispanic White | 36% | 1 in 12 | N/A |
Hispanic | N/A | More than twice as likely as white women | N/A |
American Indian | N/A | Three times more likely than whites | N/A |
Black women are twice as likely as white women to get chronic high blood pressure during pregnancy. Black adults often have more damage from high blood pressure and are four times more likely to have kidney disease at its worst.
Black adults are more likely to die from high blood pressure and related diseases. They are also more likely to be in the hospital for heart failure and to be readmitted within 90 days. Black women have a 70% higher risk of heart failure than white women.
Black adults are more likely to be hospitalized for heart failure, stroke, and die from heart attacks.
We need to work on these issues with better healthcare and focusing on the social factors that affect health. This will help reduce the big burden of heart disease on minority groups.
Diagnostic Tests for Coronary Artery Disease
Doctors use many tests to find coronary artery disease (CAD). These tests check for blockages or narrowings in the heart’s arteries. They help decide on the best treatment.
Electrocardiogram (EKG)
An EKG is a simple test that shows the heart’s electrical activity. It looks for heart muscle damage. This could mean CAD is present.
Stress Tests
Stress tests see how the heart acts when you’re active. They check blood flow to the heart during exercise. This can show CAD signs.
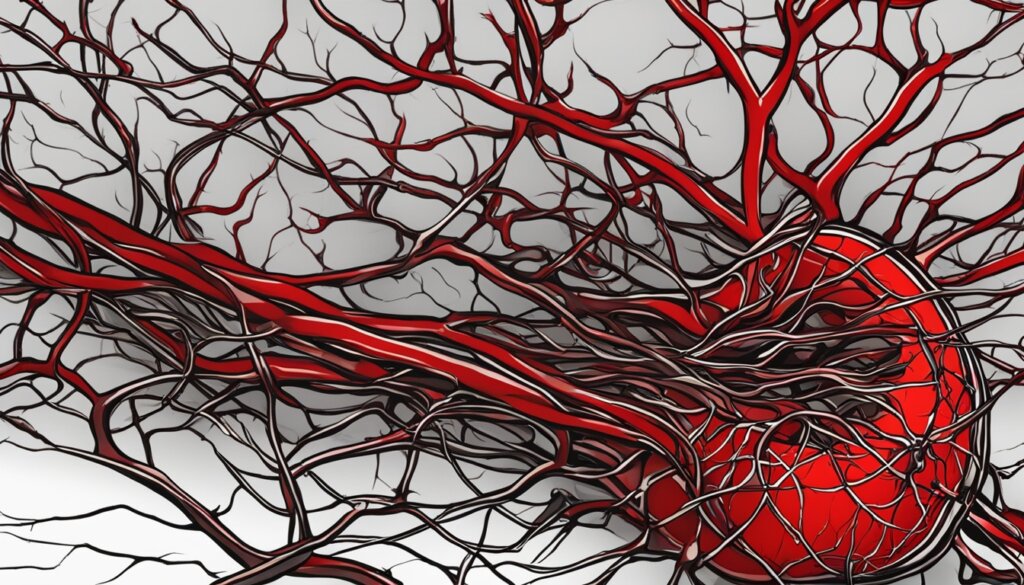
Cardiac Catheterization and Angiogram
Cardiac catheterization and angiography use a thin tube to inject dye and take X-rays. This shows blockages or narrowings in the heart arteries. It helps doctors make a clear CAD diagnosis.
Tests like EKG, stress tests, and imaging help doctors find CAD. They see how serious it is. New research makes these tests better. This helps in treating CAD better
“Accurate diagnosis and risk assessment are crucial for the effective management of coronary artery disease, as they guide healthcare providers in developing the most appropriate treatment plan for each individual patient.”
Home Monitoring for Heart Health
Checking your heart health at home is key, even with medical tests. By doing self-checks and tracking your health, you can learn a lot. This helps you talk to doctors early.
Checking your pulse is easy and useful. It shows your heart rate, which tells you about your heart health. Also, using a home blood pressure cuff can spot issues early.
The stair test is another simple way to check your heart. Climb four flights of stairs in 90 seconds to see how your heart is doing.
Keep track of your health over time. If you notice changes or patterns, talk to your doctor. Signs like sudden weight gain or fluid buildup mean you should call your doctor.
New tech like telemonitoring helps send your health info to doctors from home. By being proactive, you can catch problems early with your doctors’ help.
Groups like the American Heart Association give great advice on heart health. They talk about lifestyle changes and regular checks.
By monitoring your heart health at home, you take charge of your health. You can make smart choices and work with your doctors for better heart health.
Conclusion
Coronary artery disease (CAD) is a big health issue that affects many in the U.S.. In 2018, 16.5 million people over 20 had CAD, with 55% being men. Worldwide, it led to about nine million deaths in 2016. Experts think it will keep getting worse, mainly in poor countries.
But, we can fight this disease. Knowing the risks like age, gender, family history, and habits like smoking and being overweight helps us act early. There are also rules to prevent CAD and lower heart disease deaths.
By changing our ways, taking medicine, and sometimes getting medical help, many with CAD can live well. It’s important to stay informed, get regular check-ups, and speak up for our health. This helps us handle CAD, a common but treatable heart condition.
FAQ
What is coronary artery disease (CAD)?
Coronary artery disease is when the arteries that supply blood to the heart get damaged. This happens because of a buildup of cholesterol plaques. These plaques make the arteries narrow and hard, reducing blood flow to the heart.
Who is at risk for developing coronary artery disease?
People at risk include those getting older, men, and those with health issues like high blood pressure and diabetes. Smoking, being inactive, and having a family history of heart disease also increase risk.
What are the most common symptoms of coronary artery disease?
Common symptoms include chest pain or discomfort, known as angina. This can feel like pressure or burning in the chest or left side. It might spread to the shoulders, arms, back, neck, or jaw. Shortness of breath and feeling very tired are also symptoms.
How is coronary artery disease diagnosed?
Doctors start by reviewing your health history and doing a physical exam. They might order tests like an electrocardiogram (EKG), stress tests, and imaging tests. These help check the heart’s activity, how it handles exercise, and see the arteries.
What are the treatment options for coronary artery disease?
The treatment combines lifestyle changes and medical help. You might eat healthier, exercise more, quit smoking, and manage stress. Doctors may prescribe drugs to lower cholesterol and blood pressure. For severe cases, procedures like angioplasty or bypass surgery might be needed.
How does coronary artery disease affect mental health?
Getting diagnosed with CAD can be tough and affect your mental health. Many feel more anxious and depressed. They worry about symptoms, the disease getting worse, and heart attacks. Talking to mental health experts and joining cardiac rehab can help.
When should I seek medical attention for coronary artery disease?
Get help right away if you have chest pain, shortness of breath, or pain in the arms or jaw. Keep up with regular doctor visits to watch your condition and manage it well.
What questions should I ask my doctor about coronary artery disease?
Ask your doctor about your risk factors, how to lower them, and the best treatments. Know about potential side effects of medications. Ask about procedures, recovery, and support groups for CAD.
What are the differences in how coronary artery disease presents and is experienced by women?
Women often have different symptoms like shortness of breath, extreme tiredness, nausea, and back or jaw pain. They’re at higher risk after menopause and from pregnancy and birth control use.
How do racial and ethnic disparities affect the burden of coronary artery disease?
CAD hits harder on Black, Hispanic, and American Indian people in the U.S. They face worse health outcomes and higher death rates than whites. This is due to less access to healthcare, lower socioeconomic status, and systemic racism.