FTC disclaimer: This post may contains affiliate links and we will be compensated if you click on a link and make a purchase.
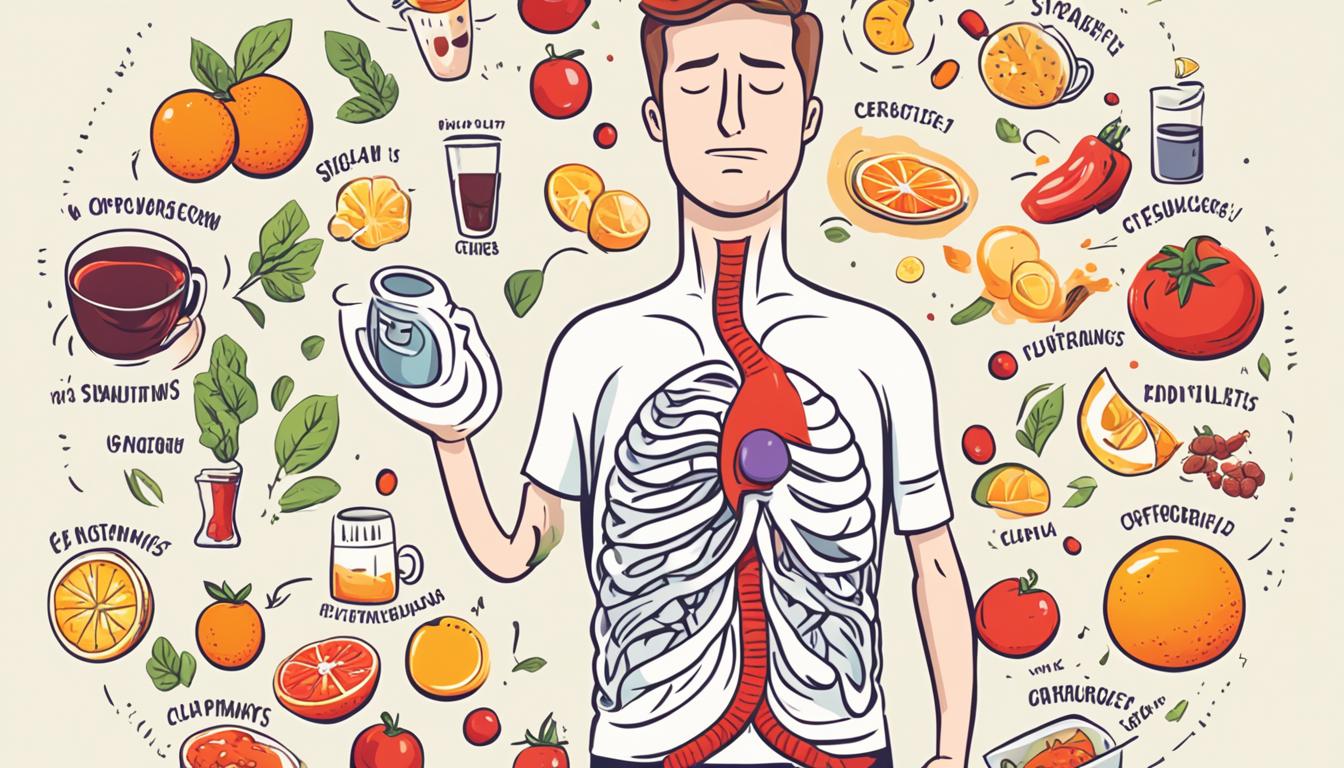
More than 60 million American adults get heartburn at least once a month. Over 15 million suffer from it every day. This common digestive issue is called acid reflux or gastroesophageal reflux disease (GERD). It happens when stomach acid goes back into the esophagus. This causes a burning feeling and other uncomfortable symptoms.
It’s important to know about the causes, symptoms, tests, and treatments for acid reflux. This knowledge helps manage this common health problem.
Key Takeaways
- Acid reflux is a common digestive condition where stomach acid flows back into the esophagus, causing symptoms like heartburn, regurgitation, and difficulty swallowing.
- Risk factors for acid reflux include obesity, pregnancy, certain foods and beverages, smoking, and the use of nonsteroidal anti-inflammatory drugs.
- Diagnostic tests for acid reflux may include endoscopy, pH monitoring, and esophageal manometry to evaluate the severity and underlying causes.
- Treatment options for acid reflux include lifestyle modifications, over-the-counter and prescription medications, and in severe cases, surgical interventions.
- Untreated acid reflux can lead to complications like esophageal inflammation, stricture, Barrett’s esophagus, and even esophageal cancer.
What is Acid Reflux?
Definition and Overview
Acid reflux, also known as gastroesophageal reflux (GER), happens when stomach acid goes back up into the esophagus. This happens when the muscle at the top of the stomach relaxes too much. It lets stomach acid flow back into the esophagus. This can make you feel a burning in your chest or throat, known as heartburn.
Having acid reflux more than twice a week might mean you have acid reflux disease, or GERD. About one in three people with GERD show signs on X-rays during a test. But only half of those with acid reflux have clear signs in their esophagus during an endoscopy.
If you have acid reflux symptoms more than twice a week, you should see a doctor. An endoscopy can check for diseases like esophageal cancer.
There are many ways to manage acid reflux, like taking certain medicines. If medicines don’t work, surgery might be an option.
Causes of Acid Reflux
Common Risk Factors
Acid reflux, also known as gastroesophageal reflux disease (GERD), has many causes. A hiatal hernia is one common cause. It happens when the stomach and the lower esophageal sphincter (LES) move up above the diaphragm. This makes it easier for acid to flow back into the esophagus.
Pregnancy is another big risk factor for acid reflux, especially in the third trimester. The growing fetus puts pressure on the stomach. Smoking can also raise the risk by harming the mucus membranes and muscle reflexes in the throat. It increases acid secretion and reduces the LES muscle function and salivation.
Being overweight or obese is a common cause of acid reflux. Some medicines, like aspirin and ibuprofen, can also cause acid reflux. They relax the LES.
Diet and lifestyle can also increase acid reflux risk. Eating big meals and lying down after can do it. Snacking before bed and eating trigger foods like alcohol and citrus fruits can also raise the risk.
https://www.youtube.com/watch?v=zh-9RaSCMxQ
“Approximately 20% of the population suffers from gastroesophageal reflux disease (GERD), a chronic acid reflux condition.”
Other causes of acid reflux include congenital defects and connective tissue diseases. Prior surgery in the chest or upper abdomen can also cause it. Knowing these risk factors can help people manage their acid reflux.
Symptoms of Acid Reflux
Acid reflux, also known as heartburn, affects millions worldwide. It can be treated at home sometimes, but not always. If it happens often or lasts a long time, it might be GERD. The main signs are a burning feeling in the chest or throat, bringing up stomach contents, and tasting sour in your mouth.
Other signs include bloating, trouble swallowing, feeling sick, wheezing, and a sore throat. These get worse at night or after eating certain foods like citrus fruits, chocolate, caffeine, and fried or fatty foods. Being overweight, eating too much, and smoking can make it worse.
Acid reflux can turn into GERD, a serious condition. This can cause scar tissue in the esophagus, ulcers, or even changes that could lead to cancer. Having heartburn two or more times a week is a sign of GERD.
Acid Reflux Symptoms | Frequency |
|---|---|
Heartburn | Occasional to frequent (2+ times per week) |
Regurgitation | Occasional to frequent |
Bloating | Occasional to frequent |
Dysphagia (difficulty swallowing) | Occasional to frequent |
Nausea | Occasional to frequent |
Wheezing | Occasional to frequent |
Sore Throat | Chronic |
If acid reflux doesn’t go away or is very bad, see a doctor. They can figure out why and suggest how to fix it. This might mean changing what you eat, taking medicine, or surgery in some cases.
“Acid reflux is common, but seeing a doctor is key if it’s ongoing or bad. Not getting help can lead to bigger health problems.”
Getting acid reflux checked early and treated can stop serious health issues. It also makes life better.
Acid Reflux in Babies
Acid reflux, also known as gastroesophageal reflux (GER), is common in infants. Babies often spit up after feeding as their digestive system grows. But, some have a severe form called gastroesophageal reflux disease (GERD), which makes them uncomfortable and makes feeding hard.
Symptoms of GERD in babies include being very fussy, not sleeping well, not wanting to eat, vomiting a lot, wheezing, and bad breath. Babies born too soon or with esophageal problems are more likely to have GERD.
- Reflux is normal in healthy babies but less common as they get older.
- It’s rare in babies after 18 months.
- Things like lying flat and drinking mostly liquids can cause reflux in babies.
- Reflux is more common in premature babies or those with lung or nervous system issues.
- Most reflux cases don’t cause problems, but GERD might make babies grow slower.
- Babies who spit up a lot may be more likely to have GERD later.
About 50% of babies up to 3 months old spit up often. By 4 months, 66% of babies spit up daily. By 7 months, only 14% spit up often, and less than 5% by 10 to 14 months.
Most babies have GERD in their first year, which is normal. The exact number of babies with GERD is unknown because symptoms can mean different things. Babies with certain health issues are more likely to have GERD.
Reflux is very common in babies, with half spitting up often in the first 3 months. Babies usually stop spitting up by 12 to 14 months. GERD is common in young babies, but by their first birthday, only 10% still have it.
Changes in feeding can help with reflux or GERD, like adding rice cereal to the bottle and burping the baby. Medicines like H2 blockers and PPIs can also help. Surgery is only for babies with severe GERD who don’t get better with other treatments.

Diagnosing Acid Reflux
Tests and Procedures
If you have ongoing acid reflux symptoms, your doctor might suggest tests to confirm the issue and find the cause. These tests check for any problems, inflammation, or damage in the esophagus. They also track how often and how bad your acid reflux is.
A barium swallow X-ray is a common test. You drink a thick liquid called barium. It coats your esophagus and stomach, showing any issues or blockages on X-ray.
An upper endoscopy lets a thin tube with a camera look at your esophagus, stomach, and small intestine’s start. It spots inflammation, ulcers, or damage in the esophagus lining.
A biopsy might be suggested next. It takes a small tissue sample from your esophagus for lab tests. This can spot conditions like Barrett’s esophagus, which is a precancerous change.
Esophageal manometry checks the esophagus muscles’ pressure and function. It finds problems with muscles that help you swallow and the opening between your esophagus and stomach.
Impedance monitoring and pH testing track your acid reflux over 24 hours. They use a small device in your esophagus to measure acid and non-acid reflux events.
Often, acid reflux is diagnosed by symptoms and how you react to changes in lifestyle or medicine. But tests give your doctor more details. This helps them make the best treatment plan for you.
Acid Reflux Medications
If you’re feeling the pain of acid reflux, you can find quick relief with over-the-counter (OTC) meds. Antacids like Alka-Seltzer, Maalox, and Rolaids work by balancing out stomach acid. H2 blockers, such as Pepcid and Tagamet, cut down on acid making.
For better and longer relief, proton pump inhibitors (PPIs) like Nexium, Prilosec, and Prevacid are stronger acid stoppers that help heal the esophagus.
Stronger PPIs, like esomeprazole, lansoprazole, and omeprazole, might cause side effects like diarrhea or headaches. But they block acid better. Prokinetic drugs like Reglan and Urecholine can be given to make the lower esophageal sphincter (LES) stronger and help food move out of the stomach, reducing acid reflux.
OTC meds can help fast, but they might not heal an inflamed esophagus. Prescription PPIs are often the best choice because they let damaged esophageal tissue heal.
Medication Type | Examples | Key Features |
|---|---|---|
Antacids | Alka-Seltzer, Maalox, Rolaids | Neutralize stomach acid |
H2 Blockers | Pepcid, Tagamet | Reduce acid production |
Proton Pump Inhibitors (PPIs) | Nexium, Prilosec, Prevacid | Most effective in blocking acid secretion and allowing esophageal healing |
Prokinetics | Reglan, Urecholine | Strengthen the LES and improve stomach emptying |
Always talk to a healthcare professional before taking any new meds or supplements, as they can make acid reflux worse. They can help you find the best way to manage your acid reflux.
Surgical Treatment for Acid Reflux
Fundoplication and LINX Device
If lifestyle changes and medicines don’t work for acid reflux, surgery might be an option. Fundoplication is a common surgery for this. It wraps the stomach’s top around the lower esophageal sphincter (LES) to stop acid from flowing back up. This surgery is done through small cuts in the belly, using a minimally invasive method.
The LINX® Reflux Management System is another choice. It puts magnetic beads around the esophagus to keep the LES closed. This method is less invasive, with smaller cuts. Transoral incisionless fundoplication (TIF) is a newer, even less invasive way to treat GERD.
Laparoscopic fundoplication is usually done as an outpatient surgery, taking about an hour and a half. Most people don’t need more medicine after this surgery, feeling better within a week. Studies on the LINX® System show most patients have no GERD symptoms and don’t need medicine for five years after surgery.
Before surgery, tests like upper endoscopy, 24-hour pH test, and esophageal manometry are done. These tests help pick the best surgery for each patient.
Surgery can greatly help with GERD, but some might still need medicine or have new symptoms. It’s important to follow up with a doctor for the best results.
Lifestyle Changes for Acid Reflux
If you’re dealing with acid reflux, making some lifestyle changes can help. By avoiding common triggers and choosing healthier habits, you can ease your symptoms. This can help prevent the discomfort of gastroesophageal reflux disease (GERD).
Keeping a healthy weight is key. Being overweight puts extra pressure on your stomach, making acid flow back up. Studies show losing weight can help many people with GERD. Eating smaller meals and not lying down after eating can also ease stomach pressure.
Stopping smoking is vital. Nicotine weakens the muscle that keeps stomach acid down. Also, raising your bed by 6-8 inches can stop acid reflux by using gravity.
Knowing and avoiding trigger foods is key. Foods like coffee, tea, and spicy foods can cause reflux. Also, alcohol, especially white wine and beer, can make it worse. Watching what you eat can help reduce your reflux.
Living a healthy life, like managing your weight, quitting smoking, and avoiding trigger foods, can help with acid reflux. Simple changes can make a big difference in your health.

Lifestyle Change | Potential Benefits for Acid Reflux |
|---|---|
Weight loss | Reduces pressure on the stomach, preventing acid from flowing back into the esophagus. |
Quitting smoking | Strengthens the valve between the stomach and esophagus, reducing reflux episodes. |
Elevating the head of the bed | Uses gravity to keep stomach contents down, preventing acid from flowing back up. |
Avoiding trigger foods | Eliminates common culprits that can aggravate reflux, such as coffee, alcohol, and spicy/fatty foods. |
“Maintaining a healthy weight, eating smaller meals, and wearing loose-fitting clothes can help reduce pressure on the stomach and GERD-related symptoms.”
By changing your lifestyle, you can take charge of your acid reflux. These changes can improve your life a lot.
Complications of Untreated Acid Reflux
Untreated acid reflux can lead to serious health issues. About 5% to 10% of people with GERD get a precancerous condition called Barrett’s esophagus. This condition slightly increases the risk of esophageal cancer.
GERD can cause inflammation of the esophagus, known as esophagitis. This can lead to Barrett’s esophagus. Untreated GERD may also cause esophageal strictures, making swallowing hard and painful.
Laryngopharyngeal reflux (LPR) is another issue from acid reflux. It happens when stomach acid goes up to the throat and voice box. Symptoms include hoarseness, chronic cough, and trouble swallowing. LPR can also cause asthma or make asthma worse.
Complication | Potential Impact |
|---|---|
Esophagitis | Inflammation of the esophagus, leading to further damage and increased risk of other complications |
Barrett’s Esophagus | Precancerous changes in the esophageal lining, raising the risk of esophageal cancer |
Esophageal Stricture | Narrowing of the esophagus, making swallowing difficult and painful |
Laryngopharyngeal Reflux | Stomach acid reaching the throat, causing hoarseness, chronic cough, and difficulty swallowing |
Esophageal Cancer | A serious and potentially life-threatening condition that can develop from untreated acid reflux and its complications |
Untreated acid reflux can cause serious health problems. These include esophagitis, Barrett’s esophagus, esophageal strictures, LPR, and a higher risk of esophageal cancer. It’s important to get medical help and make lifestyle changes to avoid these issues.
Acid Reflux During Pregnancy
Acid reflux, also known as gastroesophageal reflux disease (GERD), affects up to 80% of pregnant women. Hormones and the growing fetus put pressure on the stomach, relaxing the lower esophageal sphincter. This lets stomach acid flow back up. Expectant moms may feel heartburn, regurgitation, and other symptoms, especially later in pregnancy.
Symptoms include a burning sensation in the chest, feeling full, heavy, or bloated, and burping or belching. These symptoms start from 12 weeks of pregnancy. Hormones and the growing uterus relax the lower esophageal sphincter, causing stomach acids to flow back up.
To manage acid reflux, eat small meals, avoid spicy or fatty foods, and don’t lie down after eating. Sleeping with your head elevated and wearing loose clothes can also help. Your doctor may suggest OTC medications like antacids or proton pump inhibitors, but check with them first.
Acid reflux usually goes away after giving birth. Regular visits to your doctor can help manage any health issues, including acid reflux, during pregnancy.

Symptom | Cause | Management |
|---|---|---|
Heartburn, regurgitation, bloating, burping, feeling or being sick | Hormonal changes, increased pressure on the stomach from the growing fetus | Dietary changes (small meals, avoiding spicy/fatty foods), elevating the head during sleep, OTC medications (antacids, H2 blockers, proton pump inhibitors) |
Acid reflux is common and can be managed during pregnancy. Understanding its causes, symptoms, and how to manage it can make pregnancy more comfortable.
“Acid reflux during pregnancy can be a frustrating experience, but with the right strategies, it can be managed effectively. The key is to work closely with your healthcare provider to find the best solution for your individual needs.”
Acid Reflux and Asthma
The link between acid reflux and asthma is well-known. Up to 80% of people with asthma also have gastroesophageal reflux disease (GERD). This means acid reflux can make asthma worse, and asthma can make acid reflux worse too.
Acid reflux can make airways swell and contract. This can cause coughing, wheezing, and shortness of breath, which are asthma symptoms. Long-term heartburn might be a sign of silent GERD, which can affect asthma. Doctors use tests like laryngoscopy and endoscopy to check for GERD in asthma patients.
Some asthma medicines can make acid reflux worse. So, treating GERD is important for better asthma control. Doctors often prescribe antacids, H2 blockers, or proton-pump inhibitors for GERD. In some cases, surgery might be needed.
Changing your diet, losing weight, and avoiding certain foods can help manage GERD and asthma. Also, sleeping with the head raised, not eating before bed, and quitting smoking can prevent acid reflux.
If you think your asthma and acid reflux are connected, talk to a doctor. They can create a plan just for you to manage both conditions.
Key Findings | Details |
|---|---|
Association between Asthma and Heartburn | Individuals with asthma are more likely to experience heartburn. |
Two-way Relationship | The connection between asthma and heartburn is bidirectional. |
Impact on Asthma Symptoms | Frequent heartburn can make asthma symptoms worse. |
Acid Reflux as a Trigger | Acid reflux can trigger or worsen asthma symptoms. |
Prevalence of GERD | Long-term heartburn could indicate gastroesophageal reflux disease (GERD). |
Signs of Silent GERD | Certain signs suggest silent GERD in asthma patients. |
Diagnostic Tests for GERD | Tests like laryngoscopy and endoscopy can diagnose GERD in asthma patients. |
Medications and Acid Reflux | Certain asthma drugs may increase acid reflux risk. |
Management Approach | Controlling GERD symptoms is key to improving asthma symptoms. |
Medication for GERD | Antacids, H2 blockers, and proton-pump inhibitors are used for GERD treatment. |
Surgical Intervention | Surgery may be recommended for treating GERD in some cases. |
Lifestyle Changes | Recommendations include dietary changes, weight loss, and lifestyle adjustments. |
Impact of Gravity | Raising the head of the bed can prevent stomach acid reflux. |
Behavioral Modifications | Avoiding eating before bedtime and avoiding trigger foods can help. |
Smoking Cessation | Quitting smoking is advised to reduce GERD symptoms. |
Clothing Choice | Wearing loose clothes and avoiding belts can help manage GERD. |
Individualized Approach | Tailoring treatment to specific triggers and symptoms is key for managing asthma and GERD. |
In summary, the link between acid reflux and asthma is complex. Managing GERD symptoms is crucial for better asthma control. A mix of medication, lifestyle changes, and personalized care can help with this condition.
“Controlling GERD symptoms is key to improving asthma symptoms.”
Acid Reflux Management Strategies
Dietary and Lifestyle Adjustments
Managing acid reflux and GERD means changing your diet and lifestyle. You might also need medicine or surgery. These changes can lessen how often and how bad the reflux is. They can also stop serious problems from happening.
Keeping a healthy weight is key to managing acid reflux. Being overweight, especially around the stomach, can make heartburn worse. Just losing a few pounds can help a lot with GERD symptoms.
What you eat matters too. Stay away from spicy, fried, or acidic foods that can make reflux worse. Eating low-fat, high-protein foods is better. Chewing gum after meals can also help by making more saliva to neutralize stomach acid.
Eating smaller meals often and not lying down after eating can also help. Sleeping with your head raised can stop stomach acid from flowing back up.
Stopping smoking and wearing loose clothes can also ease GERD symptoms. Stress-reducing activities like yoga, meditation, and deep breathing can also help.
For severe acid reflux, you might need prescription drugs to protect your esophagus. In some cases, surgery like fundoplication or the LINX device might be needed if other treatments don’t work.

“Effective management of acid reflux often involves a combination of dietary and lifestyle adjustments, in addition to any necessary medical treatments.”
Recommended Strategies | Benefits |
|---|---|
Maintain a healthy weight | Reduces pressure on the stomach and lowers the risk of acid reflux |
Avoid trigger foods and drinks | Certain items can increase the risk of reflux episodes |
Eat smaller, more frequent meals | Reduces the amount of food in the stomach, which can help prevent reflux |
Elevate the head of the bed | Prevents stomach contents from flowing back into the esophagus during sleep |
Quit smoking and avoid tight clothing | These factors can exacerbate GERD symptoms |
By making these changes, people with acid reflux or GERD can better manage their symptoms. But for serious or ongoing acid reflux, you might need doctor-prescribed treatments or surgery.
Conclusion
Acid reflux is a common issue where stomach acid goes back up into the esophagus. This can cause heartburn, regurgitation, and trouble swallowing. About 20% of Americans deal with this condition all the time.
Things like a weak lower esophageal sphincter, hiatal hernia, pregnancy, being overweight, and some medicines can make acid reflux worse.
Medicines can help, but changing your diet, managing your weight, and how you sleep is also key. It usually takes a month to fix the damage from acid reflux with the right treatment. If not treated, acid reflux can cause serious problems. So, it’s important to work with a doctor to find the right treatment.
Learning about acid reflux, its causes, and how to treat it can help you manage it better. This summary of acid reflux info can be a useful guide. It can help you live a healthier, more comfortable life.
FAQ
What is acid reflux and how does it occur?
Acid reflux, also known as gastroesophageal reflux (GER), happens when stomach acid goes back up into the esophagus. This happens when the muscle at the bottom of the esophagus doesn’t work right. It lets stomach contents flow back into the esophagus.
What are the common causes and risk factors for acid reflux?
Many things can make acid reflux and GERD worse. These include a hiatal hernia, being pregnant, being overweight, smoking, and some medicines. Other causes are birth defects, diseases of the connective tissue, and surgery in the chest or upper belly.
What are the symptoms of acid reflux?
Symptoms of acid reflux include heartburn and a burning feeling in the chest or throat. You might also feel like stomach contents come back up into your mouth or throat. Other signs are bloating, trouble swallowing, nausea, wheezing, and a sore throat that doesn’t heal.
How is acid reflux diagnosed?
Doctors might use tests to find out if you have acid reflux or GERD. These tests include a barium swallow, upper endoscopy, biopsy, esophageal manometry, impedance monitoring, and pH monitoring. These help see if there are any problems, check for damage, and see how often and how bad the acid reflux is.
What are the treatment options for acid reflux?
There are many ways to treat acid reflux, like over-the-counter and prescription medicines. These can be antacids, H2 blockers, or proton pump inhibitors. If these don’t work, surgery like fundoplication or the LINX device might be an option.
How can acid reflux be managed through lifestyle changes?
Changing your lifestyle can help with acid reflux. This means keeping a healthy weight, quitting smoking, and sleeping with your head raised. Avoid foods like citrus, tomatoes, chocolate, mint, garlic, onions, and spicy or fatty foods. Eat smaller meals and don’t lie down right after eating.
What are the potential complications of untreated acid reflux?
If acid reflux is not treated, it can cause serious problems. These include inflammation of the esophagus, changes that could lead to cancer, narrowing of the esophagus, and problems with breathing. It can also increase the risk of esophageal cancer.
How does acid reflux affect babies and infants?
Babies sometimes spit up after feeding, which can include some stomach acid. However, some babies have a more serious issue called GERD. This can make them very uncomfortable and make feeding hard.
Signs of GERD in babies include being very fussy, not sleeping well, not wanting to eat, vomiting a lot, wheezing, and bad breath.
Is there a connection between acid reflux and asthma?
Yes, acid reflux and asthma are closely linked. Up to 80% of people with asthma also have GERD. Acid reflux can make asthma symptoms worse by irritating the airways. Also, asthma attacks can make acid reflux worse by putting pressure on the chest.